American women without a family history of the disease is 1 in 70 (1.4%). Because early ovarian cancer produces few specific symptoms, most women present with advanced-stage disease for which the cost of treatment is high and the prognosis poor. Approximately 90% of malignant ovarian tumors in adults are of epithelial origin followed by sex cord-stromal tumors (6%) and germ-cell tumors (3%). Good surgery is a blend of good judgment and sound surgical technique. Much of this chapter is devoted to the natural history and results of various surgical and other treatment approaches for ovarian cancer. This background information provides the surgeon with the basis for clinical decision making concerning patient selection, choice of the right operation, and postoperative treatment recommendations. The operative techniques involved in surgery for ovarian cancer are illustrated in many of the other chapters in this text.
TABLE 53.1 Risk Factors for Ovarian Cancer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
and this effect can be blocked by luteinizing hormone (LH). A corollary to this hypothesis is that elevated circulating gonadotropin levels promote estrogen biosynthesis in the ovarian stroma, which, in turn, causes abnormal proliferation of the adjacent epithelium. Breast-feeding, which has been reported to lower the risk of ovarian cancer, is associated with reduced serum concentrations of LH and estradiol. Pregnancy and the use of oral contraceptives presumably lower the risk of ovarian cancer by inhibiting pituitary secretion of gonadotropins. This theory also receives support from the observed increased risk of ovarian cancer in women taking fertility drugs because these drugs stimulate ovulation by increasing levels of FSH, particularly in the follicular phase of the cycle.
no evidence of an ovarian abnormality. The characteristics of malignant cells present in ascitic fluid may help identify the primary site of intra-abdominal malignancy. An electrocardiogram is indicated in all women older than age 40 or in a patient with specific signs or symptoms of cardiac disease.
TABLE 53.2 Serum Markers in Ovarian Cancer | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
with stage III or IV ovarian cancer. The incidence of lymph node metastases increased from 20% in well-differentiated ovarian cancers to 65% in poorly differentiated tumors and was higher in serous ovarian malignancies than in mucinous or endometrioid cancers.
TABLE 53.3 Lymph Nodal Metastases in Patients with Clinically Apparent Stage I Epithelial Ovarian Cancer | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Although there are numerous grading systems for ovarian cancers that use both architectural and nuclear features, it is recommended that four grades be used, with grade 4 (undifferentiated) applied to tumors with minimal or no differentiation. Recommendations concerning the use of special staining techniques or flow cytometry in establishing the correct histologic diagnosis of ovarian tumors are made in the CAP report. Immunohistochemical staining of ovarian tumors for cytokeratin 7 (CK7) and cytokeratin 20 (CK20) is helpful in differentiating primary mucinous ovarian carcinoma from colorectal adenocarcinoma that has metastasized to the ovary. Colorectal adenocarcinomas usually stain positively for CK20 and negatively for CK7. In contrast, ovarian carcinomas usually stain negatively for CK20 and positively for CK7.
TABLE 53.4 World Health Organization Histological Classification of Ovarian Tumors | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
The volume of ascitic fluid should be recorded, and a minimum of 25 mL should be sent for cytologic evaluation.
In the absence of ascites, separate saline washings should be obtained from the (a) pelvic cul-de-sac, (b) right paracolic space, (c) left paracolic space, and (d) undersurface of each hemidiaphragm. Approximately 100 mL of saline should be instilled in each of these areas, recovered, and sent for cytologic evaluation.
TABLE 53.5 FIGO Ovarian Cancer Staging (January 01, 2014)
STAGE I: Tumor confined to ovaries
OLD
NEW
IA
Tumor limited to 1 ovary, capsule intact, no tumor on surface, negative washings/ascites
IA
Tumor limited to 1 ovary, capsule intact, no tumor on surface, negative washings
IB
Tumor involves both ovaries
IB
Tumor involves both ovaries otherwise like IA
IC
Tumor involves 1 or both ovaries with any of the following: capsule rupture, tumor on surface, positive washings/ascites
IC Tumor limited to 1 or both ovaries
IC1
Surgical spill
IC2
Capsule rupture before surgery or tumor on ovarian surface
IC3
Malignant cells in the ascites or peritoneal washings
STAGE II: Tumor involves 1 or both ovaries with pelvic extension (below the pelvic brim) or primary peritoneal cancer
OLD
NEW
IIA
Extension and/or implant on uterus and/or fallopian tubes
IIA
Extension and/or implant on uterus and/or fallopian tubes
IIB
Extension to other pelvic intraperitoneal tissues
IIB
Extension to other pelvic intraperitoneal tissues
IICa
IIA or IIB with positive washings/ascites
STAGE III: Tumor involves 1 or both ovaries with cytologically or histologically confirmed spread to the peritoneum outside the pelvis and/or metastasis to the retroperitoneal lymph nodes
OLD
NEW
IIIA
Microscopic metastasis beyond the pelvis
IIIA (Positive retroperitoneal lymph nodes and /or microscopic metastasis beyond the pelvis)
IIIA1
Positive retroperitoneal lymph nodes only
IIIA1(i) Metastasis ≤ 10 mm
IIIA1(ii) Metastasis > 10 mm
IIIA2
Microscopic, extrapelvic (above the brim) peritoneal involvement ± positive retroperitoneal lymph nodes
IIIB
Macroscopic, extrapelvic, peritoneal metastasis ≤2 cm in greatest dimension
IIIB
Macroscopic, extrapelvic, peritoneal metastasis ≤2 cm ± positive retroperitoneal lymph nodes. Includes extension to capsule of liver/spleen
IIIC
Macroscopic, extrapelvic, peritoneal metastasis >2 cm in greatest dimension and/or regional lymph node metastasis
IIIC
Macroscopic, extrapelvic, peritoneal metastasis >2 cm ± positive retroperitoneal lymph nodes. Includes extension to capsule of liver/spleen
STAGE IV: Distant metastasis excluding peritoneal metastasis
OLD
NEW
IV
Distant metastasis excluding peritoneal metastasis. Includes hepatic parenchymal metastasis.
IVA
Pleural effusion with positive cytology
IVB
Hepatic and/or splenic parenchymal metastasis, metastasis to extra-abdominal organs (including inguinal lymph nodes and lymph nodes outside of the abdominal cavity)
a Old stage IIC has been eliminated.
Other major recommendations are as follows:
• Histologic type including grading should be designated at staging.
• Primary site (ovary, fallopian tube, or peritoneum) should be designated where possible.
• Tumors that may otherwise qualify for stage I but involved with dense adhesions justify upgrading to stage II if tumor cells are histologically proven to be present in the adhesions.
Reprinted from Prat J, for the FIGO Committee on Gynecologic Oncology. Staging classification for cancer of the ovary, fallopian tube and peritoneum. Intl J Gynecol Obstet 2014;124:1-5. Copyright © 2013 International Federation of Gynecology and Obstetrics. Published by Elsevier Ireland Ltd. All rights reserved. Reprinted with permission from Elsevier.
TABLE 53.6 Surgical Staging of Apparent Early-Stage Ovarian Cancer
Vertical midline incision
Evacuation of ascites or multiple cytologic washings
Complete abdominal inspection and palpation
Resection of ovaries, fallopian tubes, and uterusa
Omentectomy
Random peritoneal biopsies
Retroperitoneal lymph node sampling
a Exceptions may be made in selected patients who wish to preserve fertility.
The ovarian tumor should be inspected, with particular attention to the presence of papillary excrescences on the surface or rupture of the capsule. The contralateral ovary and uterus should be examined for the presence of metastatic tumor. The pathways of ovarian tumor should be removed and sent for frozen section examination. Removal of the opposite ovary and/or uterus is dependent on several factors and is discussed on the following pages.
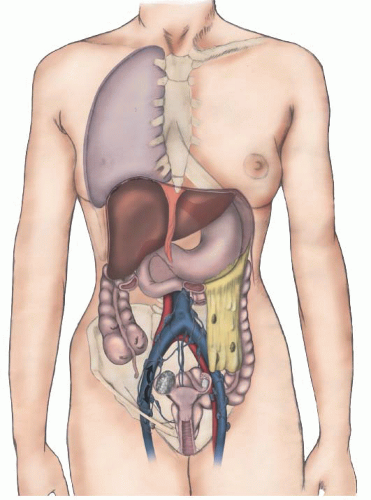
Careful inspection and palpation of the peritoneal surfaces and intra-abdominal viscera should be performed. This evaluation should be approached in a systematic fashion, beginning with the peritoneum of the cul-de-sac and small bowel mesentery. Inspection should continue with the ascending colon, liver, omentum, undersurface of the right and left hemidiaphragms, and stomach. Finally, the transverse colon, spleen, descending colon, and bladder peritoneum should be evaluated.
All areas suspicious for malignancy should be biopsied. In the absence of visible disease, biopsies should be taken of the cul-de-sac peritoneum, bladder peritoneum, both lateral pelvic walls, paracolic peritoneum bilaterally, and undersurface of the right hemidiaphragm. An infracolic omentectomy should be performed in patients with epithelial ovarian cancer and an omental wedge biopsy taken in patients with germ-cell or stromal tumors. Appendectomy should be performed in all patients with mucinous epithelial cancers involving the ovary. Primary appendiceal cancers, although rare, commonly spread to the ovaries and usually require right hemicolectomy as part of initial surgical staging.
As has been mentioned, ovarian cancer commonly spreads to both pelvic and paraaortic lymph nodes. Some patients with early-stage ovarian cancer have paraaortic lymph node metastases in the absence of pelvic lymph node spread. Therefore, these lymph node groups should be sampled separately in all patients. It is important that sampling include lymph nodes on the opposite side of the primary ovarian tumor, because isolated contralateral spread has been reported. In the setting of advanced-stage disease, prospective randomized trials reviewed by Panici et al. have shown that routine lymphadenectomy is not associated with a higher survival rate; however, it is associated with an improvement in the disease-free interval.
Finally, it should be emphasized that operative findings present at the time of staging must be carefully documented. Prognosis is related to the site and volume of metastatic tumor, as well as the amount of residual disease remaining after surgical debulking. Important data concerning the location and size of tumor metastases are often lost if the details concerning operative staging are not recorded.
TABLE 53.7 Criteria for Potential Fertility-Sparing Surgery in Ovarian Cancer Patients | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree