Fig. 69.1
Intravenous urogram (IVU) showing bilateral PUJ obstruction
Prior to the use of prenatal ultrasonography, most patients with PUJ obstruction presented with pain, hematuria, urinary tract infections, failure to thrive, or a palpable mass.
With the increasing use and availability of prenatal ultrasonography, PUJ obstructions are being diagnosed earlier and more frequently.
About 50–67 % of antenatally diagnosed hydronephrosis are due to PUJ obstruction.
Initially, most patients with PUJ are treated conservatively and monitored closely.
Surgical intervention is indicated in the event of significantly impaired renal drainage or poor renal growth.
The treatment of PUJ obstruction has changed over the years and there are several corrective procedures including:
Laparoscopic pyeloplasty
Open pyeloplasty
Endopyelotomy
Endopyeloplasty
Robotic-assisted laparoscopic pyeloplasty
Etiology
There are several possible etiologies for PUJ obstruction .
These abnormalities all lead to impaired drainage of urine from the kidney into the ureter.
As a result of this, there is increased intrapelvic pressure, which leads to elevated intrarenal back pressure, dilatation of the collecting system, and hydronephrosis .
The etiologies of PUJ obstruction are classified into:
Intrinsic causes:
Developmental anomalies of the PUJ leading to congenital stenosis .
Insertional anomalies in which the ureter inserts into the renal pelvis at a location that is not the most dependent. This prevents efficient drainage of the pelvis.
Functional abnormalities such as an aperistaltic section of smooth muscle.
Abnormal collagen architecture within the stenotic PUJ.
Asymmetry of ureteral wall musculature and ureteral hypoplasia. This may lead to abnormal peristalsis leading to defective emptying of the renal pelvis.
Mucosal folds and ureteral polyps that may be due to anatomical abnormalities. These obstruct the ureter at the PUJ in a ball–valve fashion during periods of diuresis.
Neural depletion and decreased neuronal markers and nerve growth factors within the smooth muscle layer of the pelviureteric junction .
Extrinsic causes:
Due to causes exterior to the PUJ
Aberrant or accessory blood vessels (Aberrant polar vessels) (Fig. 69.2)
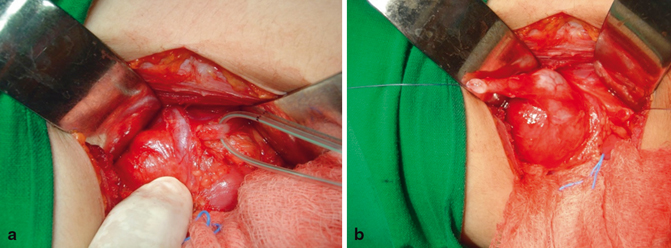
Fig. 69.2
Intraoperative photograph showing aberrant polar vessel causing hydronephrosis and intraoperative photograph showing the upper part of the ureter after its division. Note the normal ureter with no intrinsic cause of hydronephrosis
Scars and adhesions from previous surgery
Scarring and band formation from nephrolithiasis or urinary tract infection
Rotated and hypermobile kidney
Vesicoureteral reflux leading to stenosis
Additionally, PUJ obstruction is classified as primary and secondary.
Primary PUJ obstruction is due to developmental anomalies of the PUJ.
Secondary PUJ obstruction is due to other causes:
◦ Previous surgical intervention on the kidney
◦ Recurrent stone passage
◦ Recurrent urinary tract infection
◦ Vesicoureteral reflux
◦ Rotated and hypermobile kidney (Fig. 69.3)

Fig. 69.3
IVU showing hydronephrotic pelvic kidney
◦ Failed repair of a primary PUJ obstruction
Clinical Features
With the recent advancement in antenatal ultrasound, most cases of PUJ obstructions are diagnosed in utero .
Older children may present with:
Urinary tract infection
A flank mass
Intermittent flank pain
Hematuria
Investigations
All patients with possible PUJ obstruction should be evaluated with a complete blood count (CBC), coagulation profile, electrolytes, blood urea nitrogen (BUN) and creatinine, urine analysis, and culture. A plain abdominal X-ray may show a soft tissue density secondary to a hydronephrotic kidney (Fig. 69.4).
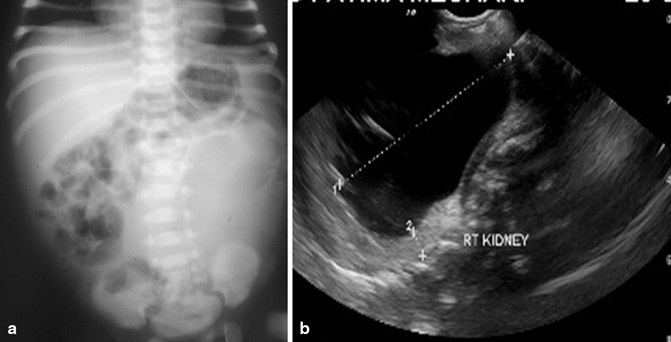
Fig. 69.4
A plain abdominal X-ray in a newborn with left hydronephrosis showing a soft tissue density on the left side and an abdominal ultrasound showing right hydronephrosis secondary to PUJ obstruction
Renal ultrasonography (Fig. 69.4a).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


