Pericardial Diseases
Julien I. E. Hoffman
The pericardium is a 2-layered sac that contains the heart and the proximal parts of the great vessels. The outer surface of the sac is termed the parietal pericardium and is lined by mesothelial cells. The inferior part of the sac is attached to the diaphragm. The inner layer of the sac, also lined by mesothelial cells, is attached to the cardiac surface and is known as the visceral pericardium. A small amount of fluid fills the cavity between the pericardial layers and acts as a lubricant so that the heart can move within the sac. The parietal pericardium has blood and lymphatic vessels. Disorders that affect the pericardium may be primary or secondary to disease elsewhere in the body, including the heart itself.
Whatever the cause, there are only 3 manifestations: acute or chronic inflammation of the pericardial sac in response to injury or accumulation of fluid between the 2 layers—a pericardial effusion with or without a tamponade.
ACUTE PERICARDITIS
Acute pericarditis has many causes (see Table 491-1). No matter what the cause, the presentation is similar.
1. Chest pain is usually precordial and often referred to the neck, shoulder, or epigastrium. The pain is sharp or burning and is usually made better by sitting up and leaning forward. It is made worse by taking in a deep breath because inspiration lowers the diaphragm, pulls the pericardial sac down, and narrows it, thereby causing the 2 pericardial layers to rub together more forcefully.
2. A pericardial friction rub is heard. A grating sound occurs when the 2 layers rub together. This rub has the sound of sandpaper on wood, but occasionally resembles creaking leather. The friction rub has a to-and-fro rhythm (or sometimes 3 components) and is heard in systole and diastole. It may become louder with firm pressure and is heard best along the left sternal border, with the patient sitting up and leaning forward. The rub, however, may be intermittent. The auscultator should not confuse a friction rub with the sounds made when the stethoscope is moved over skin or chest hairs.
Table 491-1 Etiologya of Pericarditis
A. Idiopathic, presumed viral |
B. Acute infections: |
(1) Viral-coxsackie A and B, echovirus, adenovirus, mumps virus, influenza virus, varicella zoster and vaccinia viruses, Epstein-Barr virus, infectious mononucleosis, psittacosis-lymphogranuloma venereum group, cytomegalovirus, rubella, herpes simplex, human immunodeficiency virus |
(2) Bacterial-staphylococci, pneumococci, Haemophilus influenzae, meningococci, streptococci, Salmonella, mycobacteria with HIV infection virus |
(3) Mycoplasma |
(4) Protozoa—amebae, toxoplasmosis |
(5) Rickettsia—Coxiella burnetii |
C. Physical causes: |
(1) Hemopericardium and pericarditis after chest trauma or cardiac surgery |
(2) Serous or serosanguineous effusions after cardiac trauma, cardiac surgery, or myocardial infarctions; all may result from autoimmune mechanisms |
(3) Perforation of right atrium by indwelling lines, even soft silastic catheters |
(4) Chest well radiation |
D. Chronic infections: |
(1) Tuberculosis, actinomycosis, nocardiasis |
(2) Fungi—histoplasmosis, coccidiomycosis, Candida spp, aspergillosis, blastomycosis |
(3) Hydatid disease |
E. Associated with anasarca in congestive heart failure, nephrosis, or cirrhosis of the liver |
F. Vasculitis syndromes, especially systemic lupus erythematosus, rheumatoid arthritis, and rheumatic fever, but also scleroderma, polyarteritis, Wegener granulomatosis, Behçet syndrome, Reiter syndrome, Whipple disease |
G. Metabolic disorders—uremia, myxedema, gout |
H. Hemodialysis |
I. Congenital heart disease, cardiomyopathy |
J. Benign and malignant cavity |
K. Drugs—hydralazine, procainamide, phenytoin, isoniazid, phenylbutazone, methysergide, penicillin, anticoagulants, practolol, minoxidil |
L. Certain anemias—sickle cell disease, thalassemia, congenital aplastic anemia |
M. Miscellaneous—dissecting aneurysm, acute, pancreatitis, sarcoidosis, multiple myeloma, amyloidosis, Kawasaki syndrome, ulcerative colitis |
aThe most commone causes are printed in bold type.
3. Fever is common and has no special characteristics. As a rule, it is higher when there is an acute bacterial infection (staphylococcus, pneumococcus, haemophilus) than a viral infection.
4. The electrocardiogram initially shows elevation of the ST segments in the leads facing the pericardium (I, II, aVF, V3 to V6) because the inflammation of the visceral pericardium extends deeper to the superficial myocardium and produces a current of injury that changes the ST segment. Leads that do not face the epicardium (aVR and V1) show reciprocal ST depression. These diffuse ST changes help to separate acute pericarditis from acute myocardial infarction in which the current of injury is localized to a few leads. After 5 to 7 days, the ST segments return to the baseline and then become inverted in the leads that originally showed elevation. Unlike the changes of myocardial ischemia, these inverted T waves are symmetrical. With recovery the electrocardiogram usually returns to normal, but in some patients may remain abnormal for years.
5. Chest x-ray is unremarkable in the absence of an effusion.
Treatment of acute pericarditis depends on its cause and is discussed below.
PERICARDIAL EFFUSION
An increase in the amount of pericardial fluid is termed a pericardial effusion. The fluid may be serous, purulent, or bloody, and it moves the pericardial layers apart from each other.
1. An effusion per se produces no symptoms apart from those associated with its cause, thus an effusion is often unsuspected.
2. Because of the increased amount of fluid, the heart sounds are muffled and a previously heard pericardial friction rub may disappear. On the other hand, in some patients the heart may float on top of the fluid and bring out a friction rub not previously heard. A sign of a moderate or large effusion is an increased region of cardiac dullness on percussion, with the left edge of the dullness clearly beyond the position of the apex beat. This is one of the few times when cardiac percussion is useful.
3. Because the increased amount of pericardial fluid (if more than minimal) increases the intrapericardial volume, the chest x-ray may show an enlarged cardiac silhouette. Classically, this resembles a water flask (the kind made of flexible leather or skin) that has a narrow neck and a rounded bulging lower portion. Unfortunately, most patients with a pericardial effusion have nonspecific enlargement of the cardiac silhouette. Finding low concentrations of atrial natriuretic peptide or brain natriuretic peptide (BNP) indicates that the enlarged cardiac silhouette is not caused by cardiac dilatation.1
4. The electrocardiogram is nonspecific, but may show unusually small voltages in all leads due to the volume effect or electrical alternans because the heart may swing within the enlarged pericardial cavity.2-4
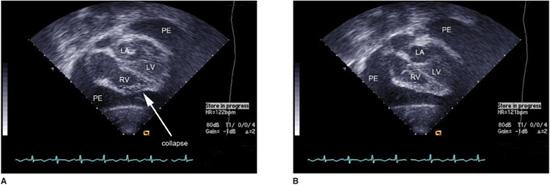
5. The gold standard for diagnosis is the echocardiogram that shows unequivocally the increased space between the pericardial layers (Fig. 491-1). Care is needed if smaller amounts of fluid are pooled behind the heart.
PERICARDIAL TAMPONADE
Normally, the pressure in the pericardial sac is low. When an effusion accumulates, the pressure may remain low if the increased fluid volume is small or accumulate so slowly that the parietal pericardium stretches and does not become tense. It is possible for a huge effusion to coexist with a normal intrapericardial pressure. If the effusion forms rapidly, or if the pericardium is stiff because of inflammatory changes, the intrapericardial pressure can rise and compress the heart—a pericardial tamponade. In these patients the cardiac silhouette may not be enlarged.5 A slowly enlarging effusion may be well tolerated for a long time, and then intrapericardial pressures may rise suddenly because the limits of pericardial distensibility have been reached. These pressure changes can occur rapidly. If the heart was previously enlarged, the events may be taken mistakenly to indicate worsening of the primary heart disease.
Compression impairs cardiac relaxation and filling. Ventricular end-diastolic and atrial pressures rise on both sides of the heart by about equal amounts, jugular venous pressure rises, the liver enlarges, and cardiac output and stroke volume fall. Heart rate increases, blood pressure and pulse pressure decrease, and there is reduced peripheral perfusion with cold, clammy extremities. Pericardial tamponade is a major cardiac emergency. Systolic function is not impaired initially, but left ventricular output is reduced because left ventricular filling is reduced. The patient has all the features of congestive heart failure and is often mistakenly diagnosed with such. Although an echocardiogram makes the definitive diagnosis of an effusion, it is often difficult to decide if there is a tamponade as well. It is best to make the diagnosis clinically by testing for Kussmaul sign and pulsus paradoxus.
Kussmaul sign is an increase in jugular venous pressure on inspiration. Normally, during inspiration the intrathoracic pressure decreases so that, despite the increased venous return, right atrial and jugular venous pressures decrease. If the compressed heart cannot accommodate the increased venous return, then the right atrial and jugular venous pressures increase. The sign is not specific because it can also occur with constructive pericarditis (see below), restrictive cardiomyopathy, and sometimes in right heart failure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


