Tumors of odontogenic epithelium
Ameloblastoma
Squamous odontogenic tumor
Adenomatoid odontogenic tumor
Keratocyst odontogenic tumor
Calcifying epithelial odontogenic tumor (Pindborg)
Clear cell odontogenic carcinoma
Intraosseous odontogenic carcinoma
Tumors of odontogenic mesenchyme
Odontogenic myxoma
Cementoblastoma
Odontogenic fibroma
Mixed odontogenic tumors
Ameloblastic fibroma
Ameloblastic fibro-odontoma/fibrodentinoma
Odontoma
Tumors of Odontogenic Epithelium
Ameloblastoma
Introduction
Ameloblastoma is a tumor of odontogenic epithelial origin [1]. It is the second most common odontogenic tumor after the odontoma . There are three major types, solid or multicystic (86 % of all cases), unicystic (13 % of all cases), and peripheral (1 % of all cases), that have different treatments and prognosis [2].
Biology and Epidemiology
Ameloblastoma arises from the rests of dental lamina. It is a benign tumor that is slow-growing but can be locally invasive.
Unicystic type: most often seen in young patients, with 50 % diagnosed during the second decade of life. The mean age at presentation is 23 years [2] and there is no sex predilection. There are three histopathologic variants of the unicystic ameloblastoma (intraluminal, luminal, and mural) that have different treatments and prognosis [3]. The mural variant appears to be more aggressive than the intraluminal or luminal variants because of its presence outside the cyst wall and closer to the surrounding bone.
Solid or multicystic type: occurs in patients over a wide age range. Though it is prevalent mainly during the third to seventh decades of life, it can be seen in the second decade. It is rare in children [2]. There is no sex predilection. It is benign but locally aggressive.
Peripheral ameloblastomas: usually seen in middle age persons with average age of 52 years [2].
There is an increase in frequency of ameloblastoma in children of African descent. Tumors in these children have a different site of predilection, being more common in the mandibular symphysis region. The morphologic type closely resembles the adult type and not the unicystic pattern [4]. It is not known whether there is a true racial difference, and the tumor incidence is not known.
Ameloblastoma can exhibit malignant behavior with development of metastases and is therefore called metastasizing or malignant ameloblastoma. It occurs in less than 1 % of all ameloblastomas [2].
Presentation
It can occur in either of the jaws, with asymptomatic swelling and/or expansion. Pain and paresthesia are uncommon.
Unicystic ameloblastomas: most are associated with an impacted tooth and the mandibular third molar is the most common site.
Solid and multicystic types: occur mostly in the mandible, usually in the posterior region [5].
Differential Diagnosis
A variety of odontogenic and nonodontogenic lesions may have similar clinical and radiographic presentations.
Dentigerous cyst
Keratocystic odontogenic tumor
Ameloblastoma
Odontogenic myxoma
Giant cell lesion
Lymphoma
Langerhans cell histiocytosis
Diagnosis and Evaluation
Physical Examination
Buccal and/or lingual cortical expansion is common
Usually nontender
Can cause root resorption and/or displacement
Unicystic ameloblastoma: commonly associated with an unerupted mandibular third molar tooth
Imaging Evaluation
Panoramic radiograph:
Unicystic ameloblastoma: well circumscribed radiolucency, usually surrounding an unerupted mandibular third molar, often mimicking a dentigerous cyst (Figs. 33.1 and 33.2) [3].

Fig. 33.1
Panoramic radiograph demontrates large, unilocular, radiolucent lesion in the left mandible associated with the crown of the impacted second mandibular molar, which is inferiorly displaced. The lesion extends from the first molar to mid ramus, with displacement of the third molar bud
Multicystic ameloblastoma: multilocular radiolucent lesion, often described as “soap bubble” or “honeycombed.” The radiolucent areas often have irregularly scalloped margins.
Solid variant: unilocular radiolucent lesion is not typically associated with the crown of a tooth.
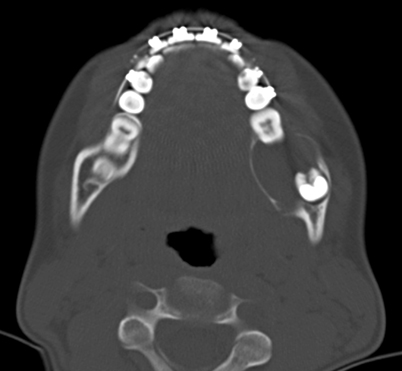
Fig. 33.2
Axial computed tomography (CT) scan demontrating unilocular lesion, with buccal and lingual cortical thinning and expansion, but no evidence of cortical perforation or soft tissue involvement
Pathology
Three histologic variants of unicystic ameloblastoma are described in the literature (Figs. 33.3, 33.4a, b) [2, 3]. In the luminal unicystic ameloblastoma, the tumor is confined to the luminal surface of the cyst while the intraluminal unicystic ameloblastoma has tumor nodules that project from the cystic lining into the lumen of the cyst. In the mural unicystic ameloblastoma, the fibrous wall of the cyst is infiltrated with tumor nodules. The solid and multicystic variants also have several microscopic subsets. The follicular and plexiform patterns are the most common. Less common patterns include granular cell, desmoplastic, acanthomatous, and basal cell types. The follicular pattern shows islands of odontogenic epithelium within a fibrous stroma. The basal cells of these islands are tall, columnar, and hyperchromatic. The nuclei are displaced away from the basement membrane (reverse polarity). Mitotic activity is rare in all variants of ameloblastomas .
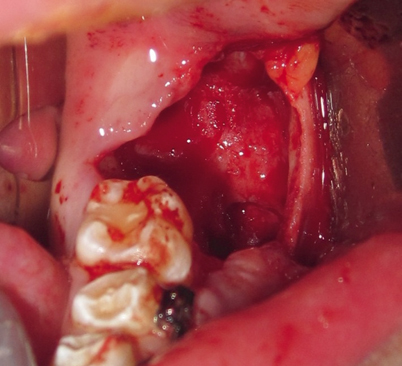
Fig. 33.3
Intraoperative photograph of the defect after enucleation and extraction of second and third molars
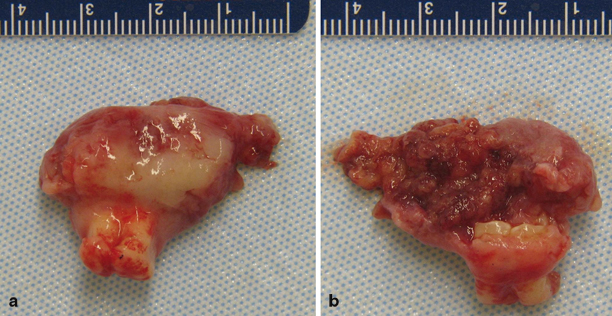
Fig. 33.4
Gross specimen of the outer surface of cyst (a); roots of second molar can be seen. The inside of the cyst is filled with projections (b)
Treatment and Prognosis
Luminal and intraluminal variants of unicystic ameloblastoma: enucleation and currettage with close follow-up [3, 6]. There is a less than 25 % recurrence after enucleation and curettage [7]. Intraoperatively, frozen section should be obtained to properly subclassify the variant of unicystic ameloblastoma [3]. If there is evidence of extension into the fibrous capsule, the tumor becomes the mural variant and, then, a marginal resection with 1 cm margins should be performed.
Solid and multicystic types: resection with 1–1.5 cm bony margins and one uninvolved anatomic barrier margin [8]. Enucleation and curettage is inadequate treatment for these types with a 50–60 % recurrence rate [9] but only a 2–4.5 % recurrence after wide resection [8, 9].
It must be followed for at least 10 years because recurrence can occur late [10].
Squamous Odontogenic Tumor
Introduction
Biology and Epidemiology
It arises from the neoplastic transformation of the rests of dental lamina or the epithelial rests of Malassez [11, 12].
Presentation
Differential Diagnosis
Dentigerous cyst
Radicular cyst
Ameloblastoma
Squamous cell carcinoma
Diagnosis and Evaluation
Physical Examination
Imaging Evaluation
Panoramic radiograph: the findings are variable and not diagnostic (Fig. 33.6). It can range from small to large in size and is irregularly shaped or has semicircular radiolucencies with smooth sclerotic borders. They are seen within the alveolar bone along the lateral surfaces of tooth roots [14].
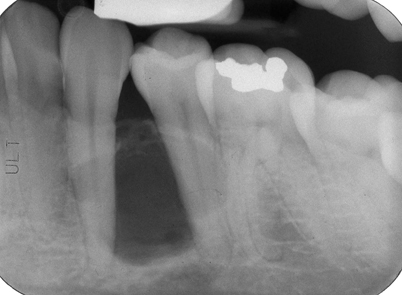
Fig. 33.6
Periapical dental radiograph demonstrates irregularly shaped, well-demarcated, radiolucent lesion in the alveolar bone between roots of adjacent teeth
Pathology
These tumors are composed of numerous islands of well-differentiated squamous epithelium with focal areas of keratinization, calcification, and cystic degeneration scattered in mature fibrous connective tissue stroma [15]. It is similar to squamous metaplasia described in ameloblastomas, but it differs by the lack of peripheral columnar cells with palisading nuclei. No polarization of nuclei is seen in this lesion and the cells lack atypical mitosis which could differentiate it from a well-differentiated squamous cell carcinoma.
Outcome
Recurrences are rare and are likely due to incomplete removal. Further excision is usually curative. Twenty percent of patients can have new lesions at different locations [15].
Adenomatoid Odontogenic Tumor
Introduction
Adenomatoid odontogenic tumor (AOT) is a benign hamartoma which was initially considered a variant of ameloblastoma [2, 16, 17]. However, its clinical features and biologic behavior are significantly different. The terminology, AOT, was introduced by Philipsen and Birn [16] and classified by the WHO in 1971 [16, 17].
Biology and Epidemiology
AOT is a benign neoplasm and comprises only 3–7 % of all odontogenic tumors [2, 17]. The lesion arises from the remnants of dental lamina.
Three variants: follicular, extrafollicular, and peripheral [16, 17]. The follicular type is the predominant form (75 %) with a central intraosseous lesion associated with an impacted tooth [2, 13, 16–18]. The extrafolicular type is also an intraosseous lesion, but is not associated with teeth. The peripheral type is very rare and is extraosseous.
It affects young patients and is usually diagnosed in the second decade of life.
It has a female predilection, with a 2:1 ratio.
Presentation
Differential Diagnosis
Keratocystic odontogenic tumor
Ameloblastoma
Dentigerous cyst
Calcifying odontogenic cyst
Calcifying epithelial odontogenic tumor
Diagnosis and Evaluation
Physical Examination
Size: usually less than 3 cm in diameter.
Larger lesions can cause a tender bony expansion [2].
Imaging Evaluation
Panoramic radiograph: appears as a well circumscribed, pear-shaped radiolucency. Seventy-five percent of the cases are associated with an unerupted tooth. Unlike dentigerous cysts that attach to the cementoenamel junction of an impacted tooth, the attachment of AOT to the impacted tooth occurs more apically onto the root surface [2, 13]. There may also be fine calcifications found within the radiolucent lesion.
Pathology
They have a thick capsule with nodules and whorls of epithelium that may form rosette-like structures around a central space. There may also be small foci of calcification. The tubular or duct-like structures with a central space surrounded by a layer of columnar or cuboidal epithelial cells are the characteristic features [2, 13].
Treatment
Treatment is enucleation, making sure the capsule is intact upon removal.
Recurrence is rare.
Because there is no documentation of aggressive behavior, it is important to distinguish AOT from ameloblastoma to avoid a more aggressive operation.
Keratocystic Odontogenic Tumor
Introduction
Keratocystic odontogenic tumor (KCOT) is a benign intraossesous cystic tumor of odontogenic origin which can be locally destructive and has a high recurrence rate. This lesion had previously been called odontogenic keratocyst but it was renamed by the WHO in 2005 because the current name better reflects its behavior as a neoplasm [1, 19].
Biology and Epidemiology
KCOT arises from the cell rests of the dental lamina [20]. Recent studies have also demonstrated that the PTCH gene plays a role in sporadic KCOT.
Found in people over a wide age range, from the first to the ninth decades, with a peak in frequency in the second and third decades [21].
Slight male predilection.
If multiple KCOTs are present, the patient should be evaluated for other findings that make up the nevoid basal cell carcinoma (Gorlin) syndrome.
Presentation
Small KCOTs are asymptomatic and incidentally discovered during routine radiographic examinations. Larger KCOTs may cause swelling, pain, or become secondarily infected.
Differential Diagnosis
Dentigerous cyst
Ameloblastoma
Ameloblastic fibroma
Langerhans cell histiocytosis
Giant cell tumor
Aneurysmal bone cyst
Diagnosis and Evaluation
Physical Examination
Majority of the lesions occur in the posterior mandible in the third molar region [21].
Teeth may be displaced but root resorption is rare.
Bony expansion and fluctuance, if present, is resorption or perforation of the cortex.
Imaging Evaluation
Panoramic radiograph: well-defined radiolucency with smooth, well-corticated margins (Figs. 33.7 and (33.8). Twenty-five to forty percent of cases are associated with an unerupted tooth [2]. It may displace the inferior alveolar nerve inferiorly.
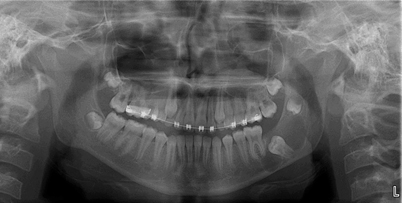
Fig. 33.7
Panoramic radiograph showing large left mandibular body and ramus radiolucent lesion associated with unerupted second molar and superiorly displaced third molar

Fig. 33.8
Axial computed tomography (CT) scan of left mandible showing radiolucent lesion with intact cortex and minor buccal and lingual cortical expansion
Pathology
On gross examination, the cystic lumen may contain cheesy material or clear liquid. The lining is thin and fragile. Microscopically, the epithelial lining is composed of uniform layer of stratified squamous epithelium, 5–8 cell layers thick, without rete ridges. The luminal surface shows parakeratinized epithelium. There is a well-defined, palisaded basal layer of columnar or cuboidal cells [21].
Treatment
Treatment of KCOT remains controversial, with recommendations including marsupialization, decompression, enucleation with or without curettage, peripheral ostectomy and/or cryotherapy, and resection.
No consensus as to which is the most appropriate treatment. Although resection offers the highest cure rate and reduces recurrences, it is associated with the greatest morbidity. Enucleation with or without curettage, peripheral ostectomy, or cryotherapy preserves the jaw structure but has a higher recurrence rate.
Outcome
The high recurrence rate for KCOT may result from incomplete removal or residual epithelial islands (daughter cysts).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



