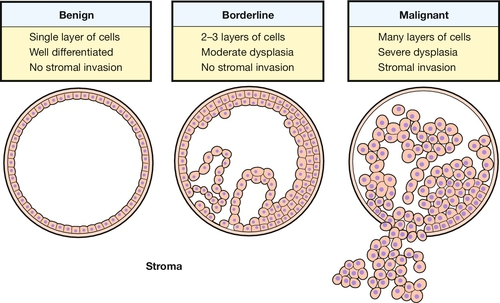
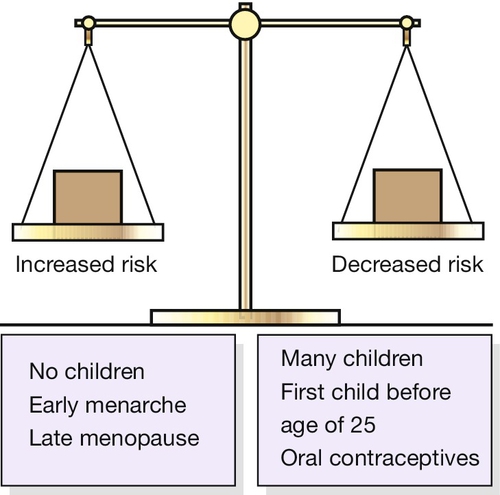
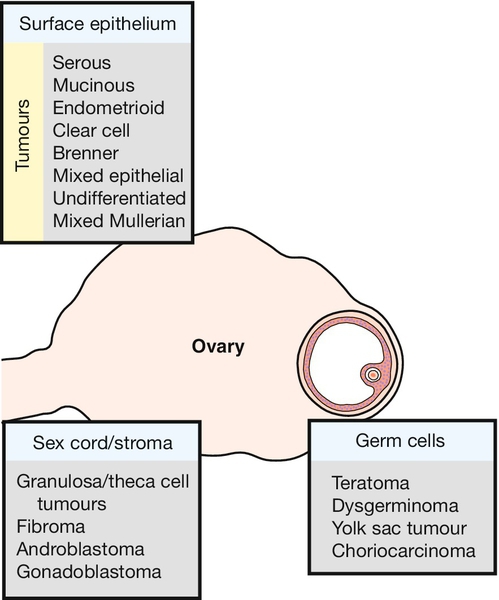
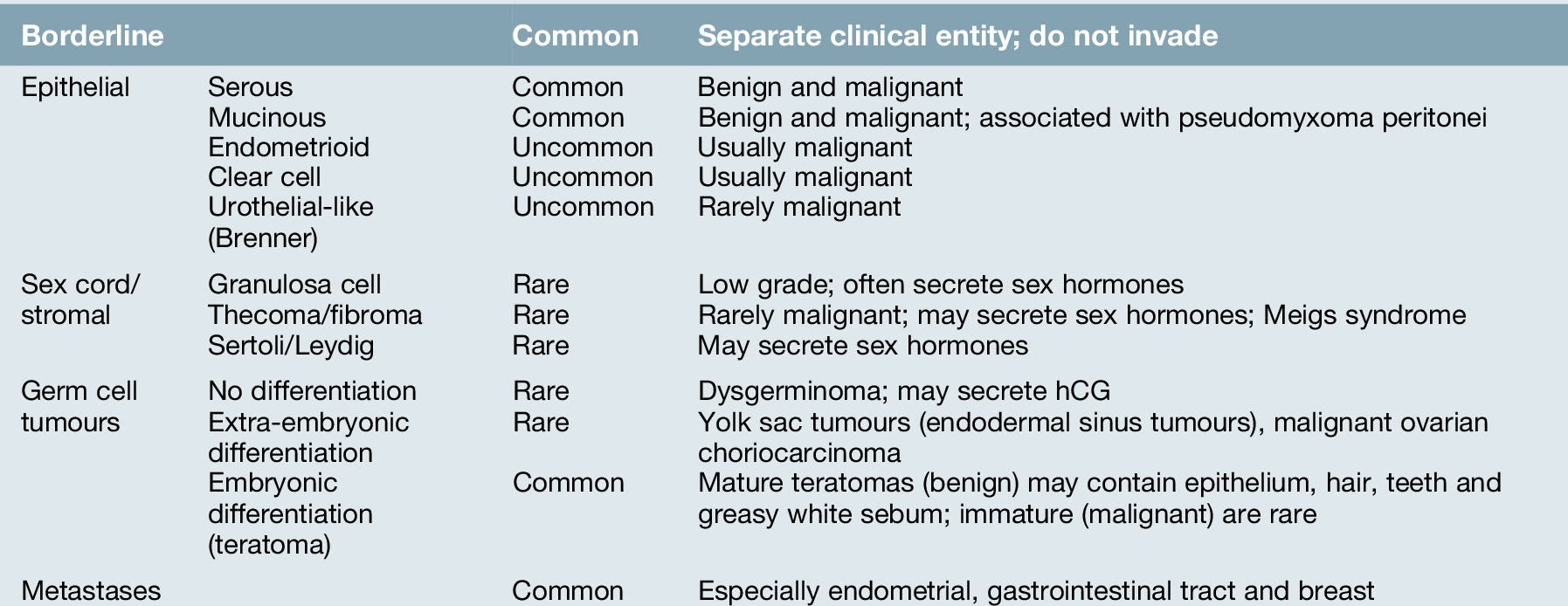
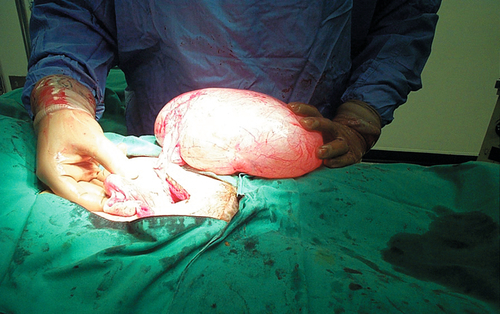
18 Ovarian cancer is the second most common of the gynaecological malignancies in most affluent countries, and the incidence is rising. In the UK, there are around 7000 newly diagnosed cases each year and approximately 4300 women annually die of the disease. The overall 5-year survival is around 40%. Ovarian cancer occurs predominantly in the fifth, sixth and seventh decades of life, with the peak age being around 75 years. Unlike cervical cancer, there is no clearly defined pre-invasive ovarian lesion. Benign, borderline and invasive tumours are recognized but these are distinct pathological entities and there is little evidence of progression from one to the other (Fig. 18.1). Indeed, there is even controversy about whether malignant epithelial tumours, which are the most common, arise from the ovary and then metastasize or arise as multicentric disease de novo. The multicentric theory is supported by the fact that ovarian-like tumours can arise in the peritoneum of women who have previously had both ovaries removed. Cancer in this case is called primary peritoneal cancer. It is entirely possible that the different types of ovarian neoplasm have differing aetiologies, particularly as germ cell tumours, which account for 25% of ovarian neoplasms, occur in much younger women than do the epithelial tumours. Reproductive history is an important determinant of epithelial ovarian cancer risk. Nulliparous women have a higher risk than parous women and the risk is inversely correlated with parity (Fig. 18.2). It is thought that the number of ovulation events in a woman’s reproductive life is the main risk factor. Overwhelming evidence now exists that women who have used the combined oral contraceptive pill at some stage in the past have a reduced risk of developing ovarian cancer. The longer the use, the lower the risk. This is again thought to be through the reduction in the number of ovulation events. In postmenopausal women, the effect of oestrogen replacement therapy has been investigated because of a reported increased risk in women who received diethylstilboestrol (a non-steroidal oestrogen) early in life. The balance of evidence, however, suggests that HRT has no significant effect on ovarian cancer risk. It has been suggested that the more often a woman ovulates, the greater the risk of ovarian carcinoma. The apparently protective effects of both pregnancy and the combined oral contraceptive pill further support this theory. The mechanism is uncertain, but it may be that repeated monthly repair of the ovarian epithelium after ovulation predisposes to malignant change. Despite this plausible theory, however, it is likely that ovarian carcinogenesis is multifactorial. It is now accepted that a genetic predisposition exists in at least a proportion of ovarian cancer cases. Although overall, there is a slightly increased risk of ovarian cancer in those with a family history, the risk is small for most categories except for those of early onset, and those with more than one affected first-degree relative. If one affected primary relative has ovarian cancer and the cancer was diagnosed when she was < 50 years old, a woman’s risk of developing ovarian cancer is around 5%. If there are two primary relatives under the age of 50 years with the disease, the risk is approximately 25%. Only 5–10% of cases of ovarian carcinoma, however, have a direct genetic association. Of particular significance in this small group are the breast–ovarian cancer tumour suppressor genes BRCA1 and BRCA2, as these are associated with a 10–50% lifetime risk of developing ovarian carcinoma. Mismatch repair genes associated with cancer of the colorectum, endometrium, stomach, urinary tract and small bowel are also responsible for a small proportion of this hereditary group. Women with such a history may warrant regular screening, and it is reasonable to consider bilateral oophorectomy after completion of their family. Such an operation will substantially reduce the risk but will not prevent primary peritoneal carcinoma. There has been controversy about the possible role of asbestos and talcum powder in the aetiology of ovarian cancer. Insufficient evidence in the form of case–control studies exists to completely dismiss reported associations. Similar problems beset the assessment of smoking, diet and alcohol consumption. Neoplasms can arise from any of the elements that comprise a mature ovary, including its surface serosal or mesothelial elements (Fig. 18.3). A number of simpler themes can be drawn from a wide diversity of tumour types, namely: epithelial tumours, which are by far the most common (70% of primary ovarian tumours); sex cord/stromal tumours; germ cell tumours; and metastatic tumours (Table 18.1). Most of the epithelial tumour types can be further broadly classified as benign, borderline or malignant. The term ‘borderline’ is reserved for tumours which display the characteristics of malignant tumours but show no evidence of invasion. Women with borderline ovarian tumours have a much better prognosis than those with frankly malignant tumours. Nevertheless, long-term survival is by no means as high as might be expected and late recurrence up to 20 years after removal of the primary does occur. Despite lacking the features of invasion, these tumours may present at an advanced stage, raising the possibility of multicentric origin. The treatment of these is predominantly surgical as they tend to be resistant to chemotherapy. Serous tumours are the most common ovarian neoplasm, accounting for almost 50% of ovarian cancers. They also account for 20% of all benign ovarian tumours, and these cases occur primarily in women of reproductive age. Serous cystadenomas (benign) are usually unilocular cysts, filled with straw-coloured fluid and of variable size (Fig. 18.4). They are bilateral in 20% of cases. Serous cystadenocarcinomas involve both ovaries in over 50% of cases and may have both cystic and solid components. Psammoma bodies, concentrically laminated calcified concretions, are a frequent histological finding. These comprise 20% of all ovarian tumours and less than 10% are malignant. Benign tumours are usually unilateral and only 20% of malignant tumours are bilateral. Mucinous tumours are usually multiloculated and contain mucinous fluid of variable viscosity. They are generally the largest of the common epithelial tumours. Uncommonly, concomitant pseudomyxoma peritonei may be present. There is characteristic gelatinous tumour within the peritoneal cavity. It is unclear to what extent pseudomyxoma peritonei truly arises from the ovary rather than from a primary mucinous tumour of the appendix. Endometrioid tumours are usually malignant and closely mimic endometrial cancer in histological appearance. In around 30% of cases there is a coexistent second primary in the endometrium. These are virtually all malignant and may be a variant of endometrioid tumours. They are the most frequent epithelial tumour found in association with ovarian endometriosis. It must be emphasized however, that ovarian cancer developing from endometriosis is uncommon. Urothelial-like or Brenner tumours (history box) are uncommon, usually unilateral and rarely malignant. They in part comprise epithelium of urothelial type but their main component is ovarian stroma. A rare aggressive variant is the urothelial or transitional cell carcinoma.
Ovarian neoplasms
Introduction
Natural history
Aetiology
Reproductive history
Exogenous oestrogens
Oral contraceptives
Hormone replacement therapy (HRT)
Repeated (incessant) ovulation
Genetic factors
Other factors
Pathology
Borderline tumours
Epithelial tumours
Serous tumours
Mucinous tumours
Endometrioid tumours
Clear cell tumours
Urothelial-like tumours
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree