KEY POINTS
• Since its introduction into clinical obstetrics, obstetric ultrasound imaging (OUI) has become an essential component of prenatal care.
• OUI requires careful documentation of findings, particularly in regard to confirmation of dates and fetal anatomy.
• While OUI has assumed important social significance to mothers and their families, it is important patients understand that it is a medical examination with certain limitations.
BACKGROUND
Applications
• Biometry
• Biometry is direct ultrasonic measurements of the fetus.
• Biometric information is used to estimate gestational age and fetal weight.
• When combined with appropriate clinical information, biometry is used to document normal or altered growth patterns of the fetus and fetal organ systems.
• Structural assessment
• High-resolution ultrasound images can detect
 Structural abnormalities of the fetal gastrointestinal, skeletal, genitourinary, cardiac, and central nervous systems
Structural abnormalities of the fetal gastrointestinal, skeletal, genitourinary, cardiac, and central nervous systems
 Multiple gestations
Multiple gestations
 Placental abnormalities
Placental abnormalities
• Assessment of fetal well-being
• Real-time ultrasound is used to obtain biophysical profiles (BPPs), amniotic fluid volume assessments, and Doppler studies of the fetal vasculature in the antepartum period.
• These tests provide information on the well-being of the fetus and have helped reduce perinatal mortality.
• Screening for chromosomal abnormalities
• Ultrasound can be used in the first and second trimester to screen for chromosomal abnormalities, such as Down syndrome.
 A first-trimester screen involves measuring fetal nuchal translucency between 10 and 14 weeks’ gestation.
A first-trimester screen involves measuring fetal nuchal translucency between 10 and 14 weeks’ gestation.
 A second-trimester screening involves multiple serum analyte and ultrasound markers that correlate with chromosomal abnormalities.
A second-trimester screening involves multiple serum analyte and ultrasound markers that correlate with chromosomal abnormalities.
• Guidance for invasive procedures
• Real-time ultrasonography is used to guide needle placement during invasive procedures such as amniocentesis, chorionic villus sampling (CVS), and cordocentesis.
• Early pregnancy assessment
• Ultrasonography is useful for evaluating early pregnancy issues, such as
 Verifying the presence (or absence) of a viable intrauterine gestation when bleeding occurs
Verifying the presence (or absence) of a viable intrauterine gestation when bleeding occurs
 Excluding ectopic pregnancy when pain is present
Excluding ectopic pregnancy when pain is present
 Assigning accurate dates
Assigning accurate dates
EVALUATION
General Principles
• Safety concerns.
• As a general principle, obstetrical ultrasound studies should be performed only for specific clinical indications.
• Ultrasound imaging uses focused, high-frequency sound waves to generate images.
• Ultrasound waves transmit energy and can theoretically cause damage to the fetus through the mechanisms of heat and cavitation (the production and collapse of bubbles).
• At much higher intensities than are in current clinical use, ultrasound waves have been shown to disrupt biologic systems.
• The relative susceptibility of a given organ system to ultrasound damage is related to the intensity and duration of ultrasound exposure, its distance from the sound source, and the thermal dissipation characteristics of the organ system (related to blood flow through the organ).
• In a review of the safety of ultrasonography in obstetrics, the U.S. Food and Drug Administration (FDA) stated that, although no definite effects could as yet be documented for current exposure levels, the possibility of long-term side effects could not be excluded. Further, the report warned that such effects might be subtle in nature and not easily detected.
• A long-term follow-up study (8 to 9 years) of children exposed to routine ultrasonography in utero showed that the risk of having poor skills in reading and writing was no greater for children whose mothers had routine ultrasonography than for those whose mothers had not had the procedure (1).
Principles of Ultrasound Image Generation
• Ultrasound images are generated by coordinating a transducer, which is a combined sound generator and receiver, with an electronic processor.
• Timed high-frequency pulses of sound (usually in the range 2 to 8 MHz) are sent out and then reflected back to the transducer by objects in the field.
• The time delay between signal generation and return is calculated by the electronic processor, and because the average speed of sound waves in human tissues is known (1540 m per second), this delay in signal return can be displayed as depth.
• By simultaneously obtaining images from adjacent points, the electronic processor can assemble a real-time cross-sectional image of structures within the sound field. This image can be oriented in a linear, curvilinear, or radial manner, depending on the shape of the transducer apparatus.
• Transabdominal and transvaginal transducers rely on the same technology and are commonly used in obstetric and gynecologic ultrasound:
• Imaging energy frequencies
 Multiple-energy frequencies are available; however, the range that is used for obstetrical imaging is typically between 2 and 9 MHz.
Multiple-energy frequencies are available; however, the range that is used for obstetrical imaging is typically between 2 and 9 MHz.
 The exact frequency used for imaging depends on the clinical setting and variables such as tissue density and required depth of penetration. Although fixed frequency transducers can be used, the transducers that are currently in use are variable over a preset energy range with continuous adjustment provided by the electronic processor. Typical energy ranges are
The exact frequency used for imaging depends on the clinical setting and variables such as tissue density and required depth of penetration. Although fixed frequency transducers can be used, the transducers that are currently in use are variable over a preset energy range with continuous adjustment provided by the electronic processor. Typical energy ranges are
– Abdominal curvilinear probe: 2 to 7 MHz
– Vaginal probe: 5 to 9 MHz
– 3D/4D probe: 4 to 8 MHz
 Generally, 5 or 6 MHz provides the best resolution. However, these high-frequency sound waves are easily attenuated by bodily tissues and do not adequately image fetuses more than 6 to 8 cm from the transducer. When this is a problem, lower frequencies of 3 to 4 MHz are used.
Generally, 5 or 6 MHz provides the best resolution. However, these high-frequency sound waves are easily attenuated by bodily tissues and do not adequately image fetuses more than 6 to 8 cm from the transducer. When this is a problem, lower frequencies of 3 to 4 MHz are used.
• Tissue interfaces
 Highly dense structures such as bones are hyperechoic, meaning they reflect a large portion of an incident sound signal, sometimes resulting in a shadowing of structures lying behind them.
Highly dense structures such as bones are hyperechoic, meaning they reflect a large portion of an incident sound signal, sometimes resulting in a shadowing of structures lying behind them.
 Fluid-filled structures are hypoechoic, meaning they generate few return images and appear empty on the display.
Fluid-filled structures are hypoechoic, meaning they generate few return images and appear empty on the display.
 Interfaces between areas of differing tissue densities (e.g., fluid–tissue, tissue–bone) are the most easily visualized.
Interfaces between areas of differing tissue densities (e.g., fluid–tissue, tissue–bone) are the most easily visualized.
 Fetal imaging is more difficult if little difference exists between the structure of interest and surrounding tissues (e.g., distinguishing fetal abdominal circumference (AC) from the uterus if oligohydramnios is present, distinguishing renal parenchyma from surrounding retroperitoneal structures if calyceal structures are not well developed).
Fetal imaging is more difficult if little difference exists between the structure of interest and surrounding tissues (e.g., distinguishing fetal abdominal circumference (AC) from the uterus if oligohydramnios is present, distinguishing renal parenchyma from surrounding retroperitoneal structures if calyceal structures are not well developed).
• Doppler ultrasound
 Ultrasound can be used to measure the direction and velocity of fluid flow by means of the Doppler principle.
Ultrasound can be used to measure the direction and velocity of fluid flow by means of the Doppler principle.
 The Doppler effect, which is a change in frequency of sound with motion, means that predictable changes in the frequency of a sound wave occur when it is reflected by moving red cells. Cells moving toward a sound wave source will reflect sound waves back at a higher frequency; cells traveling away from a source will reflect sound at a diminished frequency. Furthermore, blood cells moving with a higher velocity reflect sound waves back at a higher frequency than cells moving with a slower velocity. By comparing initial and returning sound frequencies, a Doppler shift is calculated. This information can then be combined (“duplexed”) with simultaneous standard ultrasound images to provide information regarding blood flow in a given area.
The Doppler effect, which is a change in frequency of sound with motion, means that predictable changes in the frequency of a sound wave occur when it is reflected by moving red cells. Cells moving toward a sound wave source will reflect sound waves back at a higher frequency; cells traveling away from a source will reflect sound at a diminished frequency. Furthermore, blood cells moving with a higher velocity reflect sound waves back at a higher frequency than cells moving with a slower velocity. By comparing initial and returning sound frequencies, a Doppler shift is calculated. This information can then be combined (“duplexed”) with simultaneous standard ultrasound images to provide information regarding blood flow in a given area.
 Blood flow direction.
Blood flow direction.
– In color Doppler imaging, color converters are added to assign color codes to the directions of blood flow.
– By convention, flow toward the transducer is colored red, and flow away from the transducer is colored blue. Such information is superimposed on a standard sonographic image.
– Color flow Doppler ultrasound is particularly useful for evaluating the fetal cardiovascular system and for improving the efficiency of pulsed Doppler measurements.
– Color Doppler ultrasound is pulsed energy transmission. A relatively large amount of sound energy is required to generate these images. The FDA has approved these energy levels for use in pregnancy. But pulsed Doppler ultrasound should not be used continuously in first-trimester scanning due to the total amount of energy to which the fetus could be exposed.
 Blood flow velocity.
Blood flow velocity.
– Doppler ultrasound can also be used to calculate blood flow velocity either (a) In direct terms as centimeters per second or (b) As the Pourcelot index (RI) or pulsatility index (PI), which are modified ratios of frequency shifts during systole and diastole
– These measurements have been performed for various fetal vessels, including the umbilical artery, the aorta, the carotids, the renals, the splenic, the uterine, the middle cerebral artery, and the ductus venosus in an attempt to facilitate diagnosis of fetal disease states (2).
Types of Ultrasonographic Studies
The American College of Obstetricians and Gynecologists (ACOG), in its technical bulletin on ultrasonography in pregnancy (number 101, December 2011), divided obstetric ultrasound examinations into three types in the second and third trimesters: standard, limited, and specialized. The first-trimester ultrasound is distinct and discussed separately.
• Standard examination: The standard examination is performed during the second and/ or third trimesters of pregnancy.
• It includes an evaluation of fetal presentation, amniotic fluid volume, cardiac activity, placental position, fetal biometry, fetal number, and an anatomic survey of the fetus. If technically feasible, the uterus and the adnexa should be evaluated.
• The essential elements of the standard ultrasound examination fetal anatomic survey, as defined by the ACOG, are listed in Table 31-1.
• Details of the standard examination include
 A general description of the intrauterine contents, including the number and orientation of fetuses, the placement of the placenta with relation to the uterine cavity and the cervix, and the estimation of the amniotic fluid volume (individual estimations for all fetuses in multiple gestations)
A general description of the intrauterine contents, including the number and orientation of fetuses, the placement of the placenta with relation to the uterine cavity and the cervix, and the estimation of the amniotic fluid volume (individual estimations for all fetuses in multiple gestations)
 Measurement of the following fetal features:
Measurement of the following fetal features:
– Biparietal diameter (BPD)
– Head circumference (HC)
– Abdominal circumference (AC)
– Femur length (FL)
 For all fetuses beyond 22 weeks of gestation, an estimated fetal weight (EFW) should be calculated from proved regression equations or by using suitable fetal weight nomograms. This estimated weight should then be interpreted as a percentile for gestational age (e.g., “The EFW based on a BPD-AC table was 1720 g, placing the fetus at the 25th percentile for gestational age”).
For all fetuses beyond 22 weeks of gestation, an estimated fetal weight (EFW) should be calculated from proved regression equations or by using suitable fetal weight nomograms. This estimated weight should then be interpreted as a percentile for gestational age (e.g., “The EFW based on a BPD-AC table was 1720 g, placing the fetus at the 25th percentile for gestational age”).
 A survey of the fetal anatomy (Table 31-1).
A survey of the fetal anatomy (Table 31-1).
 Comment about the fetal heart rate and rhythm.
Comment about the fetal heart rate and rhythm.
 A cursory evaluation should be carried out for other problems such as an abnormally thickened (hydropic) placenta, an overly distended fetal bladder, cystic dilation of a renal pelvis, evidence of fetal ascites or other effusions, or uterine abnormalities (such as leiomyomas); a survey of the maternal pelvic organs should also be performed.
A cursory evaluation should be carried out for other problems such as an abnormally thickened (hydropic) placenta, an overly distended fetal bladder, cystic dilation of a renal pelvis, evidence of fetal ascites or other effusions, or uterine abnormalities (such as leiomyomas); a survey of the maternal pelvic organs should also be performed.
 In multifetal gestations, the presence of a dividing membrane should always be sought (because this effectively excludes the possibility of monochorionic/monoamniotic twins). Multifetal gestations beyond 24 weeks of gestation should be evaluated for growth restriction and discordance. Discordance in twins has been defined as a difference in EFWs of more than 20% (3,4).
In multifetal gestations, the presence of a dividing membrane should always be sought (because this effectively excludes the possibility of monochorionic/monoamniotic twins). Multifetal gestations beyond 24 weeks of gestation should be evaluated for growth restriction and discordance. Discordance in twins has been defined as a difference in EFWs of more than 20% (3,4).
• Limited examination
• When a specific question requires investigation, a limited ultrasound examination may be performed.
• Limited examinations focus on a specific ultrasonic finding that is usually being surveyed serially, such as the assessment of amniotic fluid volume, confirmation of fetal viability, localization of placenta, evaluation of the cervix, and confirmation of fetal presentation.
• If a limited study is selected, a previous standard examination should have been performed and the determination made that a repeat standard examination is not warranted (3).
• Specialized examination
• A specialized examination (detailed or targeted) is a more extensive examination of the entire fetus, often with special attention on a specific fetal organ system. It may be indicated for a fetus with a suspected congenital anomaly or in pregnancies with severe growth abnormalities.
• It must be emphasized that the accuracy of ultrasonography, even in the most expert hands, does not approach 100%. Patients should be informed of this limitation.
• The specialized study is best performed under the direct supervision of an experienced sonographer as a real-time examination (3).
• Biophysical profile
• The BPP is a specialized type of ultrasound examination that was originally described by Manning and colleagues (5).
• The BPP is a scoring system that has proved to be a valuable method of fetal antepartum assessment. Its principal advantage over other methods of fetal evaluation is that it retains sensitivity (i.e., the ability to diagnose impending fetal compromise) but offers improved specificity (fewer false-positives or abnormal findings).
• There are four sonographic criteria for the BPP (fetal breathing movements, gross body–limb movements, general body tone, and amniotic fluid volume) and a fetal heart rate nonstress test (NST) component. Each is scored as either normal or abnormal. Two points are assigned for normal findings and no points if a category is judged abnormal. (Note that there are no 1-point scores.)
• These points are added to give the total score:
 8 or 10 is normal.
8 or 10 is normal.
 6 is equivocal.
6 is equivocal.
 4 or less is abnormal.
4 or less is abnormal.
 0 or 2 is ominous.
0 or 2 is ominous.
• The BPP and other similar tests are clinical applications of available technology. They must be interpreted in light of all relevant clinical data pertaining to a given patient. Caution should be used in inferring a particular prognosis from an individual test result viewed outside the clinical context.
• First-trimester examination. The first-trimester examination is performed prior to 14 weeks’ gestation.
• It may be performed transabdominally or transvaginally. A transvaginal exam should be performed if the transabdominal exam is not definitive.
• It includes an evaluation of the uterus including the cervix and adnexa, the description of the gestational sac including its location and the presence or absence of a yolk sac or embryo, measurement of the crown–rump length (CRL), and documentation of cardiac activity, fetal number, chorionicity, and amnionicity.
• If ultrasound screening for aneuploidy is desired, a nuchal translucency should be measured (3).
Table 31-1 Essential Elements of Fetal Anatomic Ultrasound Survey
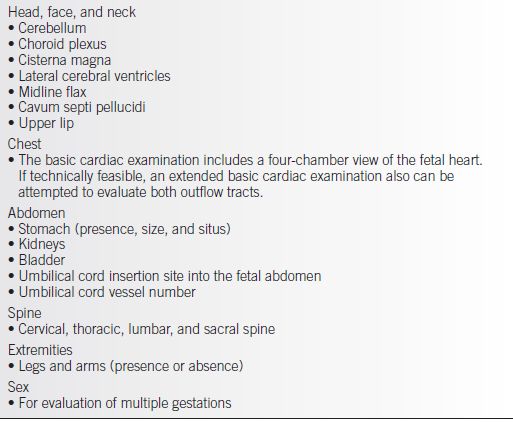
From American College of Obstetricians and Gynecologists. ACOG Tech Bull. 2009;101; and American College of Radiology. ACR practice guideline for the performance of antepartum obstetrical ultrasound. In: ACR practice guidelines and technical standards. Philadelphia: American College of Radiology, 2007:1025–1033.
Overview of Technique for Various Fetal Measurements
• Four fetal measurements are essential to every fetal ultrasound examination.
• Biparietal diameter
 The fetal BPD is measured in a plane transverse to the long axis of the head, which allows visualization of the midline falx cerebri, the cavum septum pellucidum, and the thalamus (which can be seen straddling the midline centrally) (Fig. 31-1
The fetal BPD is measured in a plane transverse to the long axis of the head, which allows visualization of the midline falx cerebri, the cavum septum pellucidum, and the thalamus (which can be seen straddling the midline centrally) (Fig. 31-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


