Periventricular Calcification
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
TORCH, General
Congenital CMV
Congenital Toxoplasmosis
Congenital Herpes Encephalitis
Congenital HIV
Congenital Rubella
Tuberous Sclerosis Complex
Less Common
Neurocysticercosis
Tuberculosis
Ventriculitis (Chronic)
Germinal Matrix Hemorrhage
Rare but Important
Radiation and Chemotherapy
Pseudo-TORCH
Aicardi-Goutières Syndrome
Coats-Plus Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Look for associations
Brain destruction
Malformations
Other loci of calcification
History
Helpful Clues for Common Diagnoses
TORCH, General
Classic acronym for congenital infections
Caused by transplacental transmission of pathogens
Toxoplasmosis
Rubella
Cytomegalovirus
Herpes
All cause parenchymal calcifications
Most can cause lenticulostriate mineralization, vasculopathy
Some (CMV) cause migrational defects
Some (syphilis, herpes) cause meningitis, meningoencephalitis
Some (e.g., CMV) cause germinolytic cysts
Others (e.g., rubella, HSV) cause striking lobar destruction/encephalomalacia
Congenital HIV, syphilis also considered part of TORCH
Consider congenital HIV
If bilateral symmetric basal ganglia calcifications identified in child > 2 months old
If congenital infection is diagnostic consideration, obtain NECT to detect calcifications
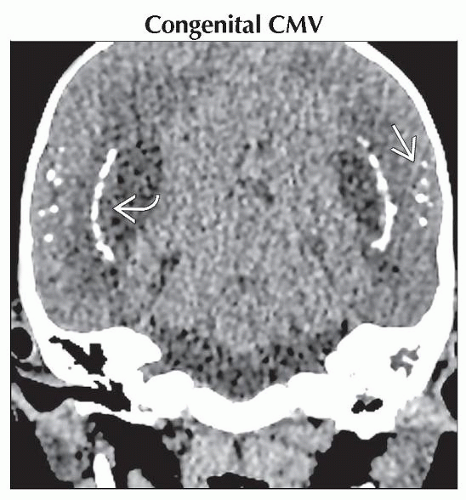
Congenital CMV
Most common cause of intrauterine infection in USA
Timing of infection predicts pattern of damage
Hypomyelination
Cortical gyral anomalies
Microcephaly
Symmetric periventricular calcifications in 30-70%
Congenital Toxoplasmosis
Periventricular and scattered calcifications
Hydrocephalus (colpocephaly-like)
Congenital Herpes Encephalitis
Calcification pattern varies in HSV2
Asymmetric periventricular
Scattered periventricular and deep gray
Subcortical white matter and cortex
Calcification pronounced in foci of hemorrhagic ischemia
Like rubella, rare cause of “stone brain”
Brain atrophy or cystic encephalomalacia
Focal or diffuse
Congenital HIV
Vertical HIV infection
Basal ganglia calcifications
Atrophy
Consider congenital HIV
If bilateral symmetric basal ganglia calcifications present and child is > 2 months old
Congenital Rubella
Periventricular and scattered calcifications
Scattered or hazy basal ganglia calcifications
Rarely “stone brain”
Extensive gyral calcification
Gliosis
Micro-infarcts
Tuberous Sclerosis Complex
Helpful Clues for Less Common Diagnoses
Neurocysticercosis
Best clue: Dot inside cyst
Usually convexity subarachnoid space
Also gray-white junction, intraventricular
Nodular calcified (healed) stage
Shrunken calcified nodule
Tuberculosis
Best diagnostic clue
Basal meningitis
Pulmonary tuberculosis
Acute
Typically basal meningitis
± localized CNS tuberculoma
Chronic
Residual pachymeningeal
± localized calcifications
“Target” sign
Calcification surrounded by enhancing rim (not specific)
Ventriculitis (Chronic)
Areas of prior hemorrhagic infarction prone to dystrophic calcification
Germinal Matrix Hemorrhage
Occasional ependymal, germinal matrix calcific foci
Helpful Clues for Rare Diagnoses
Radiation and Chemotherapy
History
Mineralizing microangiopathy
Pseudo-TORCH
Aicardi-Goutières Syndrome
“Mendelian mimic of congenital infection”
Multifocal punctate calcifications
Variable locations including periventricular white matter, basal ganglia, dentate nuclei
Elevated CSF interferon (IFN-α)
TREX1 mutations in some
Coats-Plus Syndrome
a.k.a. cerebroretinal microangiopathy with calcifications and cysts
Ocular coats: Retinal telangiectasia and exudate
CNS small blood vessel calcification
Extensive thalamic and gyral calcification
Defects of bone marrow and integument
Growth failure
Image Gallery
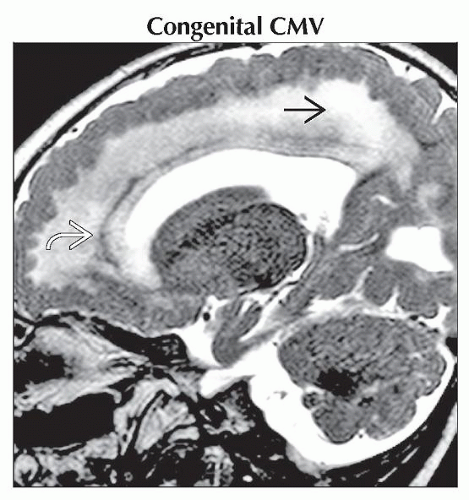 Sagittal T2WI MR shows a thick cortex with small gyri, hyperintense white matter
 , and a thin layer of calcification , and a thin layer of calcification  in the same 18-month-old deaf toddler. in the same 18-month-old deaf toddler.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|