AAPD policies and guidelines: http://www.aapd.org/policies/. Accessed December 26, 2013.
American Academy of Pediatric Dentistry (AAPD): Policy on the dental home. Pediatr Dent 2013;35 (Reference Manual):24–25.
Perinatal Factors & Oral Health
The perinatal period offers a unique opportunity for oral health counseling from various healthcare providers aimed at women’s self-care as well as future child care. Mothers may be unaware of the consequences of their own poor oral health or that of their children. Cariogenic bacteria can be transmitted vertically from mother to child by licking a pacifier or sharing eating utensils or horizontally between siblings of similar age, from the father, and from children in day care centers. Colonization of the infant with mutans streptococci (MS) is more likely when maternal salivary MS levels are high. The mother’s oral hygiene, snacking habits, and socioeconomic status all have an influence on the infant’s colonization with MS. Anticipatory guidance and dental treatment of the expectant mother can significantly reduce the child’s risk of acquiring MS. Prenatal dental counseling should include education on the importance of regular dental visits and the role of fluoride in maternal and childhood oral health, counseling on appropriate maternal diet, and advice on reduction of MS colonization. Maternal MS levels and the risk of transmission to infants can be reduced by twice-daily rinsing with chlorhexidine digluconate 0.12% for 2 weeks followed by chewing 100% xylitol gum for 5 minutes 3–5 times/d (total dose of xylitol 6–10 g/d) for several weeks.
Delayed dental development is characteristic of preterm infants and is also seen in infants with global developmental delay. Postnatal environmental tobacco smoke exposure increases susceptibility to childhood caries, an association that is independent of age, family income, geographic region, and frequency of dental visits. It is important to advise expectant mothers about this risk. The risk of oral anomalies is higher in preterm and low-birth-weight infants than in full-term infants. These anomalies may include a narrow palate caused by traumatic laryngoscopy or prolonged endotracheal intubation, hypoplasia of the enamel of primary dentition, and crown dilaceration (an angulation, or a sharp bend or curve, in the root or crown of a formed tooth) of the permanent maxillary incisors. The role of palatal protection plates to prevent palatal “grooving” is not clear.
AAPD: Guideline on perinatal oral health care. Pediatr Dent 2013;35 (Reference Manual):131–136.
Infant Oral Health Care
Infant oral health care is the foundation on which preventive dental care is built. Ideally, this begins before caries develops so preventive measures can be implemented. The primary goals for an infant oral health program are: (1) to establish with parents the goals of oral health; (2) to inform parents of their role in reaching these goals; (3) to motivate parents to learn and practice good preventive dental care; and (4) to initiate a long-term dental care relationship with parents. These goals can be achieved through oral examination of the child, risk assessment for oral disease, anticipatory parental guidance, and regular dental health supervision. This approach advances dental care beyond tooth monitoring toward true health promotion. Because pediatricians encounter new mothers and infants earlier than dentists, it is essential that they be aware of the infectious pathophysiology and risk factors for early childhood caries (ECC).
Pediatricians should incorporate oral health into anticipatory guidance by providing information on oral health in their offices and by referring children with special healthcare needs to a pediatric dentist as early as 6 months of age. Referral of healthy infants to establish a dental home should occur no later than 6 months after the first tooth erupts or 12 months of age (whichever comes first).
AAPD: Guideline on infant oral health care. Pediatr Dent 2013;35 (Reference Manual):131–141.
Caries-Risk Assessment
Caries-risk assessment estimates the likelihood of developing carious lesions based on biological and protective factors as well as clinical findings. By 6 months of age, every child should have a caries-risk assessment performed by a pediatric healthcare provider. The Caries Risk Assessment Form (Table 17–1) details risk indicators for the age group 0–3 years old that directly or indirectly influence development of dental caries. Caries management by risk assessment (CAMBRA) is another protocol for a comprehensive evaluation of the child and his/her family and integrates the many factors that contribute to the development of ECC into a practical and individualized strategy for caries control. Although the best predictor of future caries is the incidence of previous caries, this finding is not a practical preventative tool. Additional risk factors include the level of parental education and age of colonization with MS and lactobacilli. The earlier the colonization occurs, the greater the risk of severe decay.
Table 17–1. Caries-risk assessment for 0–3-year-olds.
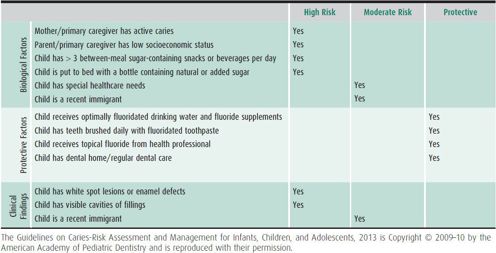
The ultimate purpose of this assessment is to develop a caries management protocol. Based on a child’s risk category and extent of parental engagement, interventions include diagnostics (regular recalls and determination of MS levels in saliva), optimization of the protective factors listed above, dietary counseling, and restorative measures as needed.
AAPD: Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent 2013;35 (Reference Manual):123–130.
Ramos-Gomez FJ et al: Caries risk assessment appropriate for the age 1 visit (infants and toddlers). J Calif Dent Assoc 2007 Oct; 35:687–702 [PMID: 18044377].
DENTAL CARIES
Dental caries is the most common chronic disease of childhood and the most prevalent unmet health need of US children. Dental caries is largely a disease of poverty. Children and adolescents in low-income families account for 80% of patients with tooth decay.
 Pathogenesis
Pathogenesis
Development of caries requires the interaction of four factors: (1) a host (tooth in the oral environment); (2) a suitable dietary substrate (fermentable carbohydrates); (3) cariogenic microorganisms that adhere to the tooth; and (4) time, measured as the frequency of exposure to fermentable carbohydrates and the duration of acid exposure. The main organisms implicated in the initiation of caries are Streptococcus mutans (MS) and Streptococcus sobrinus. Lactobacillus acidophilus and Lactobacillus casei are linked to the progression of caries. MS organisms are most commonly passed vertically from mother to child. A “window of infectivity” between ages 19 and 33 months has been described, but colonization can occur as early as 3 months of age. Earlier colonization increases the risk of caries. Dental plaque is an adherent biofilm on the tooth surface that harbors acidogenic bacteria in close proximity to the enamel. As bacteria metabolize sucrose, they produce lactic acid that solubilizes calcium phosphate in tooth enamel and dentin. Demineralization of the dental enamel occurs below pH 5.5 and is the first step in cariogenesis. The flow rate of saliva and its buffering capacity are important modifiers of demineralization. Demineralization of enamel and dentin can be halted or even reversed by redeposition of calcium, phosphate, and fluoride from saliva. If not halted, the carious process penetrates the enamel, advancing through the dentin toward the pulp of the tooth. In response, blood vessels in the pulp dilate and inflammatory cells begin to infiltrate (pulpitis). If the carious lesion is untreated, pulp exposure will occur, triggering invasion of more inflammatory cells and the eventual formation of a small pulp abscess. If this abscess can drain into the oral cavity, the apical tooth tissue may remain vital. However, if the radical pulp becomes necrotic, a periapical abscess develops (Figure 17–1). Although this process may be asymptomatic, it usually causes severe pain, fever, and swelling.

 Figure 17–1. Tooth anatomy and progression of caries.
Figure 17–1. Tooth anatomy and progression of caries.
 Clinical Findings & Treatment
Clinical Findings & Treatment
The diagnosis of caries is usually made by visual and tactile oral examination. Radiographs are used to visualize caries on the surfaces between teeth. The initial defect observed on enamel beneath the dental plaque is the so-called “white-spot lesion,” a white, chalky, decalcified area along the gingival margin or on approximated tooth surfaces. Frank carious lesions are light- to dark-brown spots or cavities of varying size on the tooth. A light shade of brown indicates more rampant decay. Arrested caries are almost black in color. In the early stages of decay, the tooth may be sensitive to temperature changes or sweets. Removing the carious tooth structure and filling the early defect with a restorative material can repair the tooth. As decay progresses deeper into the pulp, inflammation and pain increase. Eventually, the entire pulp becomes necrotic, and a choice must be made between root canal therapy (pulpectomy) or removal of the tooth. In the presence of cellulitis or facial space abscess, extraction and antibiotic therapy are the treatments of choice.
Cavitation is the late phase of disease. Filling cavities does not address the underlying pathologic process responsible for tooth decay. Unlike other infections, dental caries cannot be treated by a course of antibiotics. However, a daily dose of chlorhexidine gluconate rinse 0.12% for 2 weeks can significantly reduce the number of cariogenic bacteria in the mouth and delay recolonization for 3–6 weeks. Such treatment is recommended at 3-month intervals for patients with high levels of bacteria. Improvement in risk of dental caries can only be achieved by a sustained reduction in the number of cariogenic oral bacteria and by the creation of a favorable oral environment. Additionally, all active cavities must be restored to eliminate sources of reinfection. A patient and his/her family must be encouraged to change diet and habits of oral hygiene in an effort to prevent further infection. Motivational interviewing has been shown to be more successful in setting these self-management goals than simple or stern recommendations. Regular dental visits, the periodicity of which should be determined by the risk level for developing carious lesions, must be maintained to monitor and reinforce these goals. The concept of prevention through timely and regular parent education, early diagnosis, and prompt intervention offers greater efficiency, better health outcomes, and lower costs than repeated restoration of diseased teeth.
 Caries Prevention
Caries Prevention
Prevention of dental caries necessitates restoring the delicate balance between pathologic and protective factors. Pathologic factors include cariogenic bacteria and fermentable carbohydrates. Protective factors include salivary flow, and fluoride in food, beverages, drinking water, and oral care products. Saliva provides calcium, phosphate, proteins, antibacterial substances, and buffers to neutralize acid produced by bacteria in plaque.
A. Changes in Lifestyle
Oral hygiene practices should start soon after birth. The infant’s gums should be cleaned daily using a moist, soft cloth. Once the teeth erupt, oral hygiene must be practiced in earnest, particularly in children assessed as high risk. A small amount of fluoridated toothpaste (“smear layer”) should be used on a small, soft toothbrush designed for infants. Because of a lack of manual dexterity in children younger than 8 years of age, parents need to brush for them twice daily and assist with flossing. Another important parental task is reducing the amount of substrate available to the bacteria by limiting the consumption of sugar-containing infant formulas, beverages, and snacks. Each such exposure produces an acidic oral environment for up to 30 minutes. The primary care physician and his/her team play an invaluable role in disseminating this information during early well-baby visits.
B. Fluorides
Fluorides are safe and effective in caries prevention through three topical mechanisms of action: inhibition of bacterial metabolism by interfering with enzyme activity; inhibition of demineralization; and enhancing remineralization. Fluoride can be applied professionally or by the patient under parental supervision. Although more than half the US population has access to fluoridated community water, an increasing number of families consume processed water with unknown fluoride content. Fluorides affect the dentin and enamel of both erupted and unerupted teeth. Systemic effects are achieved by oral ingestion from sources such as fluoridated drinking water or fluoride supplements. Fluoridated toothpaste and mouth rinses deliver topical benefits. Table 17–2 shows the current ADA recommendations for dietary fluoride supplementation for children at high caries risk. They should be taken daily to maximize the caries risk prevention benefit. For children at low caries risk, dietary fluoride supplements are not recommended. The child’s true exposure to fluoride must be evaluated before supplements are prescribed to avoid the mottled enamel (dental fluorosis) produced by excessive fluoride. Because children younger than 6 years of age cannot expectorate reliably, parents must monitor the use of fluoridated toothpaste, ensuring that only a “pea-sized” amount of the product is used at each brushing. Several factors are associated with a high risk for caries—orthodontic appliances, decreased salivary function, gastroesophageal reflux disease, cariogenic diet, physical inability to properly clean the teeth, mother or siblings with caries, personal history of caries. Children with these risk factors should be considered for additional topical fluoride therapy to supplement oral hygiene measures.
Table 17–2. Dietary fluoride supplementation schedule for children at high caries risk.
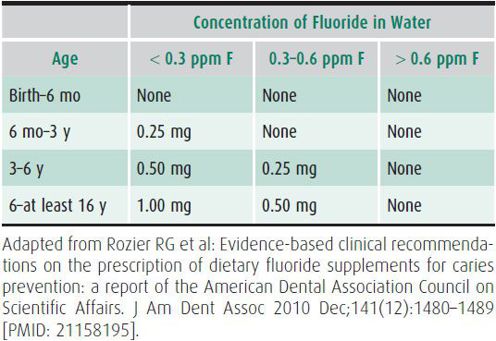
Infants who consume concentrate infant formulas as the main source of nutrition may incur an increased risk for enamel fluorosis in the permanent dentition if those formulas are reconstituted with optimally fluoridated drinking water. It is important that practitioners evaluate all sources of fluoride intake when advising parents about the use of fluoridated toothpastes or prescribing fluoride supplements.
Berg J et al: Evidence-based clinical recommendations regarding fluoride intake from reconstituted infant formula and enamel fluorosis: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2011 Jan;142(1):79–87 [PMID: 21243832].
C. Other Adjunctive Measures
Consumption of beverages sweetened with artificial sweeteners instead of sugar can help reduce the intake of fermentable carbohydrates. While chewing gum helps to clean food debris from teeth and increases salivary flow, these beneficial effects are lost when sugar-containing gum is used. The AAP considers chewing gum a choking risk in smaller children. A significant reduction of salivary MS by the polyol sweetener xylitol has been described, but a dose of at least 5–10 g/d for adults and 5–7.5 g/d for toddlers aged 6–36 months with exposure times lasting several minutes three times daily are required to produce this effect. Topical application of 8 g/d xylitol syrup in 9–15-month-old children twice per day for 12 months during primary tooth eruption could prevent up to 70% of dental caries. However, unclear labeling of the ingredients in xylitol-containing products makes the exact determination of the dose difficult and the high cost of foods containing xylitol limits its widespread use.
AAPD: Policy on the use of Xylitol in caries prevention. Pediatr Dent 2013;35 (Reference Manual):45–47.
Featherstone JD: The science and practice of caries prevention. J Am Dent Assoc 2000 Jul;131(7):887–899 [PMID: 10916327].
Early Childhood Caries
Formerly termed “baby bottle tooth decay” or “nursing bottle caries,” early childhood caries (ECC) is a particularly virulent and rapidly progressive form of caries that begins on the smooth surfaces of the teeth soon after eruption. Lack of adequate preventive care as well as poor feeding habits, such as the frequent consumption of liquids containing fermentable carbohydrates from a nursing bottle, frequent sipping from a no-spill sippy cup, taking a bottle to bed, and breast-feeding in combination with other carbohydrates, place children at high risk for ECC. It is uncertain whether ad libitum breast-feeding increases the risk for developing caries. ECC typically involves the maxillary incisors but any other teeth may be affected.
ECC is defined as one or more decayed (d), missing (m), or filled (f) tooth surfaces (s) in any primary tooth in a child younger than 71 months of age. Any sign of smooth-surface caries in a child younger than 3 years is termed severe ECC (S-ECC). From 3 to 5 years, one or more decayed, missing, or filled smooth surfaces in maxillary front teeth or a total dmfs score of 4 or higher must be present to make a diagnosis of S-ECC. By age 5 years, a dmfs score of 6 or higher must be present to constitute S-ECC. Children with S-ECC are at higher risk for new carious lesions, more frequent hospitalizations, and emergency department visits. They are absent more often from school, may have below-normal height and weight gain, and have a diminished oral health-related quality of life. Although S-ECC can affect all children, it is 32 times more likely in children who consume sugary foods and whose mothers are of low socioeconomic status and education level.
Parents should be counseled to eliminate saliva-sharing activities and not to put infants to sleep with a bottle containing fermentable carbohydrates. After eruption of the first tooth, ad libitum breast-feeding should be discontinued and regular oral hygiene measures such as twice-daily use of fluoridated toothpaste, both in optimally fluoridated and fluoride-deficient communities, should be implemented. Infants should be weaned from the bottle at about 1 year of age and encouraged to drink from a uncovered cup mainly as part of a snack or meal. Frequent consumption of cariogenic liquids from a bottle or no-spill training cup should be avoided. The AAP recommends limiting juice to 4–6 oz/day for children 1–6 years of age.
Preventive strategies focused on the pregnant woman should start in the prenatal and perinatal periods. Maternal malnutrition during the third trimester, low birth weight, and systemic illness in the neonatal period can lead to tooth hypoplasia, which makes teeth more susceptible to caries. Later, motivational interviewing may help parents to reduce deleterious feeding habits and to adopt lifestyle changes within their family that address the multifactorial etiologies of early childhood caries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


