FIGURE 47-1 Preoperative radiograph of upper arm and forearm of a 4-year-old child with distal ulnar OCE and a marked dislocation of the radial head.
CLINICAL QUESTIONS
- What is the inheritance pattern of multiple hereditary exostoses (MHE)?
- What are the gene mutations responsible for OCE formation?
- What is the natural history of MHE?
- What are the indications for surgical excision of an OCE?
- Will excision of an OCE restore skeletal growth?
- What are the expected outcomes from excision of an OCE?
- When is an ulnar lengthening indicated?
- When is creation of a single bone forearm indicated?
- What are the complications associated with surgical reconstruction of an imbalanced forearm and wrist with osteochondromatosis?
- What is the risk of malignant degeneration with an OCE?
THE FUNDAMENTALS
Etiology and Epidemiology
Arising from juxtaphyseal regions, OCEs are the most common (20% to 50%) type of bone tumor. The differential diagnosis includes metachondromatosis, dysplasia epiphysialis hemimelia (Trevor disease),1 multiple enchondromatosis (Ollier disease), and malignancies, among others. OCEs can either be solitary or multiple. Known also as multiple osteochondromatosis, multiple cartilaginous exostoses, and diaphyseal aclasis, among other synonyms, multiple hereditary exostosis (MHE) is typically (~80% of cases) an autosomal dominantly inherited disease associated with mutations in tumor suppression genes (EXT1 and EXT2) that are required for heparan sulfate synthesis. Specifically, these EXT1 and EXT2 mutations lead to defective glycotransferases and altered endochondral ossification by abnormal chondrocyte proliferation and maturation.2 The OCE lesions begin as microchondromas within the periosteum adjacent to the normal physis, in the groove of Ranvier.3 Of note, metachondromatosis and dysplasia epiphysialis hemimelia are not due to abnormalities of the EXT pathway.4
The incidence of OCE is on average 1 to 2:100,000 live births but varies greatly depending on the genetic pool in specific geographic regions. Patients and families with EXT1 have a more severe phenotype than EXT2 patients. The EXT1 patients have more lesions, more severe deformities, more short stature, more length discrepancy in involved bones, and more involvement in flat bones and undergo more operations than other EXT subtypes.5–7 The EXT1 patients are also more at risk for malignant degeneration of an OCE lesion, as are patients with Maffucci syndrome (enchondromas and hemangiomas). The overall risk of malignant degeneration is about 2% for MHE patients.8 Sequencing differentiation of the EXT1 and EXT2 mutations in individual pedigrees is ongoing in many diverse ethnic families with MHE and will provide more definitive, patient-specific information in the future.
Clinical Evaluation
Patients with solitary OCEs usually present when the lesion is large enough to be palpated. This is often during an accelerated growth phase, such as during the preado-lescent growth spurt. The presence of a firm mass raises a serious concern over malignancy by parents, providers, and patients. The parental and patient worry about a possible cancer is often the “elephant in the room,” and addressing this grave concern of theirs promptly is a great relief to patients and families.
Patients with MHE usually present earlier because their genetically aware parents will repeatedly examine their children for lesions. The severe EXT1 pedigrees will have lesions at younger ages, some present in infancy and even in flat bones such as ribs. Digital malalignment and a prominent finger mass arising from the phalangeal articular cartilage can occur in infancy with an EXT1 patient. The ratio of ulnar length to patient height has been used to distinguish EXT1 and EXT2 patients.9
Restricted and/or painful joint motion; long bone deformity; growth discrepancy of involved bones; joint subluxation; and impingement symptoms of neurovascular structures, muscles, and/or tendons are common complaints of patients with an OCE and MHE.10 The lesions will increase in size with growth, and, therefore, complaints and problems are common in children over the age of 10 years.11 In essence, pain (~80% of patients) is their most common complaint since it is frequent and directly impacts the daily function of many patients.12
The most common upper limb problem with OCEs is forearm and wrist deformity that impairs function. Involvement of the distal ulna is common and can lead to relative shortening of the ulna compared to the radius. If the growth discrepancy is marked, there will be (1) increased radial articular inclination, (2) ulnar deviation of the hand, (3) ulnar and proximal translocation of the carpus, and (4) increased radial diaphyseal bowing and/or proximal radial head dislocation.13 The shorter the ulna relative to the radius, the more loss of motion and function will occur.14
Hand involvement with MHE is common with juxtaphyseal lesions in metacarpals, proximal and middle phalanges. There are often more than 10 hand lesions per MHE patient that result in brachydactyly and less commonly angular deformity.15 Distal phalanx and thumb involvement are rare. Unusual presentations in the hand include mallet finger, nail plate deformity and intra-articular OCEs.
Winging of the scapula, crepitus, and/or pain can be the presentation for anterior scapular OCEs.16 Rarely these can be palpated by exam or seen on plain radiographs. A computed tomography (CT) or magnetic resonance imaging (MRI) scan will be diagnostic. Proximal humeral OCEs are common since approximately 80% of the growth of the humerus is at the proximal physis. These lesions will initially hide under the deltoid. Later, with growth, they can become more prominent. Local impingement can cause functional pain and limit both motion and strength.
One of the most worrisome clinical features is an intra-spinal OCE that leads to spinal cord compression.17 This occurs in <1% of MHE patients. The most common regions are upper cervical (C2), upper thoracic (T4–T8), and base of skull. Plain radiographs may reveal the lesion but often these intraspinal lesions are small. Neurologic exam with clonus, increased reflexes, and positive Babinski signs is diagnostic of myelopathy, and assessing for this should be a part of all annual and preoperative physical exams. Spinal cord imaging with tomograms, myelograms, or more commonly now MRI and thin-slice CT scans is diag-nostic.18,19 Surgical removal of the intraspinal OCE before progressive myelopathy or complete neurologic loss, such as under anesthesia for elective surgery for other reasons, is strongly recommended.20
There are several clinical classification systems for MHE patients. The forearm can be used to gauge the severity of total body MHE and the risk of malignant degeneration. Taniguchi defined three groups: group I, no involvement of the distal forearm; group II, involvement of the distal forearm without shortening of the radius or ulna; and group III, involvement of the distal forearm with shortening of the radius and/or ulna.21 Group I was mildly affected, and group III had axial and severe appendicu-lar skeleton involvement and was most at risk for malignant degeneration. Masada classified forearm deformity by group I, ulnar shortening and radial bowing due to a distal ulna OCE; group II, dislocation of the radial head due to an OCE of the proximal radius (IIA) or distal involvement (IIB); and group III, relative radial shortening due to a distal radius OCE.22 Radiographic parameters on the anteroposterior (AP) view to measure the degree of deformity include radial articular angle, carpal slip, ulnar variance, and forearm to third metacarpal angle. Ulnar variance in the skeletally immature requires measurement of the radial metaphysis to the ulnar metaphysis.23
Malignant degeneration of OCEs is a risk in approximately 2% of MHE patients24 and is higher in EXT1 patients.25 These patients, especially those with EXT1 gene mutations, clearly need to be made aware of the possible occurrence and followed expectantly. In some populations, serial bone scans have been used to monitor lesions.26 Worsening pain or increased size of a lesion in adulthood is serious cause for concern. The size of the cartilaginous cap is a factor, with a cap thicker than 2 cm being high risk for chondrosarcoma. Cartilaginous cap size discrimination can be determined with a high degree of accuracy by both MRI and CT scans.27 Positron emission tomography scans can aid in diagnosing malignant chondrosarcomas, local recurrence, and metasta-ses by the metabolic activity of the lesion(s).28 In the end though excisional biopsy is indicated for suspicious lesions.
Surgical Indications
The presence of a mass alone is not an indication for surgical excision of an OCE. Otherwise, patients with MHE would have aggressive and frequent surgeries for both primary and secondary resections. The presence of pain associated with an OCE is an indication for surgery, understanding that pain is relative. Resection of a painful OCE provides pain relief in more than 90% of patients.
Excision of an OCE to prevent growth deformity is more controversial.29 In the forearm, excision of a solitary OCE on one of the two bones can restore and improve growth. If OCEs are present on both the distal radius and ulna, growth restoration does not occur with simple excision.
Surgery to correct deformity and/or length discrepancy is indicated when there is marked deformity, painful restriction of motion, and functional deficits. Surgery has to be compared with natural history, as adults with OCEs, growth discrepancy, and upper limb deformity can be pain free and functional.30–32 There is clear evidence that symptomatic patients can obtain pain relief, improved motion of wrist and forearm, and aesthetic enhancement with forearm rebalancing surgery.13,33–36 Forearm rebalancing is usually a combination of OCE excision, distal radial osteotomy or temporary growth retardation on the radial side of the distal physis, and ulnar lengthening (by singlestage or distraction osteoclasis). Reconstructive procedures performed at an early age often require reoperation with growth. The ability to successfully reduce and maintain reduction of a dislocated radial head is controversial. A dislocated radial head, especially in a very young patient, for us is an indication for single bone surgery.37,38
SURGICAL PROCEDURES
 Excision of OCE
Excision of OCE
Common symptomatic sites in the upper limb are (1) distal ulna with impingement against the radius, limiting motion and causing pain (Figure 47-2); (2) proximal humerus causing impingement and pain (Figure 47-3); and (3) distal radius with compression and contact pain. Other less common sites and indications are (1) anterior scapula with winging, crepitus, and painful motion; (2) metacarpal or phalanx with pain and at times angular deformity (simultaneous corrective osteotomy may be indicated); and (3) an intra-articular OCE in infancy with limited motion and angular deformity (see Figure 6-8).

FIGURE 47-2 Large OCE of the distal ulna with foreshortening ulna and mild deformity of radius in response to OCE impingement.
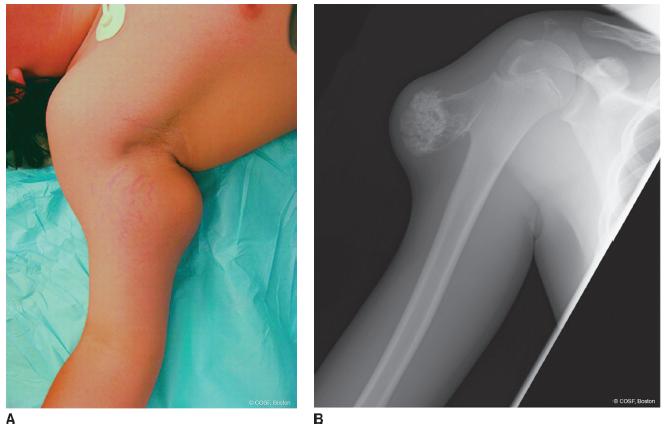
FIGURE 47-3 A: Clinical photograph of large OCE of the proximal humerus with painful impingement. B: Radiograph of similar proximal humeral OCE except on lateral rather than medial side.
Exposure of the symptomatic OCE is made considering the neighboring neurovascular bundles and cutaneous nerves. Frequently, the local nerves and arteries are displaced from their native anatomic sites by large, symptomatic OCEs, for example, ulnar nerve and artery by a large, volar distal ulnar OCE (Figure 47-2) and radial, axillary nerve(s) or brachial plexus by proximal humeral OCEs (Figure 47-4). The incision needs to be sufficiently extensile to perform a careful excision of the entire cartilaginous cap and OCE while protecting not only the neurovascular bundles but the physis as well. If there is a concern about a malignant degeneration, surgery should be performed with or by an orthopaedic oncologist, so the incisions and dissection do not jeopardize limb salvage. Circumferential dissection around the base of the OCE is performed with elastic loops or gentle retractors mobilizing the neurovascular bundle. Once the entire base, body of the OCE, and cartilaginous cap are isolated (Figure 47-5), the periosteum is incised with electrocautery, and excision is performed with an appropriate-size curved osteotome. (Rongeuring of the sharp edges of the base is performed to prevent further impingement and persistently symptomatic bony prominences.) Fluoroscopy can be utilized to aid in avoiding excessive or insufficient resection. Insufficient resection can lead to continued symptoms or recurrence. Excessive resection can result in subsequent growth disturbance or pathologic fracture. After completion of the desired resection—at times, this may involve multiple OCEs in the same operative field—bone wax is applied to the base. Closure is in layers after gently placing the displaced nerves and vessels back into the wound without tension. Immobilization is with splint, bivalved cast, or sling depending on the anatomic site of the surgery. Length of protection is dependent on pain and risk of pathologic fracture. Overall, more than 90% of the preoperative symptoms are resolved with OCE excision, making it a successful treatment of symptomatic OCEs with a low morbidity39,40
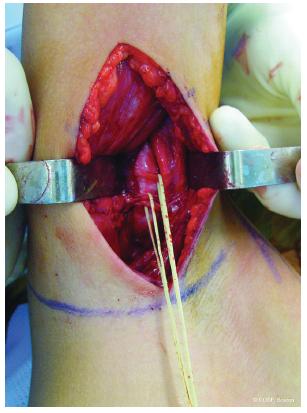
FIGURE 47-4 Intraoperative photograph of OCE of the proximal humerus with branches of the radial nerve isolated with elastic loops for protection during excision.

FIGURE 47-5 Intraoperative photograph of proximal humerus lesion in preparation for excision.
 Nail Reconstruction
Nail Reconstruction
Some patients with MHE will develop with a subungual exostosis.41,42 Once you have seen one of these, you have seen them all. The surgical focus is on the exostosis excision and restoration of a flat, aligned nail bed. Once that occurs, the nail plate will grow out with minimal to no deformity.
Removal of the nail plate is performed with a smooth, curved elevator (Freer) or small, curved snap while protecting the underlying nail bed. The thinned nail bed is carefully elevated with a small, sharp knife blade from lateral to central to expose the exostosis completely. The nail bed can be very thin over the exostosis, so very delicate elevation is required. The exostosis is removed with a rongeur to a flat base. Bone wax is placed over the open bony surface. A radiograph or fluoroscopy view is obtained to confirm complete excision. There have been instances when we thought our excision was complete only to realize it was inadequate by radiographic assessment. After complete excision, the nail bed is replaced so that it is as flat and smooth as possible. There are times when the exostosis has created a central hole in the nail bed. We do not graft those defects initially. Surprisingly, the nail plate almost always grows out with minimal to no deformity. We cauterize a hole in the center of the nail plate and replace it under the eponychium, or we use petrolatum gauze (Xeroform, Covidien, Mansfield, MA) for this purpose if the nail plate is too deformed. A protective dressing is used for 2 weeks and then serial soaks with a saline hydrogen peroxide mix and dressing changes with Xeroform; gauze and self-adherent wrap (Coban, 3M, St. Paul, MN) are used until the wound is fully healed. It takes 3 to 6 months for the final outcome of the nail plate to be determined.
 Excision of OCE and Sauve-Kapandji Procedure
Excision of OCE and Sauve-Kapandji Procedure
Wrist stabilization and forearm realignment after OCE excision can be achieved in many ways. Ulnar lengthening with a SauveKapandji procedure (fusion of the distal ulna to the radius with the creation of a more proximal ulnar pseudarthrosis to allow for pronationsupination) is one technique that has been successful in a small series of patients with moderate length follow-up.43 It is a tool worth knowing and keeping in your armamentarium.
The distal diaphyseal and metaphyseal portions of the ulna are exposed through a straight longitudinal incision with deep dissection between the extensor carpi ulnaris (ECU) and flexor carpi ulnaris (FCU). Fluoroscopy aids in identifying the physis and more proximal area of resection. In the skeletally immature patient, it is important to be more proximal than in the skeletally mature, about 2 cm proximal to the physis. Resection of the bone needs to include the periosteum, or recurrent healing of the resection will result in a single bone forearm. A 2-cm section of bone and periosteum is excised. The ulna is stretched out to neutral variance by metaphyseal measurement.23 The ulna is fused to the radius through a bone block to maintain the interosseous space and correct alignment of the radius and ulna that will allow for full forearm rotation without impingement. K-wire or cannulated screw fixation is used. Two wires or screws are necessary for rotational control. In the skeletally mature, this operation is performed just proximal to the distal radioulnar joint (DRUJ) with compressive screw fixation. At this level, bone graft is rarely needed because bone-on-bone compression can be achieved without distorting the alignment of the radius to the ulna.
This procedure can be performed in conjunction with OCE(s) excision and radial osteotomy or temporary growth arrest as appropriate. Long-arm cast immobilization is utilized until healing is sufficient enough to change to a short-arm cast without worry of rotatory stress negatively affecting healing or fixation. Smooth wires are removed in the office, or screws are left in place with full healing. Rehabilitation is important to restore full forearm rotation. Radiographs through the first year are important to be certain the ulnar pseudarthrosis stays open and there is no impingement of ulna on radius with rotation movements.
 Radial Osteotomy
Radial Osteotomy
There are patients with MHE/OCE who are referred near skeletal maturity with a chief complaint of increased ulnar deviation deformity of their wrist. Radiographs reveal ulnar shortening and increased radial articular inclination, as expected. However, their distal radius and ulna will not accommodate each other for a stable, reduced DRUJ if the ulna is lengthened. A radial closing wedge osteotomy will improve their aesthetics and wrist motion without the complexity of an ulnar lengthening, DRUJ reconstruction, or Sauve-Kapandji procedure (Figure 47-6).
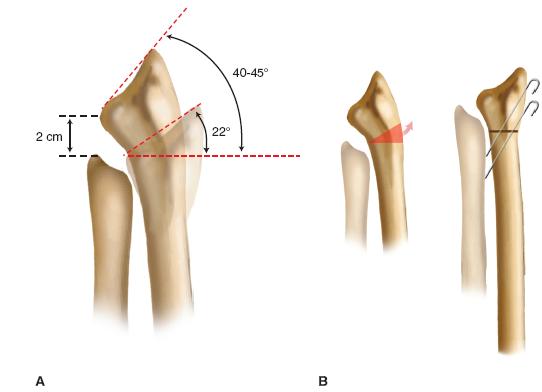
FIGURE 47-6 A: Illustration of a preoperative radiograph of adolescent patient with increased radial inclination and foreshortened ulna. B: Radial closing wedge osteotomy to level the radial articular surface and rebalance the forearm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


