Bronstein AC et al: 2011 Annual report of the America Association of Poison Control Centers’ National Poison Data System (NPDS): 29th Annual Report. Clin Toxicol (Phila) 2011;50:911–1164 [PMID: 23272763].
PHARMACOLOGIC PRINCIPLES OF TOXICOLOGY
In the evaluation of the poisoned patient, it is important to compare the anticipated pharmacologic or toxic effects with the patient’s clinical presentation. If the history is that the patient ingested a tranquilizer 30 minutes ago, but the clinical examination reveals dilated pupils, tachycardia, dry mouth, absent bowel sounds, and active hallucinations—clearly anticholinergic toxicity—diagnosis and therapy should proceed accordingly. In addition, standard pharmacokinetics (absorption, distribution, metabolism, and elimination) often cannot be applied in the setting of a supratherapeutic exposure, since these parameters are extrapolated from healthy volunteers receiving therapeutic doses.
LD50
Estimates of the LD50 (the amount per kilogram of body weight of a drug required to kill 50% of a group of experimental animals) or median lethal dose are of little clinical value in humans. It is usually impossible to determine with accuracy the amount swallowed or absorbed, the metabolic status of the patient, or in which patients the response to the agent will be atypical. Furthermore, these values are often not valid in humans even if the history is accurate.
Absorption
Absorption is how the substance enters the body. Depending on the route, absorption times can vary in general, intravenous/intra-arterial > inhalation > sublingual > intramuscular > subcutaneous > intranasal > oral > rectal > dermal. Large overdoses, hypotension, decreased gut mobility are factors that can delay absorption.
Elimination Half-Life
The t1/2 of an agent must be interpreted carefully. Most published t1/2 values are for therapeutic dosages. The t1/2 may increase as the quantity of the ingested substance increases for many common intoxicants such as salicylates. One cannot rely on the published t1/2 for salicylate (2 hours) to assume rapid elimination of the drug. In an acute salicylate overdose (150 mg/kg), the apparent t1/2 is prolonged to 24–30 hours.
Volume of Distribution
The volume of distribution (Vd) of a drug is determined by dividing the amount of drug absorbed by the blood level. With theophylline, for example, the Vd is 0.46 L/kg body weight, or 32 L in an average adult. In contrast, digoxin distributes well beyond total body water. Because the calculation produces a volume above body weight, this figure is referred to as an “apparent volume of distribution.”
Body Burden
Using the pharmacokinetic principles permits a practical determination of the absorbed dose and permits an understanding of the patient’s status as to whether a therapeutic administration or an overdose has occurred. A 20-kg child with an acetaminophen blood level reported as 200 mcg/mL (equivalent to 200 mg/L) would have a body burden of 4000 mg of acetaminophen. This is ascertained by taking the volume of distribution of 1 L times the weight of the child times the blood level in milligram per liter. This would be consistent with an overdose history of having consumed eight extrastrength 500-mg tablets but would not be consistent with a history of therapeutic administration of 15 mg/kg for four doses. Such a therapeutic administration would have a maximum administered dose of 1200 mg (20 kg times 15 mg/kg times four doses), which is well under the calculated body burden. Given metabolism of the drug with a normal half-life of 2 hours, it is apparent that much of the first doses would have been metabolized further adding to an understanding that this must not have been a therapeutic dose. While patients who develop hepatic toxicity from acetaminophen might have a prolonged half-life later in the course, it would certainly not occur with early therapeutic doses.
Metabolism & Excretion
The route of excretion or detoxification is important for planning treatment. Methanol, for example, is metabolized to the toxic product, formic acid. This metabolic step may be blocked by the antidote fomepizole or ethanol and patients with renal failure may not eliminate methanol as readily.
Blood Levels
Care of the poisoned patient should never be guided solely by laboratory measurements. Concentration results may not return in time to influence acute management. Initial treatment should be directed at symptomatic and supportive care, guided by the clinical presentation, followed by more specific therapy based on laboratory determinations. Clinical information may speed the identification of a toxic agent by the laboratory.
PREVENTING CHILDHOOD POISONINGS
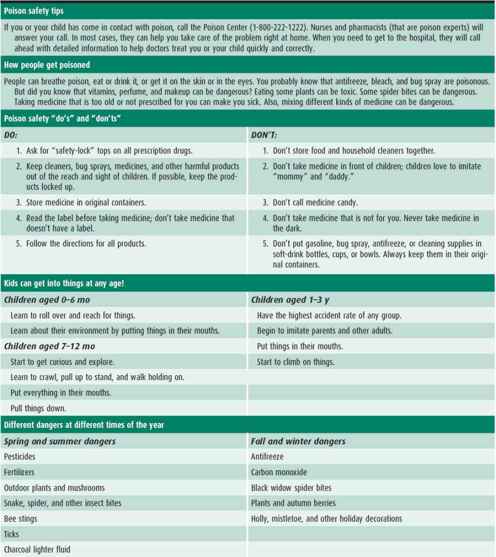
Inclusion of poison prevention as part of routine well-child care should begin at the 6-month well-baby visit. The poison prevention handout included as Table 13–1 may be copied and distributed to parents. It contains poison prevention information as well as first-aid actions that should be taken in the event of an exposure. All poison control centers in the United States can be reached by dialing 1-800-222-1222; the call will be automatically routed to the correct regional center.
Table 13–1. Poison prevention and emergency treatment handout.
GENERAL TREATMENT OF POISONING
The telephone is often the first contact in pediatric poisoning. Some patients may contact their pediatrician’s office first. Proper telephone management can reduce morbidity and prevent unwarranted or excessive treatment. The decision to refer the patient is based on the identity and dose of the ingested agent, the age of the child, the time of day, the reliability of the parent, and whether child neglect or endangerment is suspected. Poison control centers are the source of expert telephone advice and have excellent follow-up programs to manage patients in the home as well as provide further poison prevention information.
INITIAL TELEPHONE CONTACT
Basic information obtained at the first telephone contact includes the patient’s name, age, weight, address, and telephone number; the agent and amount of agent ingested; the patient’s present condition; and the time elapsed since ingestion or other exposure. Use the history to evaluate the urgency of the situation and decide whether immediate emergency transportation to a health facility is indicated. An emergency exists if the ingestant is high risk (caustic solutions, hydrogen fluoride, drugs of abuse, or medications such as a calcium channel blocker, opioid, hypoglycemic agent, or antidepressant) or if the self-poisoning was intentional. If immediate danger does not exist, obtain more details about the suspected toxic agent. If the child requires transport to a health facility, instruct parents that everything in the vicinity of the child that may be a cause of poisoning should be brought to the healthcare facility.
It may be difficult to obtain an accurate history. Obtain names of drugs or ingredients, manufacturers, prescription numbers, names and phone numbers of prescribing physician and pharmacy, and any other pertinent information. Find out whether the substance was shared among several children, whether it had been recently purchased, who had last used it, how full the bottle was, and how much was spilled. Determine if this occurred in the home, school, or elsewhere. If unsure of the significance of an exposure, consult with a poison control center.
Each year, children are accidentally poisoned by medicines, polishes, insecticides, drain cleaners, bleaches, household chemicals, and materials commonly stored in the garage. It is the responsibility of adults to make sure that children are not exposed to potentially toxic substances.
Obtaining Information About Poisons
Current data on ingredients of commercial products and medications can be obtained from a certified regional poison center. It is important to have the actual container at hand when calling. Material safety data sheets (MSDS) are helpful in providing product ingredient and concentration information. Caution: Antidote information on labels of commercial products or in the Physicians’ Desk Reference may be incorrect or inappropriate.
Follow-Up
In over 95% of cases of ingestion of potentially toxic substances by children, a trip to the hospital is not required. In these cases, it is important to call the parent at 1 and 4 hours after ingestion. If the child has ingested an additional unknown agent and develops symptoms, a change in management may be needed, including transportation to the hospital. An additional call should be made 24 hours after the ingestion to begin the process of poison prevention.
INITIAL EMERGENCY DEPARTMENT CONTACT
Make Certain the Patient Is Breathing
As in all emergencies, the principles of treatment are attention to Pediatric Advance Life Support algorithms in resuscitation: airway, breathing, and circulation. These are sometimes overlooked under the stressful conditions of a pediatric poisoning.
Treat Shock
Initial therapy of the hypotensive patient should consist of laying the patient flat or head down and administering intravenous (IV) isotonic solutions. Vasopressors should be reserved for poisoned patients in shock who do not respond to these standard measures.
Treat Burns & Skin Exposures
Burns may occur following exposure to strongly acidic or strongly alkaline agents or petroleum distillates. Burned areas should be decontaminated by flooding with sterile saline solution or water. A burn unit should be consulted if more than minimal burn damage has been sustained. Skin decontamination should be performed in a patient with cutaneous exposure. Emergency department personnel in contact with a patient who has been contaminated (with an organophosphate insecticide, for example) should themselves be decontaminated if their skin or clothing becomes contaminated. Ocular exposures can initially be decontaminated at home by placing the child in the shower allowing the water to indirectly flow from the top of the head into the eyes. Otherwise, irrigation with assessment of pH should be performed in the emergency department.
Take a Pertinent History
The history should be taken from the parents and all individuals present at the scene. It may be crucial to determine all of the kinds of poisons in the home.
These may include drugs used by family members and their medical histories, dietary or herbal supplements, foreign medications, chemicals associated with the hobbies or occupations of family members, or the purity of the water supply.
DEFINITIVE THERAPY OF POISONING
Treatment of poisoning or potential poisoning has evolved over time, and general measures such as prevention of absorption and enhancement of excretion are only instituted when specifically indicated. Specific therapy is directed at each drug, chemical, or toxin as described in the management section that follows.
Prevention of Absorption
A. Emesis and Lavage
These measures are rarely used in pediatric patients and have their own associated risk. They should not be used routinely in the management of poisonings except in potential lethal exposures with poor treatment options, such as a large tricyclic antidepressant overdose. They should be performed only in consultation with a poison center.
B. Charcoal
The routine use of charcoal has decreased substantially in recent years, especially in unintentional pediatric ingestions where lick, sip, taste ingestions are rarely dangerous. Charcoal can be considered in patients who are awake, alert, and able to drink it voluntarily. It should never be given to patients with altered sensorium who are unable to protect their airway due to risk of aspiration. The dose of charcoal is 1–2 g/kg (maximum, 100 g) per dose. Repeating the dose of activated charcoal may be useful for those agents that slow passage through the gastrointestinal (GI) tract. When multiple doses of activated charcoal are given, repeated doses of sorbitol or saline cathartics must not be given. Repeated doses of cathartics may cause electrolyte imbalances and fluid loss. Charcoal dosing is repeated every 2–6 hours until charcoal is passed through the rectum. It is not useful in ingestions of heavy metals, and may be harmful in hydrocarbons, caustics, and solvent ingestions.
C. Catharsis
Cathartics do not improve outcome and should be avoided.
D. Whole Gut Lavage
Whole bowel lavage uses an orally administered, nonabsorbable hypertonic solution such as CoLyte or GoLYTELY. The use of this procedure in poisoned patients remains controversial. Preliminary recommendations for use of whole bowel irrigation include poisoning with sustained-release preparations, mechanical movement of items through the bowel (eg, cocaine packets, iron tablets), and poisoning with substances that are poorly absorbed by charcoal (eg, lithium, iron). Underlying bowel pathology and intestinal obstruction are relative contraindications to its use. Consultation with a certified regional poison center is recommended.
American Academy of Clinical Toxicology, European Association of Poisons Centers and Clinical Toxicologists: Position statement and practice guidelines on the use of multidose activated charcoal in the treatment of acute poisoning. J Toxicol Clin Toxicol 1999;37:731 [PMID: 10584586].
Benson et al: Poison paper update: gastric lavage. Clin Toxicol 2013 Mar;51(3):140–6.
Chyka PA et al: Position paper: single-dose activated charcoal. American Academy of Clinical Toxicology; European Association of Poison Centres and Clinical Toxicologists. Clin Toxicol (Phila) 2005;43:61 [PMID: 15822758].
Gielen AC et al: Effects of improved access to safety counseling, products, and home visits on parents’ safety practices: results of a randomized trial. Arch Pediatr Adolesc Med 2002;156:33 [PMID: 11772188].
Hojer et al: Poisition paper update: ipecac syrup. Clin Toxicol 2013 Mar;15(3):134–9.
Thummel KE, Shen DD: Design and optimization of dosage regimens: pharmacokinetic data. In Goodman LS et al (eds): Goodman & Gilman’s The Pharmacological Basis of Therapeutics. McGraw-Hill; 2001;1917.
Enhancement of Excretion
Excretion of certain substances can be hastened by urinary alkalinization or dialysis and is reserved for very special circumstances. It is important to make certain that the patient is not volume depleted. Volume-depleted patients should receive a normal saline bolus of 10–20 mL/kg, followed by sufficient IV fluid administration to maintain urine output at 2–3 mL/kg/h.
A. Urinary Alkalinization
1. Alkaline diuresis—Urinary alkalinization should be chosen on the basis of the substance’s p Ka, so that ionized drug will be trapped in the tubular lumen and not reabsorbed (see Table 13–1). Thus, if the pKa is less than 7.5, urinary alkalinization is appropriate; if it is over 8.0, this technique is not usually beneficial. The pKa is sometimes included along with general drug information. Urinary alkalinization is achieved with sodium bicarbonate. It is important to observe for hypokalemia, caused by the shift of potassium intracellularly. Follow serum K+ and observe for electrocardiogram (ECG) evidence of hypokalemia. If complications such as renal failure or pulmonary edema are present, hemodialysis or hemoperfusion may be required. It is most commonly used for the treatment of salicylate toxicity and to prevent methotrexate toxicity.
B. Dialysis
Hemodialysis is useful in the treatment of some poisons and in the general management of a critically ill patient. Although peritoneal dialysis can enhance elimination of a few medications, it is typically too slow to be clinically useful. Continuous hemofiltration techniques may be used when hypotensive patients may not tolerate traditional hemodialysis; however, clearance rates may also be slower. Dialysis should be considered part of supportive care if the patient satisfies any of the following criteria:
1. Clinical criteria
A. Potentially life-threatening toxicity that is caused by a dialyzable drug and cannot be treated by conservative means.
B. Hypotension threatening renal or hepatic function that cannot be corrected by adjusting circulating volume.
C. Marked hyperosmolality or severe acid-base or electrolyte disturbances not responding to therapy.
D. Marked hypothermia or hyperthermia not responding to therapy.
2. Immediate dialysis—Immediate dialysis should be considered in ethylene glycol and methanol poisoning only if acidosis is refractory, the patient does not respond to fomepizole treatment, or blood levels of ethanol of 100 mg/dL are consistently maintained. Refractory salicylate intoxication may benefit from dialysis.
MANAGEMENT OF SPECIFIC COMMON POISONINGS
ACETAMINOPHEN (PARACETAMOL)
Overdosage of acetaminophen is the most common pediatric poisoning and can produce severe hepatotoxicity. The incidence of hepatotoxicity in adults and adolescents has been reported to be 10 times higher than in children younger than age 5 years. In the latter group, fewer than 0.1% develop hepatotoxicity after acetaminophen overdose. In children, toxicity most commonly results from repeated overdosage arising from confusion about the age-appropriate dose, use of multiple products that contain acetaminophen, or use of adult suppositories.
Acetaminophen is normally metabolized in the liver. A small percentage of the drug goes through a pathway leading to a toxic metabolite. Normally, this electrophilic reactant is removed harmlessly by conjugation with glutathione. In overdosage, the supply of glutathione becomes exhausted, and the metabolite may bind covalently to components of liver cells to produce necrosis. Some authors have proposed that therapeutic doses of acetaminophen may be toxic to children with depleted glutathione stores. However, there is no evidence that administration of therapeutic doses can cause toxicity, and only a few inadequate case reports have been made in this regard.
 Treatment
Treatment
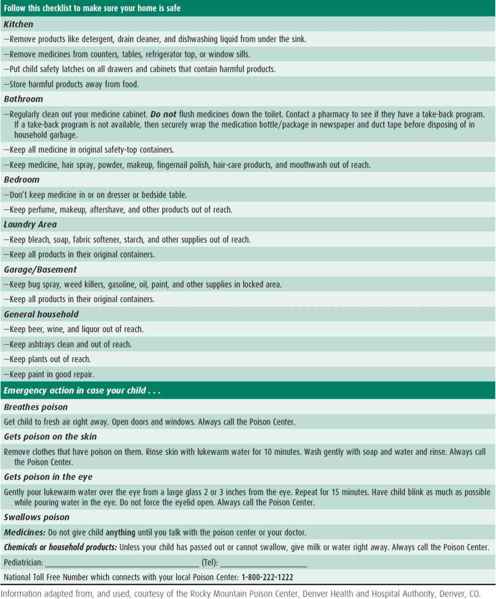
Treatment is to administer acetylcysteine. It may be administered either orally or intravenously. Consultation on difficult cases may be obtained from your regional poison control center or the Rocky Mountain Poison and Drug Center (1-800-525-6115). Blood levels should be obtained 4 hours after ingestion or as soon as possible thereafter and plotted on Figure 13–1. The nomogram is used only for acute ingestion, not repeated supratherapeutic ingestions. If the patient has ingested acetaminophen in a liquid preparation, blood levels obtained 2 hours after ingestion will accurately reflect the toxicity to be expected relative to the standard nomogram (see Figure 13–1). Acetylcysteine is administered to patients whose acetaminophen levels plot in the toxic range on the nomogram. Acetylcysteine is effective even when given more than 24 hours after ingestion, although it is most effective when given within 8 hours postingestion.
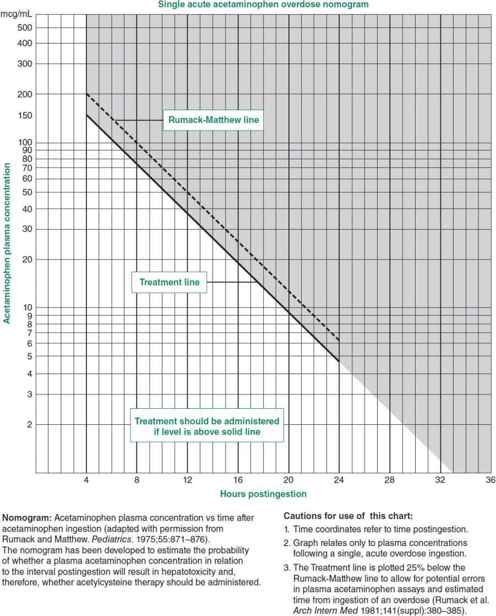
 Figure 13–1. Semi-logarithmic plot of plasma acetaminophen levels versus time. (Modified and reproduced, with permission, from Rumack BH, Matthew H: Acetaminophen poisoning and toxicity. Pediatrics 1975;55:871.)
Figure 13–1. Semi-logarithmic plot of plasma acetaminophen levels versus time. (Modified and reproduced, with permission, from Rumack BH, Matthew H: Acetaminophen poisoning and toxicity. Pediatrics 1975;55:871.)
For children weighing 40 kg or more, IV acetylcysteine (Acetadote) should be administered as a loading dose of 150 mg/kg administered over 15–60 min; followed by a second infusion of 50 mg/kg over 4 hours, and then a third infusion of 100 mg/kg over 16 hours.
For patients weighing less than 40 kg, IV acetylcysteine must have less dilution to avoid hyponatremia (a dosage calculator is available at http://www.acetadote.com) (Table 13–2). Patient-tailored therapy is critical when utilizing the IV “20-hour” protocol and those patients who still have acetaminophen measurable and/or elevated aspartate transaminase/alanine transaminase (AST/ALT) may need treatment beyond the 20 hours called for in the product insert.
Table 13–2. Intravenous acetylcysteine administration dosing.
The oral (PO) dose of acetylcysteine is 140 mg/kg, diluted to a 5% solution in sweet fruit juice or carbonated soft drink. The primary problems associated with administration are nausea and vomiting. After this loading dose, 70 mg/kg should be administered orally every 4 hours for 72 hours. AST–serum glutamic oxaloacetic transaminase (AST–SGOT), ALT–serum glutamic pyruvic transaminase (ALT–SGPT), serum bilirubin, and plasma prothrombin time should be followed daily. Significant abnormalities of liver function may not peak until 72–96 hours after ingestion.
Repeated miscalculated overdoses given by parents to treat fever are the major source of toxicity in children younger than age 10 years, and parents are often unaware of the significance of symptoms of toxicity, thus delaying its prompt recognition and therapy.
Dart RC, Rumack BH: Patient-tailored acetylcysteine administration. Ann Emerg Med 2007;50:280–281 [PMID: 17418449].
Rumack BH: Acetaminophen hepatotoxicity: the first 35 years. J Toxicol Clin Toxicol 2002;40:3 [PMID: 11990202].
Yarema MC et al: Comparison of the 20-hour intravenous and 72-hour oral acetylcysteine protocols for the treatment of acute acetaminophen poisoning. Ann Emerg Med 2009;54(4):606–614 [PMID: 19556028].
ALCOHOL, ETHYL (ETHANOL)
Alcoholic beverages, tinctures, cosmetics, mouthwashes, rubbing alcohol, and hand sanitizers are common sources of poisoning in children. Concomitant exposure to other depressant drugs increases the seriousness of the intoxication. In most states, alcohol levels of 50–80 mg/dL are considered compatible with impaired faculties, and levels of 80–100 mg/dL are considered evidence of intoxication. (Blood levels cited here are for adults; comparable figures for children are not available.)
Recent erroneous information regarding hand sanitizers has indicated that a “lick” following application on the hand could cause toxicity in children. In fact, this is not the case, but because these hand sanitizers contain 62% ethanol, toxicity following ingestion is very possible. Potential blood ethanol concentration following consumption of a 62% solution in a 10-kg child is calculated as follows:
1 oz = 30 mL × 62% = 18.6 mL of pure ethanol
18.6 mL × 0.79 (the specific gravity) = 14.7 g of ethanol, or 14,700 mg
In a patient weighing 10 kg, the distribution into total body water (Vd) will be 6 L—this is the amount of the body water into which the ethanol will be distributed.
14,700 mg ÷ 6 L = 2450 mg/L
2450 mg/L ÷ 10 = 245 mg/dL
Based on these calculations, a 10-kg child consuming 0.5 oz would have a concentration of 122.5 mg/dL; a 20-kg child consuming 1 oz would have a concentration of 122.5 mg/dL; a 30-kg child consuming 1 oz would have a concentration of 81.7 mg/dL; and a 70-kg adult consuming 1 oz would have a concentration of 35 mg/dL.
One “pump” from a hand sanitizer bottle dispenses approximately 2.5 mL of the product. If ingested, this amount (containing 62% ethanol) would create a blood ethanol concentration as follows:
1. In a 10-kg child: 23.1 mg/dL.
2. In a 20-kg child: 11.6 mg/dL.
3. In a 30-kg child: 7.7 mg/dL.
Children show a change in sensorium with blood levels as low as 10–20 mg/dL and any child displaying such changes should be seen immediately. Although a “lick” or a “drop” is unlikely to produce toxicity, the accuracy of the history should be considered when determining whether or not to see a child.
Complete absorption of alcohol requires 30 minutes to 6 hours, depending on the volume, the presence of food, and the time spent in consuming the alcohol. The rate of metabolic degradation is constant (about 20 mg/h in an adult). Absolute ethanol, 1 mL/kg, results in a peak blood level of about 100 mg/dL in 1 hour after ingestion. Acute intoxication and chronic alcoholism increase the risk of subarachnoid hemorrhage.
 Treatment
Treatment
Management of hypoglycemia and acidosis is usually the only measure required. Start an IV drip of D5W or D10W if blood glucose is less than 60 mg/dL. Fructose and glucagon have been suggested but are no longer used. Death is usually caused by respiratory failure. In severe cases, cerebral edema may occur and should be appropriately treated.
AMPHETAMINES & RELATED DRUGS (METHAMPHETAMINE, MDMA)
 Clinical Presentation
Clinical Presentation
A. Acute Poisoning
Amphetamine, 3,4-methylenedioxy-N-methylamphetamine (MDMA), and methamphetamine poisoning is common because of the widespread availability of “diet pills” and the use of “ecstasy,” “speed,” “crank,” “crystal,” and “ice” by adolescents. (Care must be taken in the interpretation of slang terms because they have multiple meanings.) A new cause of amphetamine poisoning is drugs for treating attention-deficit/hyperactivity disorder, such as methylphenidate. There are also newer designer drugs, synthetic cannabinoids (“spice, K2”) and MPDV or mephedrone (“bath salts, plant food”), which cause effects similar to stimulants.
Symptoms include central nervous system (CNS) stimulation, anxiety, hyperactivity, hyperpyrexia, diaphoresis, hypertension, abdominal cramps, nausea and vomiting, and inability to void urine. MDMA has been associated with hyponatremia and seizures. Severe cases often include rhabdomyolysis. A toxic psychosis indistinguishable from paranoid schizophrenia may occur. Methamphetamine laboratories in homes are a potential cause of childhood exposure to a variety of hazardous and toxic substances. Maternal use and the effect on the fetus as well as exposures of young children are a continuing problem.
B. Chronic Poisoning
Chronic amphetamine users develop tolerance; more than 1500 mg of IV methamphetamine can be used daily. Hyperactivity, disorganization, and euphoria are followed by exhaustion, depression, and coma lasting 2–3 days. Heavy users, taking more than 100 mg/d, have restlessness, incoordination of thought, insomnia, nervousness, irritability, and visual hallucinations. Psychosis may be precipitated by the chronic administration of high doses. Chronic MDMA use can lead to serotonin depletion, which can manifest as depression, weakness, tremors, GI complaints, and suicidal thoughts.
 Treatment
Treatment
The treatment of choice is diazepam, titrated in small increments to effect. Very large total doses may be needed. In cases of extreme agitation or hallucinations, droperidol (0.1 mg/kg per dose) or haloperidol (up to 0.1 mg/kg) parenterally has been used. Hyperthermia should be aggressively controlled. Chronic users may be withdrawn rapidly from amphetamines. If amphetamine–barbiturate combination tablets have been used, the barbiturates must be withdrawn gradually to prevent withdrawal seizures. Psychiatric treatment should be provided.
Carvalho M et al: Toxicity of amphetamines: an update. Arch Toxicol 2012;86(8):1167–1231 [PMID: 22392347].
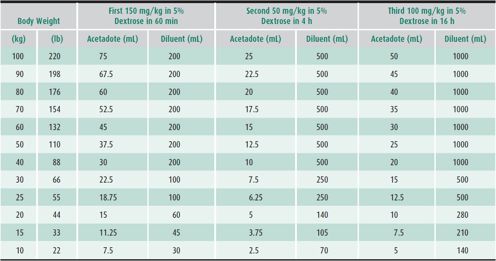
ANESTHETICS, LOCAL
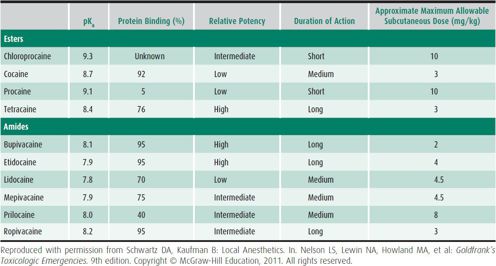
Intoxication from local anesthetics may be associated with CNS stimulation, acidosis, delirium, ataxia, shock, convulsions, and death. Methemoglobinemia has been reported following local mouth or dental analgesia, typically with benzocaine or prilocaine. It has also been reported with use of topical preparations in infants. The maximum recommended dose for subcutaneous (SQ) infiltration of lidocaine is 4.5 mg/kg (Table 13–3). The temptation to exceed this dose in procedures lasting a long time is great and may result in inadvertent overdosage. PO application of viscous lidocaine may produce toxicity. Hypercapnia may lower the seizure threshold to locally injected anesthetics.
Table 13–3. Pharmacologic properties of local anesthetics.
Local anesthetics used in obstetrics cross the placental barrier and are not efficiently metabolized by the fetal liver. Mepivacaine, lidocaine, and bupivacaine can cause fetal bradycardia, neonatal depression, and death. Accidental injection of mepivacaine into the head of the fetus during paracervical anesthesia has caused neonatal asphyxia, cyanosis, acidosis, bradycardia, convulsions, and death.
 Treatment
Treatment
If the anesthetic has been ingested, mucous membranes should be cleansed carefully and activated charcoal may be administered. If it is a topical application, the area should be cleaned and irrigated. Oxygen administration is indicated, with assisted ventilation if necessary. Symptomatic methemoglobinemia is treated with methylene blue, 1%, 0.2 mL/kg (1–2 mg/kg per dose, IV) over 5–10 minutes; this should promptly relieve the cyanosis. Acidosis may be treated with sodium bicarbonate, seizures with diazepam, and bradycardia with atropine. In the event of cardiac arrest, 20% fat emulsion therapy should be initiated. Initial 1.5 mL/kg bolus over 1 minute, followed by 0.25 mL/kg/min for up to 20–30 minutes until spontaneous circulation returns. Repeat bolus can be considered. Therapeutic levels of mepivacaine, lidocaine, and procaine are less than 5 mg/mL.
Ozcan MS, Weinberg G: Update on the use of lipid emulsions in local anesthetic systemic toxicity: a focus on differential efficacy and lipid emulsion as part of advanced cardiac life support. Int Anesthesiol Clin 2011;29(4):91–103 [PMID: 21956080].
Spiller HA et al: Multi-center retrospective evaluation of oral benzocaine exposure in children. Vet Hum Toxicol 2000;42:228 [PMID: 10928690].
ANTIHISTAMINES & COUGH & COLD PREPARATIONS
The use of cough and cold preparations in young children has recently been called into question due to potential toxicity. In 2007, manufacturers voluntarily removed preparations intended for use in children younger than the age of 4 from the market. Considerable controversy remains as to the toxicity of these medications if they are used according to labeled directions and an evaluation of the cases on file at FDA stated, “In the cases judged to be therapeutic intent or unknown intent, several factors appeared to contribute to the administration of an overdosage: administration of two medicines containing the same ingredients, failure to use a measuring device, use of an adult product, use of the wrong product because of product misidentification, and two or more caregivers administering the same medication. In the cases of non-therapeutic intent, circumstances involved attempts at sedation and several included apparent attempts of overt child abuse and were under investigation by law enforcement authorities.”
Medications included in this area are: antihistamine (brompheniramine, chlorpheniramine, diphenhydramine, doxylamine), antitussive (dextromethorphan), expectorant (guaifenesin), and decongestant (pseudoephedrine, phenylephrine). Although antihistamines typically cause CNS depression, children often react paradoxically with excitement, hallucinations, delirium, ataxia, tremors, and convulsions followed by CNS depression, respiratory failure, or cardiovascular collapse. Anticholinergic effects such as dry mouth, fixed dilated pupils, flushed face, fever, and hallucinations may be prominent.
They are absorbed rapidly and metabolized by the liver, lungs, and kidneys. A potentially toxic dose is 10–50 mg/kg of the most commonly used antihistamines, but toxic reactions have occurred at much lower doses.
 Treatment
Treatment
Activated charcoal should be used to reduce drug absorption. Whole bowel irrigation may be useful for sustained-release preparations. Physostigmine (0.5–2.0 mg IV, slowly administered) dramatically reverses the central and peripheral anticholinergic effects of antihistamines, but it should be used only for diagnostic purposes in patients without cardiotoxicity or seizures. Benzodiazepines, such as lorazepam (0.1 mg/kg IV) can be used to control seizures or agitation. Cardiac dysrhythmias and hypotension should be treated with normal saline at a dose of 10–20 mg/kg and a vasopressor if necessary. Sodium bicarbonate may be useful if there is QRS widening at a dose of 1–2 mEq/kg, making certain that the arterial pH does not exceed 7.55. Forced diuresis is not helpful. Exchange transfusion was reported to be effective in one case.
Dart RC et al: Pediatric fatalities associated with over the counter (nonprescription) cough and cold medications. Ann Emerg Med 2009;53:411–417 [PMID: 19101060].
Yin S. Malicious use of pharmaceuticals in children. J Pediatr 2010;157(5):832–836 [PMID: 20650468].
ARSENIC
Arsenic is used in some insecticides (fruit tree or tobacco sprays), rodenticides, weed killers, and wood preservatives. It can also be found in some fireworks. It is well absorbed primarily through the GI and respiratory tracts, but skin absorption may occur. Arsenic can be found in the urine, hair, and nails by laboratory testing.
Highly toxic soluble derivatives of this compound, such as sodium arsenite, are frequently found in liquid preparations and can cause death in as many as 65% of victims. The organic arsenates found in persistent or preemergence weed killers are relatively less soluble and less toxic. Poisonings with a liquid arsenical preparation that does not contain alkyl methanearsonate compounds should be considered potentially lethal. Patients exhibiting clinical signs other than gastroenteritis should receive treatment until laboratory tests indicate that treatment is no longer necessary.
 Clinical Findings
Clinical Findings
A. Acute Poisoning
Abdominal pain, vomiting, watery and bloody diarrhea, cardiovascular collapse, paresthesias, neck pain, and garlic odor on the breath occur as the first signs of acute poisoning. Convulsions, coma, anuria, and exfoliative dermatitis are later signs. Inhalation may cause pulmonary edema. Death is the result of cardiovascular collapse.
B. Chronic Poisoning
Anorexia, generalized weakness, giddiness, colic, abdominal pain, polyneuritis, dermatitis, nail changes, alopecia, and anemia often develop.
 Treatment
Treatment
In acute poisoning, administer activated charcoal. Then immediately give dimercaprol (commonly known as BAL), 3–5 mg/kg intramuscularly (IM), and follow with 2 mg/kg IM every 4 hours. The dimercaprol–arsenic complex is dialyzable. A second choice is succimer. The initial dose is 10 mg/kg every 8 hours for 5 days. A third choice is penicillamine, 100 mg/kg PO to a maximum of 1 g/d in four divided doses.
Chronic arsenic intoxication should be treated with succimer or penicillamine. Collect a 24-hour baseline urine specimen, greater than 50 mcg/L is elevated. Elevated levels must be correlated with history, as seafood can contain high levels of organic arsenic and cause a transient increase in urinary arsenic. With elevated levels, speciation of the sample is recommended, or a seafood holiday for 1 week and repeat lab work. If treatment is initiated, continue chelation for 5 days. After 10 days, repeat the 5-day cycle once or twice, depending on how soon the urine arsenic level falls below 50 mcg/L/24 hrs.
Abernathy CO et al: Arsenic: health effects, mechanisms of actions, and research issues. Environ Health Perspect 1999;107:593 [PMID: 10379007].
Stephanopoulus DE et al: Treatment and toxicokinetics of acute pediatric arsenic ingestion: danger of arsenic insecticides in children. Pediatr Crit Care Med 2002;3(1):74–80.
BARBITURATES & BENZODIAZEPINES
Barbiturates are rarely used today, and have mostly been replaced with benzodiazepines for their use in seizures or for sedation. The toxic effects of barbiturates include confusion, poor coordination, coma, miotic or fixed dilated pupils, and respiratory depression. Respiratory acidosis is commonly associated with pulmonary atelectasis, and hypotension occurs frequently in severely poisoned patients. Ingestion of more than 6 mg/kg of long-acting or 3 mg/kg of short-acting barbiturates is usually toxic. Benzodiazepines typically cause CNS depression and lethargy in unintentional oral ingestions. Large oral overdoses or iatrogenic IV overdose can cause cardiovascular or respiratory depression.
 Treatment
Treatment
Careful, conservative management with emphasis on maintaining a clear airway, adequate ventilation, and control of hypotension is critical. Urinary alkalinization and the use of multiple-dose charcoal may decrease the elimination half-life of phenobarbital but have not been shown to alter the clinical course. Hemodialysis is not useful in the treatment of poisoning with short-acting barbiturates or benzodiazepines. Analeptics are contraindicated. Flumazenil can be considered if severe CNS depression or respiratory depression develops after benzodiazepine overdose using a dose of 0.01 mg/kg IV (maximum dose of 0.2 mg).
Gaudreault P et al: Benzodiazepine poisoning: clinical and pharmacological considerations and treatment. Drug Saf 1991;6(4):247 [PMID: 1888441].
Kreshak AA et al: Flumazenil administration in poisoned pediatric patients. Pediatr Emerg Care 2012;28(5):488 [PMID: 22531190].
BELLADONNA ALKALOIDS (ATROPINE, JIMSONWEED, POTATO LEAVES, SCOPOLAMINE, STRAMONIUM)
The effects of anticholinergic compounds include dry mouth; thirst; decreased sweating with hot, dry, red skin; high fever; and tachycardia that may be preceded by bradycardia. The pupils are dilated, and vision is blurred. Speech and swallowing may be impaired. Hallucinations, delirium, and coma are common. Leukocytosis may occur, confusing the diagnosis.
Atropinism has been caused by normal doses of atropine or homatropine eye drops, especially in children with Down syndrome. Many common plants and over-the-counter medications contain belladonna alkaloids.
 Treatment
Treatment
If the patient is awake and showing no signs or symptoms, administration of activated charcoal can be considered. Gastric emptying is slowed by anticholinergics, so that gastric decontamination may be useful even if delayed. Benzodiazepines should be administered to control agitation. Bolus dosing should be given in escalating doses, and high doses may be required. Physostigmine (0.5–2.0 mg IV, administered slowly) dramatically reverses the central and peripheral signs of atropinism but should be used only as a diagnostic agent. It should not be given in patients with cardiotoxicity or seizures. Hyperthermia should be aggressively controlled. Catheterization may be needed if the patient cannot void.
Burns MJ et al: A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning. Ann Emerg Med 2000;35:374 [PMID: 10736125].
Vearrier D, Greenberg MI: Anticholinergic delirium following Datura stramonium ingestion: implications for the internet age. J Emerg Trauma Shock 2010;3(3):303 [PMID: 20930988].
β-BLOCKERS & CALCIUM CHANNEL BLOCKERS
β-Blockers and calcium channel blockers primarily cause cardiovascular toxicity; bradycardia, hypotension, and various degrees of heart block; a cardiac dysrhythmias may develop. Severe toxicity can cause CNS depression. The β-blocker propranolol is associated with seizures. Hyperglycemia can be seen with calcium channel blocker toxicity.
 Treatment
Treatment
Initial stabilization with IV fluid resuscitation with isotonic fluids should be initiated. Atropine can be given for symptomatic bradycardia. Calcium at doses of 20 mg/kg and repeated as needed should be administered. Infusions of calcium chloride 10%, 0.2–0.5 mL/kg/h, can be started after initial bolus dosing. Glucagon can be administered; 50–100 mcg/kg (5–10 mg) IV bolus followed by 2–5 mg/h infusion if patient improves. Vasopressors such as dopamine or norepinephrine should be started if patient continues to be hypotensive and bradycardic. In patients who are severely poisoned and refractory to these initial measures, hyperinsulinemia euglycemic therapy should be started. Your regional poison control center should be contacted for further details on dosing of this therapy.
Dewitt CR, Waksman JC: Pharmacology, pathophysiology and management of calcium channel blocker and beta-blocker toxicity. Toxicol Rev 2004;23(4):223–238 [PMID: 15898828].
Engebretsen KM, Kaczmarek KM, Morgan J, Holger JS: High-dose insulin therapy in beta-blocker and calcium channel-blocker poisoning. Clin Toxicol (Phila) 2011;49(4):277–283 [PMID: 21563902].
CARBON MONOXIDE
The degree of toxicity correlates well with the carboxyhemoglobin level taken soon after acute exposure but not after oxygen has been given or when there has been some time since exposure. Onset of symptoms may be more rapid and more severe if the patient lives at a high altitude, has a high respiratory rate (ie, infants), is pregnant, or has myocardial insufficiency or lung disease. Normal blood may contain up to 5% carboxyhemoglobin (10% in smokers). Neonates may have elevated carboxyhemoglobin levels due to breakdown of bilirubin.
Presenting symptoms can include nonspecific symptoms such as headache or flu-like illness. Other effects include confusion, unsteadiness, and coma. Proteinuria, glycosuria, elevated serum aminotransferase levels, or ECG changes may be present in the acute phase. Permanent cardiac, liver, renal, or CNS damage occurs occasionally. The outcome of severe poisoning may be complete recovery, vegetative state, or any degree of mental injury between these extremes. The primary mental deficits are neuropsychiatric.
 Treatment
Treatment
The biologic half-life of carbon monoxide on room air is approximately 200–300 minutes; on 100% oxygen, it is 60–90 minutes. Thus, 100% oxygen should be administered immediately. Hyperbaric oxygen therapy at 2.0–2.5 atm of oxygen shortens the half-life to 30 minutes. The use of hyperbaric oxygen therapy for delayed neurologic sequelae can be considered, but remains controversial. After the level has been reduced to near zero, therapy is aimed at the nonspecific sequelae of anoxia. Evaluation of the source should be performed before the patient returns to the home.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


