Fig. 8.1
Linear and whorled nevoid hypermelanosis. A form of pigmentary mosaicism that follows the lines of Blaschko
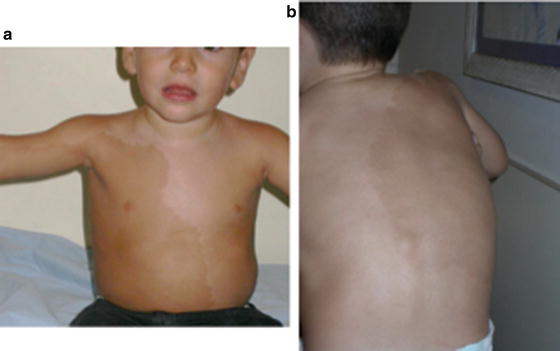
Fig. 8.2
Pigmentary mosaicism in a lateralization pattern. (a) Front view and (b) back view
Table 8.1
Patterns of pigmentary mosaicism
Patterns of pigmentary mosaicism | Clinical features |
|---|---|
Linear and whorled hypermelanosis | Reticulated, streaky, narrow and whorled macules occur along Blaschko lines |
Broad band Hyperpigmentarion | Broad band of hyperpigmetation that follow Blaschko lines |
Patchy hyperpigmentation | Irregularly shaped macules without midline separation |
Checkerboard pattern | Alternating squares of pigmentary anomalies with a sharp midline separation or arranged in a flag-like pattern |
Lateralization pattern | Hyperpigmented macules affect only one side with midline separation |
Associated extracutaneous manifestations have been reported in as much as 30 % of the cases, although this figure may reflect a reporting bias [10]. The associated findings include developmental delay, autism, seizures, microcephaly, and ocular, cardiac (ventricular septal defects and tetralogy of Fallot), and skeletal abnormalities (digit abnormalities, hemiatrophy).
The associated anomalies are so diverse that clinical investigation should be directed by clinical findings.
Pathogenesis
An enormous range of cytogenetic abnormalities has been reported in PM, including polyploidy, aneuploidy, and chromosomal deletions, insertions, and translocations. Mosaic trisomy 20, 7, 14, 18, and X-chromosomal have been reported in linear and whorled nevoid hypermelanosis [11–13]. The cytogenetic abnormalities may be only be found in fibroblast of affected skin. There is no single genotype for each phenotypic expression of pigmentary mosaicism except may be for phylloid hypermelanosis that has been more consistently related to chromosome 13 aberrations or mosaic chromosome 5p tetrasomy [4, 14] In most cases of pigmentary mosaicism a cytogenetic alteration cannot be detected and several hypotheses have been proposed to explain the abnormal pigmentation, such as comigration of genetically different cell populations, X-chromosome functional disomy, “Spreading” of X inactivation to autosomes, transposons, genetic imprinting, and phenotypic reversion [15].
Histology usually shows hyperpigmentation of the basal keratinocytes with normal number of melanocytes.
Treatment
No effective treatment has been described
There is no effective treatment for pigmentary mosaicism.
Prognosis
The hyperpigmented macules persist throughout life. The prognosis is marked by the associated extracutaneous findings.
Conclusion
Pigmentary mosaicism is a common usually sporadic disorder. Many different names have been used to describe it due to the fact that clinically it may manifest in any of the five patterns of cutaneous mosaicism described by Happle [9].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


