The difference between a wide and narrow therapeutic window
Pregnancy and pharmacokinetics
Due to the very large physiological changes associated with pregnancy, it is mainly drug handling that is affected rather than intrinsic drug actions.
The most relevant factors include:
Large increase in circulating volume (40–50%)
Concomitant large increased in renal blood flow and consequent GFR
Increased third space availability (amniotic fluid and peripheral oedema)
Relatively increased fat content due to laying down of maternal fat reserves
Reduced albumin and other binding proteins due to the overall plasma dilution effect
Progressive insulin resistance affecting medication for diabetes
This results in:
Increased clearance of most drugs reducing serum concentrations and sometimes efficacy. There are certain clinical conditions in pregnancy where this may require close drug monitoring and usually increases in drug doses over the course of pregnancy:
Anticonvulsants such as carbamazepine, phenytoin, valproate, lamotrigine and gabapentin especially where fit frequency is closely related to serum levels.
Mood stabilisers such as lithium where stable mood is vital and toxicity is particularly significant.
Common endocrine disorders in young women such as hypothyroidism – thyroxine inevitably need to be increased to keep thyroid function normal.
Pregnancy is characterised by progressive insulin resistance – women with pre-existing diabetes invariably need large increases in diabetic medication, especially insulin, as pregnancy advances.
While most drugs have reduced levels due to altered Pk, the effect may be less marked for:
Pharmacodynamics
Describe what the drug does to the body i.e. the drug effect. There are generally four major drug effects:
Receptors – tend to be metabotropic or ionotropic
Ionotropic receptors directly open or close an ion-pore in a membrane
Metabotropic receptors are indirectly linked to ion channels in plasma membranes via signal transduction by secondary messengers, usually G-coupled proteins.
Drugs can be agonists, antagonists or occasionally have a mixed effect on receptors. Table 26.1 gives some examples of drugs and their target receptors.
Enzyme interaction – the majority of licensed drugs that influence enzymatic reactions tend to inhibit them (Table 26.2 and Figure 26.3)
Membrane ion channels – most licensed drugs are generally designed to block ion channels (Table 26.3 and Figure 26.4)
Metabolic processes e.g. antibiotics and ribosome / DNA synthesis (Table 26.4 and Figure 26.5)
| Drug name | Receptor |
|---|---|
| Agonists | |
| Salbutamol | β1 and β2 adrenergic |
| Methyldopa | α2 adrenergic |
| Phenylephrine | α1 adrenergic |
| Pilocarpine | Muscarinic |
| Diazepam | GABA |
| Morphine | μ-opioid |
| Cabergoline | Dopamine |
| Antagonists | |
| Atenolol | β1 adrenergic |
| Labetolol | α1, β1 adrenergic |
| Doxazocin | α1 adrenergic |
| Tolterodine | Muscarinic |
| Ranitidine | Histamine (H2) |
| Cyproterone acetate | Testosterone |
| Metoclopramide | Dopamine |
| Drug name | Enzyme |
|---|---|
| Diclofenac | Cyclo-oxygenase (COX) inhibition |
| Ramipril | Angiotensin-converting enzyme (ACE) inhibition |
| Neostigmine | Anti-cholinesterase inhibition |
| Zidovudine | Reverse transcriptase inhibition |
| Acyclovir | HSV-specific thymidine kinase inhibition |
| Warfarin | Vitamin K epoxide reductase inhibition |
| Methotrexate | Dihydrofolate reductase inhibition |
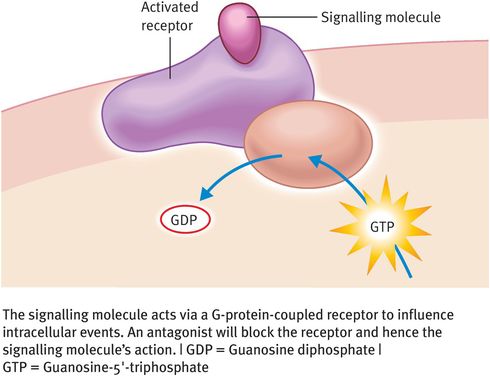
Muscarinic receptors as a signaling molecule act via G-protein coupled receptors to influence intracellular events. An antagonist will block the receptor and hence its action
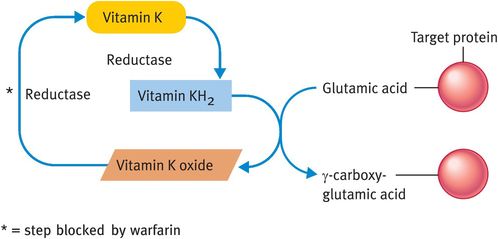
The enzyme block due to warfarin
| Drug name | Ion channel |
|---|---|
| Nifedipine | Calcium blocker |
| Diltiazem | Calcium blocker |
| Verapamil | Calcium blocker |
| Lignocaine | Sodium blocker |
| Amiloride | Sodium blocker |
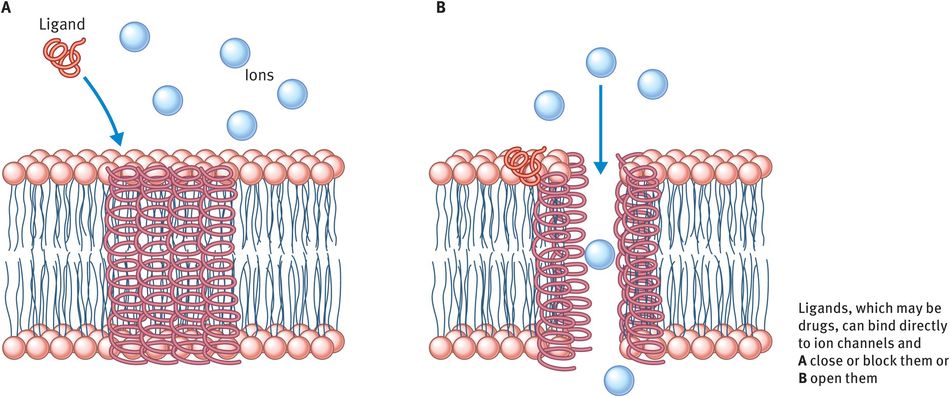
Ligands which may be drugs can bind directly to ion channels and open or close them. Nifedipine blocks the calcium influx seen here
| Drug name | Process |
|---|---|
| Gentamicin | Inhibition of ribosome synthesis |
| Erythromicin | Inhibition of protein translocation |
| Doxycycline | Inhibition of protein translation |
| Carboplatin | DNA alkylating agent |
| Paclitaxel | Cellular microtubule function |
| Vincristine | Spindle poison |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


