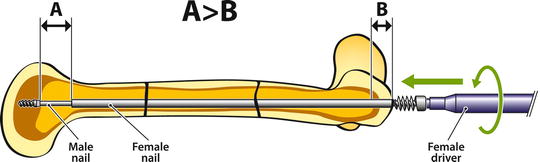
Fig. 16.1
The medullary canal on the AP view (a) is smaller than on lateral view (b)
Consequence: Measuring the size of the implant on the lateral view of the deformed bone may lead to an over optimistic size for a rod and intraoperative problems (fracture).
One fundamental aspect of OI bone surgery is that the child needs more bone than metal: Reaming to enlarge the medullary canal should be limited as it removes bone, and a large implant takes most of the stress in the bone which disappears around the rod. This is a very challenging situation. Prevention is the best way to deal with this problem.
The bone deformity is (like scoliosis) a 3D problem. The 2D pre-op imaging (AP and LAT of the affected bone) gives a limited understanding of the complexity of the deformity. Intraoperatively, prior to making an incision, it is useful to analyze the bone deformity with fluoroscopy: it allows to define precisely the apex (or apices) of the deformity (or deformities) and choose wisely where to perform the osteotomy (or osteotomies).
Soft Tissue Problems
Soft tissues play an important role in the development of bone curvatures in OI. During growth, the soft tissue resists the elongation of the bone. The tether effect leads to a pattern of deformities defined by the most important muscle groups.
In the femur, the posteromedial hamstrings are the most resistant muscles, and therefore the femur bows anterolaterally. In the tibia, most muscles are posterior and lateral, hence the anteromedial bow of the tibia. This “rule” can be modified according to the antenatal position of the fetus: for instance, a child with OI born in a breech position may be born with a recurvatum deformity of the femur due to the extended knee with a flexed hip.
These soft tissues problems can, and will cause difficulties at the time of surgical correction of the deformities. Generally speaking beyond 60° of angulation, it is advisable to shorten the bone (closing wedge resection) to be able to straighten the bone without too much tension in the muscles.
Two important points to check prior to surgery: (1) correction of coxa vara: the amount of free adduction preoperatively gives the amount of possible skeletal correction (adduction test); (2) if the foot is in equinus prior to correcting procurvatum tibial bow, this equinus will be worse at the end of the correction. In such a case, a shortening of the tibia can be done at the time of the osteotomy. A tendo Achilles lengthening can also be done at the end of the procedure.
Before Surgery
At our center, most patients with severe OI receive bisphosphonates soon after birth. Intravenous Pamidronate is the most widely used treatment in North America. Zoledronate is progressively replacing Pamidronate as it is more potent and is administered only twice a year. The acute complications of the bisphosphonates include a flu-like reaction in most children at first cycle treatment as well as risk of hypocalcaemia (significant respiratory distress has been reported in children with preexisting respiratory compromise [3]). Fracture healing does not seem to be affected by the administration of bisphosphonates while osteotomy healing (slow remodeling process) is often delayed. Therefore, no bisphosphonates are given postoperatively (see Box 16.3).
The patient/family must be aware of the risks of complications that can be seen with any type of surgery but also specific complications related to the OI:
Anesthesia: There is a risk of malignant hyperthermia [4, 5] during surgery, even though a recent paper [6] comparing patients with OI and those without OI did not find a difference between the two groups.
Difficult intubations (big head, big tongue).
Ventilation problems (deformed thorax).
Fracture: The risk is always present during the transfer of patient, while finding an IV access, positioning on the OR table, and during the surgical manipulations.
Neurologic complications (patients with Type III OI may have hydrocephalus).
Hemorrhage.
Surgical Correction
Why?
A deformed bone (particularly when weak due to OI) loses its biomechanical properties and is likely to break at the apex of the deformity. Usually the deformity gets worse after a fracture, leading to a vicious circle of fracture/deformity/fracture.
When?
Rodding before walking age is technically more difficult, implant size is reduced and postoperative rehabilitation can be challenging. Since the introduction of bisphosphonates, stronger bones can be obtained in a few months, and therefore there is no need to operate on children before walking age.
How?
“Guided growth” with hemi-epiphysiodesis using non-locking plates or staples is quite popular for managing angular deformities of the lower extremity in children. This technique is very effective when the angulation originates close from the growth plate; and the growth plate has a normal growth potential. It is unlikely to work on a diaphyseal angulation like OI, and with a limited function of the growth plate. Therefore, the indications of hemi-epiphysiodesis in OI are relatively rare. A recent paper from Yilmaz and collaborators [7] demonstrates the safety and effectiveness of “guided growth” in patients with skeletal dysplasias. No case of OI is reported in this series.
The use of IM rods was proposed by Sofield and Millar in 1959 [1]. The rod acts as a tutor in the bone, preventing progressive deformity during growth. It reduces the fracture rate, and if a fracture happens, it eases the treatment, preventing the displacement of the bone fragments.
Application of plates is generally not indicated in patients with OI, since the plate creates a rigid segment and the bone is likely to break above or below the implant [8]. Furthermore, under the plate, the bone is not submitted to any stress and resorbs (Fig. 16.2).
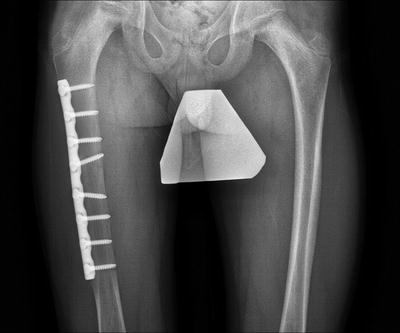
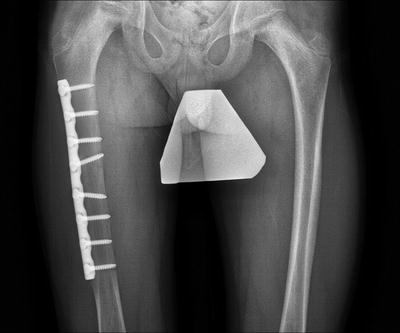
Fig. 16.2
Type I OI, resorption of the bone at the level of the plate, particularly the medial cortex
Different Types of Rods Can Be Used in OI Bones
Regular rods (such as K-wires, Rush rods, elastic nails) have the advantage of being readily available, relatively inexpensive and come in varying diameters from 1 mm up (K-wires). The Telescopic rods introduced by Dubow-Bailey [9] have been modified by Sharrard [10] Karbowski [11] and more recently by Cho [12]. A new concept of telescopic rod, without the need for arthrotomies has been described by the author [13] with short term promising results. These implants are more expensive, need to be ordered (and currently not available in all countries), and the smallest diameter is 3.2 mm, which is sometimes too large for small children. The major advantage of telescopic (or growing rods) is that the implant gets longer as the child grows, reducing the need for reoperation (which is needed every second or third year with non-telescopic rods because the bone deforms under the tip of the nail during growth) (Fig. 16.3). If a telescopic rod is not available, it is also possible to use “sliding rods”: two regular rods (Rush or elastic nails) are inserted: one from proximal epiphysis-distally, and the other rod from the distal epiphysis-proximally. As each of the two rods are inserted from a distinct epiphysis, these implants move away of each other during growth. Unfortunately, they do not provide the same stability as telescopic nails, and it is common to see the bone deform during growth (Fig. 16.4). In their report [14] Laville and Al concluded that sliding rods were not superior to telescopic rods.



Fig. 16.3
Type III OI, deformity of the femur under the tip of the nail with progressive migration through the cortex

Fig. 16.4
Sliding rods. (a, b) After 4 years, progressive varus deformity aggravated by a proximal femoral fracture (b)
Open or Percutaneous Osteotomy?
The growing trend for minimally invasive surgery in orthopedics is beneficial, as it results in less scars and decreased soft tissue trauma (including less blood loss and less postoperative pain); but is technically more demanding. For the femur: before the era of bisphosphonates, OI bone was extremely brittle, but it was easier to do a percutaneous osteotomy, or even an osteoclasis. Since most patients receive bisphosphonate before surgery, the surgeon must be aware that the bone which is harder will break suddenly and not necessarily at the desired place! The amount of preoperative deformity as well as the absence of a medullary canal on X-rays should lead the surgeon to prefer the “open” technique in selected cases.
For the tibia: because of the soft tissue problem (relative equinus deformity) it is better in most cases to do an open, closing wedge osteotomy. It allows appropriate shortening of the tibia so that the foot will be plantigrade following surgical correction.
Note: Author’s preferred method: Whenever possible, I use percutaneous surgery for the femur, but if after 15–20 min, I am not able to reduce the osteotomy and realign the bone, I switch to the open technique.
The relative contraindications for percutaneous femoral osteotomies are as follows:
Angulation > 60°.
No medullary canal seen on X-rays.
Osteotomy
The use of an oscillating saw for performing the osteotomy in patients with OI is not recommended: It burns the bone ends, and as these patients receive bisphosphonates (which reduces the number of osteoclasts), the remodeling is slow. It takes time to remove the dead bone and this may lead to delayed union or non-union. It is better to use osteotomes (after preparing the bone with a few drill holes) and clean the bone ends (in the open technique) with a rongeur.
Reduction after osteotomy: the soft tissue tightness is here again a challenge. If there is too much tension at the osteotomy site, do not fight with OI bone! Just shorten as much as necessary to get a good alignment without too much tension.
Note: At the time of reduction, I usually ask the anesthetist to give adequate muscle relaxation to the patient for a few minutes, allowing a smooth manipulation of the bone fragment. If the bone breaks, it may just be a split of one of the fragments: cerclage technique (with resorbable suture) is often sufficient. If the bone bursts in multiple fragments, it may be best to postpone rodding and leave the patient in skin traction for a few weeks.
Do not accept poor alignment as it will likely increase overtime. In the femur, if the nail is too anterior distally, it will perforate the cortex (see Fig. 16.3a). It is easy to do a percutaneous distal metaphyseal osteotomy to be able to center the rod in the middle third of the epiphysis (for telescopic rods) on both frontal and sagittal planes.
In the tibia, the deformity is most exclusively in procurvatum, particularly in the distal tibia. It is advisable to overcorrect to 5–10° of recurvatum to slow down the recurrence of the deformity during growth.
Technique for Femoral Rodding (see Box 16.1)
With an open osteotomy through a posterolateral approach, it is simple to ream the medullary canal to the appropriate size of nail. (Remember that the child needs more bone than metal; avoid excessive reaming!)
If the implant is to be a Rush nail; its introduction through the tip of the greater trochanter (GT) is facilitated with the retrograde insertion of a K-wire that is used as a guide.
Note: The author has modified his own K-wires so that the tip on the blunt end is “cup-shaped” allowing a better contact between the nail and the K-wire guide (Fig. 16.5).


Fig. 16.5
Modified K-wires to serve as guide to introduce a Rush nail
The length of the nail should be calculated from the tip of the GT (or the ossified proximal metaphysis) to the intercondylar notch. Pushing the nail through the growth plate (often the strongest part of OI bone) helps stabilizing the nail which is often “floating” in an empty metaphysis. As long as just one attempt of placing the nail through the growth plate is done, epiphysiodesis is unlikely to occur. For the use of the elastic nails, the original technique was described [15] for normal bones and the entry point is in the metaphysis. The technique has been adapted by Metaizeau for OI bones with a retrograde nail introduced through the epiphysis distally, and an antegrade nail inserted through the greater trochanter. Both nails “slide” away of each other during growth [16]. For sliding rods, care must be taken for the distal rod to be anchored in the epiphysis without disturbing the knee motion. The tip of the rod must be bent and embedded.
The Fassier-Duval telescopic rod is inserted also from the GT and the introduction of the male driver is done first: A K-wire (same diameter as the male nail) is pushed up in the buttock from the osteotomy, and the male driver is pushed down on the K-wire as a guide. When the driver is at the level of the osteotomy, the K-wire is removed and replaced with the nail. After reduction of the osteotomy, the male nail is pushed down in the shaft until it reaches the growth plate, and screwed in the epiphysis. C-arm control of the position in the bone is important: the nail should be in the middle third of the epiphysis both on AP and lateral. It is relatively simple to be centered on AP but in lateral, any mild bow of the femur will drive the nail to be too anterior. In such a case, the nail is withdrawn a few centimeters, a percutaneous metaphyseal osteotomy is done and the nail is pushed in the center of the epiphysis (Fig. 16.6 and Box 16.4). The male driver is removed while maintaining pressure on the nail to avoid dislodging it. The female nail is measured, from the ossified proximal femoral metaphysis to 1 cm above the distal femoral growth plate. The threads of the female nail being left above the ossified metaphysis of the proximal femur (see Fig. 16.6). (The measurement of the nail length does not take the threads of the female nail into consideration.) When the female nail has been cut (Midas Rex®) and the lumen of the nail cleaned to allow a smooth telescoping; the female nail is pushed down over the male nail. At the moment the proximal end of the nail disappears inside the wound, a careful X-rays measurement is done to verify that the distance between the distal end of the female nail and the “aisles” of the male nail (“A” on Fig. 16.7) is greater than the distance between the proximal threads of the female nail and the proximal metaphysis (“B”). If “B” is greater than “A”, while screwing the female nail in the non-ossified GT, one will push the male nail into the knee joint. The male nail is cut above the female and the smoothness of the section checked with a little probe to ensure that the male nail slides smoothly distally during growth.