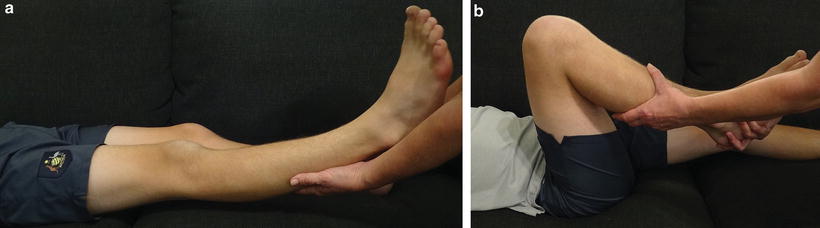
Fig. 11.1
The Silfverskiold test is used to determine the contribution of the gastrocnemius to the overall equinus contracture. The foot is dorsiflexed with the knee extended and then again with the knee flexed to 90°. If there is more dorsiflexion of the ankle possible with the knee flexed than with the knee extended, a gastrocnemius contracture is present. The test should be performed with the forefoot supinated and the sub-talar joint inverted to lock the midfoot joints
Imaging
Radiographically, equinus can be evaluated on a weight-bearing lateral radiograph in which the patient stands with the knee straight. The magnitude of the equinus can then be determined from the standing lateral radiograph by measuring the tibial-sole angle [6]. This is calculated by drawing a line along the sole of the foot from the plantar aspect of head of first metatarsal to plantar aspect of calcaneus and joining it with a line drawn along the long axis of the tibia (Fig. 11.2). The degree of equinus deformity can be categorized as mild (less than 20° plantarflexion), moderate (20°–40°) and severe (greater than 40°) [7].
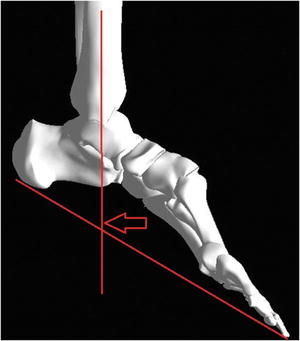
Fig. 11.2
The magnitude of the equinus can be measured on a lateral radiograph of the ankle by measuring the tibial-sole angle. Equinus deformity will have a measurement of greater than 90°
Management Strategy and Decision Making
Nonoperative
Most mild and some moderate equinus will respond to physical therapy with stretching, casting and bracing. Because early age at first surgery in children with cerebral palsy is a major risk factor for recurrent equinus deformity, temporizing measures to postpone the first surgery should be considered in younger children [8, 9]. Options include the use of botulinum toxin A, casting and orthoses. Serial casting should be performed with the patient in a prone position to obtain the most effective correction [10]. Botulinum toxin A has had successful short-term outcomes and may allow surgery to be delayed until after the age of 6 years in children with cerebral palsy [9]. Planning of surgical procedures can be based on the results of selective botulinum toxin A injections. Potential problems include the development of antibodies to botulinum toxin A and the cost of the treatment. Botulinum toxin A should only be used in muscles that produce dynamic deformities in the absence of fixed contracture.
Operative
Lengthening of Muscles and Tendons
If the patient demonstrates an equinus deformity with gait but the ankle has sufficient dorsiflexion past neutral on passive range of motion examination, the equinus is dynamic, and surgical treatment may not be needed. However, if the child has failed conservative management or demonstrates tripping, falling, or forefoot pain with functional impairment, then surgery should be considered [11]. The presence of a fixed equinus contracture at the ankle, with dorsiflexion to less than neutral is also an indication to operate. An important principle governing surgery for equinus is to use the most conservative gastrocnemius lengthening procedure possible to achieve approximately 5° of dorsiflexion with the knee extended [11]. The amount of lengthening required for a specific degree of fixed equinus is often much less than surgeons estimate. The appropriate surgical treatment for equinus deformity must not only achieve adequate length of the gastrocnemius–soleus complex to allow dorsiflexion in stance phase, but also preserve adequate strength and moment generation to control advancement of the tibia over the foot [11]. The most devastating complication of surgery for equinus deformity is excessive weakness of plantarflexion with a calcaneus gait. Surgery for recurrent equinus is possible but there are currently no reliable methods with which to shorten an over-lengthened gastrocnemius–soleus complex [11]. Therefore it is better to err on the side of undercorrection especially in patients with cerebral palsy and follow the philosophy “a little equinus is better than calcaneus” [11]. Overcorrection may result in a severe crouch gait and the loss of walking ability [11].
Operations designed to lengthen the triceps surae can be assigned to one of three discrete anatomical zones. Zone 1 starts at the gastrocnemius origin and ends at the most distal fibers of the medial belly of the gastrocnemius [9]. The operative procedures in Zone 1 include the Baumann and the Strayer distal gastrocnemius recession (Fig. 11.3). The procedure described by Baumann involves intramuscular lengthening of the gastrocnemius and soleus performed in the interval between the gastrocnemius and soleus fascia [13]. The gastrocnemius may be lengthened selectively, or differential lengthening of the gastrocnemius and soleus may be performed by varying the number of cuts in the fascia overlying the two muscles. Herzenberg et al. found it more effective to make a second more distal incision in the gastrocnemius muscle rather than adding an incision in the soleus [14]. At the junction of Zones 1 and 2 it is possible to perform selective lengthening of the gastrocnemius alone, as described by Strayer [15]. It is also possible to perform differential lengthening of the gastrocnemius and soleus by separating the gastrocnemius fascia from the soleus fascia and dividing the gastrocnemius aponeurosis and soleus fascia separately in a technique known as the modified Strayer procedure [11].
Fig. 11.3
Zone 1 level surgeries include the Baumann procedure and the Strayer procedure. Illustration created by and reprinted with permission of Daniel Biggers
Zone 2 extends from the distal end of the medial belly of the gastrocnemius muscle to the end of the soleus muscle [9]. This zone is characterized by condensation of the gastrocnemius fascia into a broad aponeurosis, which lies superficial to the soleus fascia. The layers are most accurately referred to as the conjoined gastrocnemius aponeurosis–soleus fascia [12]. The two Zone 2 layers can very rarely be separated and then only partially and by sharp rather than blunt dissection [12]. Zone 2 procedures include those of Vulpius and Baker and involve performing a gastrocnemius–soleus complex recession with the use of a single transverse division of both the gastrocnemius aponeurosis and the soleus fascia (Fig. 11.4). Neither selective nor differential lengthening of the two layers that comprise the conjoined tendon is possible in Zone 2 with these procedures [12]. The Zone 2 procedures are neither anatomically nor biomechanically equivalent to the Zone 1 procedures [12]. The Vulpius procedure is often grouped with the Strayer procedure and referred to as a gastrocnemius recession, when it is in fact a gastrocnemius–soleus complex recession [12].
Fig. 11.4
Zone 2 level surgeries include the Vulpius and the Baker procedures. Illustration created by and reprinted with permission of Daniel Biggers
Zone 3 extends from the end of the soleus muscle to the insertion of the Achilles tendon on the calcaneus [9]. The gastrocnemius aponeurosis and the soleus fascia provide two groups of fibers that are distinct at first, then rotate, and finally blend together within the substance of the Achilles tendon [12]. Zone 3 procedures include all forms of lengthening of the Achilles tendon, as well as heel cord advancement (Fig. 11.5). Zone 3 lengthening of the Achilles tendon should be used when there is a contracture of both the gastrocnemius and the soleus of greater than 30° and no improvement in ankle dorsiflexion is seen with knee flexion [11].
Fig. 11.5
Zone 3 level surgeries include the White and Hoke procedures. Illustration created by and reprinted with permission of Daniel Biggers
Achilles tendon lengthening may be performed by open or percutaneous techniques. In the open technique, a longitudinal incision is made just lateral to the Achilles tendon. The tendon is lengthened in Z-fashion and repaired with heavy non-absorbable suture. Percutaneous lengthening can be performed by either two or three transverse partial tenotomies. The first tenotomy is made proximal to the calcaneal insertion and a little more than half of the tendon is divided by inserting a scalpel longitudinally into the center of the tendon, turning the blade out toward the edge of the tendon, and pushing the tendon down onto the blade. The opposite half of the tendon is then divided by using a similar maneuver 3–4 cm more proximally. In a patient with a valgus hindfoot, the distal cut is through the lateral half of the tendon. In a varus hindfoot, the distal incision is through the medial half. After completing the incisions, the ankle should be dorsiflexed gradually with the heel inverted. The foot should be dorsiflexed to neutral. It is important to verify the integrity of the tendon after a percutaneous lengthening is performed. The surgeon should squeeze the calf and simultaneously watch the ankle. If the ankle plantarflexes when the calf is squeezed, then the tendon can be presumed to be intact within the tendon sheath. If there is no plantar flexion, the tendon may have been ruptured by the lengthening procedure and an open repair will be needed.
The stability of the musculotendinous unit after a particular lengthening procedure as well as the amount of lengthening achieved are directly related to the residual cross-sectional area of the soft tissues remaining intact at the site of the lengthening [12]. For example, after a Baumann intramuscular tenotomy, all of the soleus and gastrocnemius muscle fibers, plus the intact fascia on the posterior aspect of the gastrocnemius and the anterior aspect of the soleus remain intact. This confers excellent stability and resists further lengthening of the musculotendinous unit [12]. The Baumann procedure appears to yield good results in children with spastic diplegia and mild equinus deformities with no reported overcorrections [16]. Zone 2 procedures achieve greater lengthening than Zone 1 procedures [12]. This may be related to the decreasing cross-sectional area of muscle at the site of the fascial division. In Zone 3, the stability of the musculotendinous unit after a percutaneous triple hemi-section depends entirely on side-to-side links between the largely parallel collagen fibers of the tendon, which have been divided at three contiguous levels [12]. This may contribute to overlengthening and poor outcomes, especially in ambulatory children with spastic diplegia [12].
Therefore, there is no single surgical procedure that should be considered a panacea for all patients with equinus deformity. Rather, the history and physical examination will help guide the surgeon to decide which procedure may be more appropriate for each clinical situation. For example, in children with spastic hemiplegia and equinus deformity, the Silfverskiold test usually reveals a substantial fixed contracture of both the gastrocnemius and the soleus [12]. A Zone 2 lengthening (Vulpius) or a Zone 3 procedure (percutaneous hemi-section) might be selected, depending on the severity [12]. In contrast, a Zone 3 procedure in patients with spastic diplegia is associated with a very high prevalence of calcaneus deformity and crouch gait at long-term follow-up [12]. In these patients, the Silfverskiold test usually reveals either an isolated contracture of the gastrocnemius or a contracture of the gastrocnemius that is greater than that of the soleus [12]. Therefore, a Zone 1 procedure such as the Baumann or Strayer would be recommended. The type of cerebral palsy should be carefully considered when deciding on the type of surgical procedure and overall management of an equinus deformity [9].
The stability of the gastrocnemius–soleus musculotendinous unit after surgical lengthening may also be relevant to the decisions about postoperative care and rehabilitation protocols [12]. The intrinsic stability after Zone 1 or 2 lengthening may permit very early weight-bearing and relatively short periods of cast immobilization. The relative instability after Zone 3 lengthening and the documented tendency for continued lengthening under small loads may require longer immobilization and delayed weight-bearing [12].
A typical postoperative regimen after equinus surgery consists of a below-the-knee cast with the foot in a neutral dorsiflexion for 3 weeks. Unrestricted weight bearing beginning the first postoperative day is prescribed if a Zone 1 or Zone 2 procedure was performed. Casts are removed after 3 weeks to check healing and to cast molds for an ankle–foot orthosis. The standard postoperative ankle–foot orthosis is solid with hinges inserted but not activated [11]. Casts are reapplied and removed at 6 weeks after surgery where they are replaced by the ankle–foot orthoses.
The greatest risk after equinus surgery is recurrence and it correlates strongly with the age of the patient at surgery. Children with cerebral palsy who undergo heel cord lengthening at 7 years or younger are particularly at risk for recurrence [8]. Recurrence of equinus is also possible in cases of congenital disease, such as arthrogryposis, or with the loss of function of the anterior compartment muscle(s), as in severe burn cases, poliomyelitis, or nerve injury [6]. Recurrence in posttraumatic equinus is rare as long as the anterior tibial muscles are functional. Recurrent equinus can be corrected with a Vulpius gastrocnemius–soleus complex recession in Zone 2 [12]. In some cases of repeated lengthening the Achilles tendon becomes scarred and adherent, so the subsequent lengthenings must be done using the open technique.
When performing a lengthening the surgeon must be careful not to position the foot in excessive dorsiflexion. Overstretching of the tendon can lead to excessive length and calcaneus gait. Calcaneus can also occur after lengthening if there is an unrecognized flexion contracture of the knee. If the knee remains crouched and the Achilles tendon becomes longer, the ankle will drop into excessive dorsiflexion during stance phase and create an inefficient gait pattern.
External Fixation
While mild to moderately severe equinus contracture can be addressed with soft tissue lengthening, severe equinus deformities often cannot be corrected with a single open surgical procedure because the skin and neurovascular structures may not tolerate such an acute stretch. The Ilizarov method of gradual correction can be used in these situations. The risk of a neurovascular stretch injury during treatment can be further reduced by decompressing the posterior tibial neurovascular bundle at the tarsal tunnel during frame application, especially in the presence of any associated varus deformity [4]. If any neurologic compromise occurs during the gradual distraction, the rate of the distraction can be slowed or temporarily stopped to allow for neurological recovery. Nerve decompression should be considered when nerve function does not improve or if any new motor deficit is noted [4].
In addition to providing a method for correction of severe contractures, external fixation has several other advantages. During external fixation treatment there will be access to the soft tissues for wound care, especially in the presence of abnormal soft tissues such as scars, burns, and compromised skin [4]. External fixation also allows for adjusting the rate of deformity correction during the postoperative period and can allow for joint range of motion and early weight bearing [4].
All ankle external fixator constructs need to allow for distraction of the ankle joint space prior to beginning the deformity correction. This should be performed at the time of frame placement. In a simple equinus correction, the ankle should be distracted 2–5 mm compared with preoperative radiographs [6]. This limits cartilage compression of the ankle joint and any rockerbottom deformity that may occur as the ankle is brought into dorsiflexion [6]. The distraction of the hindfoot, however, must be done in a posterior-inclined direction. If distraction is performed in a purely axial direction, parallel to the tibia, the talus will tend to sublux anteriorly [6]. Fixation should be applied to both the talus and the calcaneus to prevent overdistraction of the subtalar joint during the correction of the tibiotalar joint contracture [4].
Types of External Fixation Constructs
There are three different types of external fixator constructs that may be used to correct equinus contractures depending on the hinge system used: constrained, unconstrained, and virtual. The constrained fixator has a single hinge centered on the axis of rotation of the ankle (Fig. 11.6). The normal trans-malleolar axis is 80° in the coronal plane and 84° in the sagittal plane [6]. Therefore, the axis created by the hinges is positioned on a slightly oblique plane with respect to the horizontal from the tip of the lateral malleolus to just distal to the tip of the medial malleolus [6]. Anterior subluxation of the talus can be avoided by carefully positioning the hinges slightly inferior to the axis of the ankle by 4–5 mm [6]. This produces a counter-push on the foot during correction and directly opposes anterior subluxation of the talus [6]. The constrained fixator allows for range of motion of the joint during contracture correction.
Fig. 11.6
An example of a constrained external fixator with hinges placed at the center of rotation of the ankle. Illustration created by and reprinted with permission of Daniel Biggers
An unconstrained or flexible frame can be used for simple, unidirectional deformities with no associated bony deformities [6] (Fig. 11.7). Frames for the correction of a simple equinus contracture require much less rigidity than those for bony instability. Consequently, this construct consists of only a tibial ring block, a calcaneal half ring, and a metatarsal half ring [6]. The use of a footplate or connecting bars between the calcaneal and metatarsal half rings is usually not needed for simple equinus correction. A single olive wire is placed in the calcaneus and in the metatarsals and attached to the respective half ring. The calcaneal wire should be placed relatively proximally and posteriorly to prevent wire cutout and to increase its biomechanical advantage [6]. Instead of building a hinge at the center of rotation like the constrained frame, the unconstrained frame allows rotation to occur naturally at the tibiotalar joint as the correction progresses.


Fig. 11.7
An example of an unconstrained external fixator for correction of an equinus deformity
The Taylor Spatial Frame™ (Memphis, TN) allows the surgeon to correct the equinus deformity around a virtual hinge (Fig. 11.8). The lateral process of the talus is generally chosen as the “origin.” In severe contractures, the tibial ring can be mounted obliquely to create a larger space posteriorly for the struts to fit. The tibiotalar joint can be distracted acutely with the frame in the operating room or the distraction can be built in to the deformity program. It is also possible to prevent anterior subluxation of the talus by accounting for it during data input in the deformity software program. A typical comprehensive spatial frame deformity program will define the deformity as plantar flexed (amount of equinus to correct), short 5–10 mm (to distract the tibiotalar joint), anteriorly translated (to prevent anterior talar subluxation), and slightly internally rotated (the ankle naturally externally rotates as it dorsiflexes).
Fig. 11.8
An example of a Taylor Spatial Frame™ used for correction of an equinus deformity. The lateral process of the talus is chosen as the origin. Illustration created by and reprinted with permission of Daniel Biggers
Postoperatively, deformity correction with the external fixator is started as soon as the patient can tolerate it comfortably. Weekly or biweekly postoperative radiographs should be taken to follow the deformity correction and to ensure that the ankle remains distracted 2–5 mm without any subluxation [6]. The equinus deformity should be overcorrected by 10°–15° if possible and held with the fixator for a minimum of 4–6 weeks further to allow for soft tissue adaptation [6]. The corrected position should be maintained with a cast for approximately 4 weeks after frame removal and with functional bracing thereafter. However, once the Ilizarov fixator is removed the deformity may recur, especially as the child grows [17]. Increasing the duration of time in the fixator does not seem to prevent recurrence [17]. Any motor imbalance should be identified and addressed with tendon transfer or bracing to try to prevent recurrence. The parents and patients should be made aware that additional procedures are most likely going to be necessary to maintain the foot in a plantigrade position as the child gets older.
Box 11.1. Equinus Deformity
Recurrence is common after equinus surgery especially in children under age 7 years.
In an external fixation construct for equinus correction, distraction must be performed first to prevent impaction of the tibia and talus.
Watch for anterior subluxation of the talus during correction of equinus with an external fixator.
The surgeon should choose the appropriate zone for soft tissue lengthening based on the physical examination, the underlying diagnosis, and the amount of equinus contracture present.
Knee Flexion Contracture
Etiology
Knee flexion contractures commonly develop in children with neuromuscular disease such as cerebral palsy. They are also associated with congenital deformities of the lower extremities such as congenital femoral deficiency, tibial hemimelia, congenital dislocation of the patella, arthrogryposis, popliteal pterygium syndrome, sacral agenesis, and certain skeletal dysplasias [18]. Knee flexion contractures are considered to be more disabling than knee extension contractures [19]. As little as 5° of extension loss can create a noticeable limp, strain the quadriceps muscle and lead to patellofemoral pain [20]. Murray and Fixsen found that only 46 % of their patients with arthrogryposis and knee flexion contractures became community ambulators whereas 89 % of the children with extension contractures did [21]. Unlike hip and ankle contractures, the other lower extremity joints or the lumbar spine cannot compensate for knee flexion contractures [22]. Hoffer et al. found that a knee flexion contracture of greater than 20° was incompatible with functional ambulation [23].
Biomechanics
In children the hinge point of the knee is defined as the intersection of the posterior femoral cortex and the physis or physeal scar [24]. Normally, the mechanical axis of the limb will pass slightly anterior to the hinge point of the knee allowing the knee to lock when the lower limb is fully extended [24]. This permits the quadriceps muscle to rest during prolonged standing [24]. In a knee flexion contracture, however, the center of gravity falls posterior to the knee. This arrangement places increasing demand on the quadriceps to resist the progressive crouch and energy expenditure increases during a crouched gait. This constant activation of the quadriceps muscle will result in fatigue and increases the oxygen cost during such pathologic gait [25]. Knee flexion contracture also functionally shortens the limb creating a gait disturbance. Consequently, a fixed knee flexion deformity exceeding 10° can lead to anterior knee pain, decreased endurance, patella alta, and progressive crouch gait in ambulatory patients [25]. In wheelchair users, knee flexion contracture may impair standing, transfers, and activities of daily living.
Clinical Evaluation
The physical examination for knee flexion contracture should focus on observation of the gait pattern from both the frontal and sagittal plane. A typical knee flexion contracture gait pattern will include greater than normal knee flexion during midstance and an inability to extend the knee fully at the end of swing phase continuing into initial contact [18]. Walking will also exhibit decreasing cadence and step length. A focused examination of the knee should include an assessment of the maximal knee extension, maximal knee flexion and the total arc of motion present (Fig. 11.9). As the range of motion is evaluated, it is important to determine if there is firm or soft endpoint to maximal knee extension. A flexion contracture of the knee with a soft endpoint will likely have an improvement from soft tissue procedures [22]. The stability of the knee should be tested and the function of the quadriceps evaluated. One relative contraindication to surgical treatment is the absence of active quadriceps function because of the high likelihood of recurrence of the flexion deformity [18, 26]. The flexibility of the hamstring muscles must be assessed and can be measured via the popliteal angle. This angle is created first by positioning the patient supine on the examining table, flexing the hip to 90° and then maximally extending the ipsilateral flexed knee. The acute angle between the vertical and maximal extension of the tibia is the popliteal angle. There is variability in measured popliteal angles with a mean value of 26° in normal children 4 years and older [18]. The examining physician must carefully assess all of the lower extremity joints for strength, spasticity and contracture. While tight hamstrings are generally the cause of a crouch knee gait, quadriceps and gastrocsoleus weakness may also lead to excessive knee flexion in stance phase [18]. A bent-knee gait may also be a compensation for equinus and toe-walking if the popliteal angle is normal [18]. The hip must also be examined because correction of hamstring contractures without addressing concomitant hip flexion contractures will lead to increased hip flexion and forward lean during gait [18]. Furthermore, distal femoral or proximal tibial deformities may create or exaggerate a knee flexion deformity. In patients with skeletal dysplasias, for example, the knee flexion deformity may be the result of bony or articular cartilage abnormalities rather than any soft tissue tightness [18]. Patients with congenital knee flexion contractures that have never reached full extension positioning may develop compensatory deformities of the distal femur and proximal tibia [19]. Syndromic and congenital contractures such as arthrogryposis are also occasionally associated with lateral displacement of the extensor mechanism and the mechanical axis [26]. Each particular problem needs to be recognized and addressed at the time of surgical correction in order to prevent recurrence.