PAINFUL HIP
Christopher G. Anton, MD
DIFFERENTIAL DIAGNOSIS
Common
Transient Synovitis
Septic Arthritis
Osteomyelitis
Slipped Capital Femoral Epiphysis (SCFE)
Legg-Calvé-Perthes (LCP)
Juvenile Idiopathic Arthritis (JIA)
Trauma
Less Common
Idiopathic Chondrolysis
Osteoid Osteoma
Osteonecrosis
Malignancy
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Age and history are helpful in narrowing differential diagnosis
Helpful Clues for Common Diagnoses
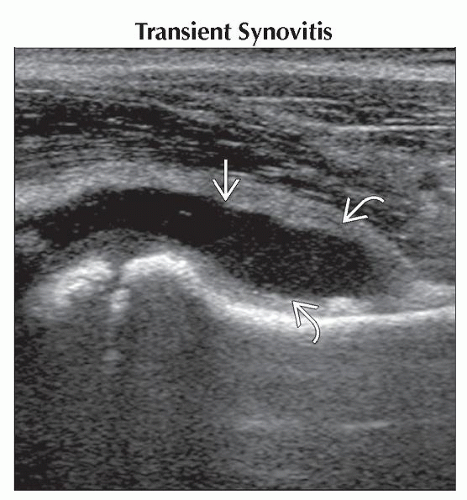
Transient Synovitis
a.k.a. irritable hip, toxic synovitis
Age: 18 months to 10 years; most common from age 4-7
Typically follows recent upper respiratory infection
Radiographs
Normal
Widening of medial joint space, lateral displacement of femoral head
70% hip effusion on ultrasound
Hip held in flexion, external rotation, and abduction, restricted abduction and internal rotation
± fever (often < 38° C)
May have mildly elevated erythrocyte sedimentation rate and white blood cell
Symptoms improve (usually within 48 hours) in 1-5 weeks
If symptoms persists beyond 1 week, consider another diagnosis
Recur in up to 17%
Legg-Calvé-Perthes develops in 1-3%
Septic Arthritis
Important to diagnose early to avoid destruction of joint
Delay in treatment ≥ 4 days results in suboptimal recovery
Age: < 4 years old
Staphylococcus aureus most common cause
Umbilical catheter, sepsis, and prior venous puncture have been implicated
Hip held in flexion
Infants can present with low-grade fever and feeding intolerance
Radiographs
Normal
Periostitis of proximal femur in neonates within days after start of symptoms
Treatment: Surgical drainage, IV antibiotics, traction
Osteomyelitis
Staphylococcus aureus most common
Streptococcus pneumonia (hypogammaglobinemia, sickle cell disease, asplenia)
Referred pain from spine or sacroiliac joints
Importance of scrutinizing spine and sacroiliac joints when imaging hips
May take up to 10-14 days before radiographs depict changes or osteomyelitis
Treatment: Abscess drainage, debridement, IV antibiotics
Slipped Capital Femoral Epiphysis (SCFE)
Salter-Harris type 1 femoral epiphyseal fracture
Age: 10-15 years old
M:F = 2:1; occurs earlier in girls
Predisposed: Obesity and endocrine disorders
Bilateral (18-36%)
Opposite side occurs within 18-24 months of 1st occurrence
Presentations: Acute, chronic, and acute on chronic
Radiographs
Widened femoral physis, medial and posterior displacement of femoral head (best seen frog leg lateral view)
Capital femoral epiphysis displacement without intersection of Klein line
Klein line: Line along lateral femoral neck and continuing toward acetabulum; ordinarily crosses small portion of femoral ossification center
Legg-Calvé-Perthes (LCP)
Osteonecrosis of femoral head of unknown etiology
Age: 3-12 years old; peak: 6-8 years old
Bilateral (10-20%)
Radiographs
Normal
Flattening, fragmentation, and sclerosis of femoral head
Key: Prognosis heavily depends on containment of femoral head
Juvenile Idiopathic Arthritis (JIA)
a.k.a. juvenile rheumatoid arthritis (JRA)
Age: < 16 years old
Symptoms with > 6 week duration
Other causes of arthritis are excluded
Stiff, swollen, painful, warm, and decreased motion in joint involved
MR: Synovitis, ± erosions, ± rice bodies
Joint space narrowing and ankylosis are late findings
Trauma
Acute (fracture) or repetitive (stress fracture) trauma
Helpful Clues for Less Common Diagnoses
Idiopathic Chondrolysis
Destruction of articular cartilage of femoral head and acetabulum
Stiffness, limpness, and pain around hip
Radiographs
Concentrically joint space narrowing, < 3 mm with osteopenia and pelvic tilt
MR: Rectangular hypointense T1 and hyperintense T2WI signal abnormality of center 1/3 of femoral head, ± ill defined within acetabulum
Osteoid Osteoma
Benign composed of osteoid and woven bone
3 types: Cortical (most common), cancellous, or subperiosteal
< 2 cm nidus surrounded by dense sclerotic bone
Most common location is femur
Age: 10-30 years old, uncommon before age 5
Classic history: Pain at night relieved by nonsteroidal anti-inflammatory agents
NECT: Depicts nidus better than MR
Bone scan: Increased flow, “double density” pattern
Intense uptake by nidus surrounded by less intense activity of reactive bone
Osteonecrosis
Most commonly located in anterolateral weightbearing portion of femoral head
T2WI: “Double line” sign
Many causes, including sickle cell disease, trauma, steroid therapy, vasculitis, Gaucher disease, hemophilia
Malignancy
Primary such as chondroblastoma
Metastatic disease: Most commonly neuroblastoma
± pathologic fracture
Image Gallery
 Longitudinal ultrasound shows a normal hip for comparison with no significant joint fluid, evidenced by a normal joint space with a concave anterior margin
 along the anterior femoral neck. along the anterior femoral neck.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|