Chapter 18
Obstetric Management of Labor and Vaginal Delivery
Alan T.N. Tita MD, PhD, Dwight J. Rouse MD, MSPH
Chapter Outline
The Process of Labor and Delivery
Labor, which is also called parturition, is the process by which sufficiently frequent and strong uterine contractions cause thinning (i.e., effacement) and dilation of the cervix, thereby permitting passage of the fetus from the uterus through the birth canal.
Onset of Labor
Timing
Fewer than 10% of pregnancies end on the expected date of delivery (EDD), although the majority of births occur within 7 days of the EDD. In the United States, approximately 13% of births occur preterm (before 37 weeks’ gestation), and approximately 5% to 7% of pregnancies remain undelivered at 42 weeks’ gestation (14 days after the EDD, known as post-term). These rates are lower for carefully dated pregnancies.
Mechanism
The cause of the onset of labor in women—either term or preterm—remains unknown. In other mammalian species, a decrease in serum progesterone concentration in association with an increase in estrogen concentration is followed by increases in prostaglandin production, oxytocin receptors, and myometrial gap junction formation. In sheep, the fetus apparently triggers parturition through a surge in fetal cortisol production. In women, progesterone concentrations do not decline before the onset of labor and no surge in fetal cortisol secretion occurs. The laboring human uterus does manifest increases in prostaglandin production, oxytocin receptors, and myometrial gap junction formation.1,2 As more is learned, perhaps a unifying concept of the onset of mammalian labor will emerge. Preterm and post-term deliveries both constitute important obstetric problems; and when more is understood about the mechanism of the onset of labor, new approaches to preventing the preterm and post-term onset of parturition may evolve.
Stages of Labor
By convention, labor is divided into three stages. The first stage begins with the maternal perception of regular, painful uterine contractions and ends with the complete dilation of the cervix. Complete cervical dilation is the dilation necessary to allow movement of the fetus from the uterus into the vagina. At term gestation, 10 cm approximates complete cervical dilation. Preterm fetuses require less than 10 cm of cervical dilation. The second stage of labor begins with the complete dilation of the cervix and ends with the birth of the infant. The third stage begins with the birth of the infant and ends with the delivery of the placenta. The first stage of labor can be considered the cervical stage, the second stage the pelvic stage (reflecting the descent of the fetus through the pelvis), and the third stage the placental stage. Some authorities identify a fourth stage of labor, corresponding to the first postpartum hour, during which postpartum hemorrhage is most likely to occur.
Components of Labor and Delivery
When the events that occur during labor and vaginal delivery are considered, it is helpful to think about the following three components of the process: (1) the powers (uterine contractions and, in the second stage, the addition of voluntary maternal expulsive efforts); (2) the passageway (the bony pelvis and the soft tissues contained therein); and (3) the passenger (the fetus). The interaction of these three components determines the success or failure of the process.
The Powers
The uterus, which is a smooth muscle organ, contracts throughout gestation with variable frequency. The parturient verifies the onset of labor when she perceives regular, uncomfortable uterine contractions. In some women, the uterus remains relatively quiescent until the abrupt onset of labor. In others, the uterus contracts several times per hour for days without causing pain or even a clear perception of uterine contractions.
During labor, the frequency, duration, and intensity of uterine contractions increase. During early labor, the contractions may occur every 5 to 7 minutes, last 30 to 40 seconds, and develop intrauterine pressures (intensity) of 20 to 30 mm Hg above basal tone (10 to 15 mm Hg). Late in the first stage of labor, contractions typically occur every 2 to 3 minutes, last 50 to 70 seconds, and are 40 to 60 mm Hg in intensity. This higher intensity reflects a more widespread propagation of the contractions, with the recruitment of more myometrial cells.
Retraction accompanies contraction as the myometrial cells shorten. The walls of the upper, contractile portion of the uterus thicken. Cervical dilation and effacement reflect the traction placed on the cervix by the contracting uterus. The passive lower uterine segment enlarges and becomes thinner as cervical tissue is pulled over the fetal presenting part by traction from the upper portion of the uterus. At the end of the first stage of labor, no cervix is palpable on vaginal examination (corresponding to complete cervical dilation). If there is no mechanical obstruction, additional uterine contractions force the fetus to descend through the birth canal. At this time, the parturient perceives an urge to defecate (reflecting pressure on the rectum). Her expulsive efforts add to the force of uterine contractions to hasten descent and shorten the second stage of labor.
The Passageway
The fetus must be of such size and conformation that there is no mechanical mismatch with the bony pelvis. At times, an ovarian or uterine tumor (e.g., leiomyoma), cervical cancer, or a vaginal septum may impede passage of the fetus through the birth canal, but these situations are unusual.
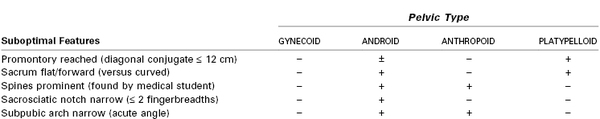
Four pelvic types have been described on the basis of the shape of the pelvic inlet (the plane bounded by the upper inner pubic symphysis, the linea terminalis of the iliac bones, and the sacral promontory) (Table 18-1).3 The type and size of the pelvis constitute important predictors of the success of vaginal delivery.
The most common pelvic type and the one theoretically best suited for childbirth is the gynecoid pelvis. The flexed fetal head presents a circle to the bony pelvis; a pelvis with gynecoid features best accommodates this circle. The inlet is round or oval, with the transverse diameter only slightly greater than the anteroposterior diameter. The pelvic sidewalls are straight and do not converge, the ischial spines are not prominent, the sacrum is hollow, and the subpubic arch is wide. The absence of prominent ischial spines is an important feature, because the distance between them—the transverse diameter of the midpelvis—is the narrowest pelvic dimension. The other pelvic types are less favorable for vaginal delivery.
Radiographic pelvimetry provides much more information regarding pelvic dimensions and features than can be obtained by clinical pelvimetry alone. However, it has only a limited place in clinical management because of its poor ability to predict a successful vaginal birth. In the absence of a history of pelvic fracture or musculoskeletal disease (e.g., a dwarfing condition), there are few circumstances in which the apparent pelvic anatomy precludes a trial of labor. A pelvis with smaller-than-average dimensions may be adequate for a particular fetus if the head is well-flexed, sufficient molding (i.e., overlapping of the unfused skull bones) has occurred, and the labor is strong; thus, radiographic pelvimetry does not always predict the presence or absence of cephalopelvic disproportion.4 Further, some risk is associated with radiographic pelvimetry. In addition to the potential for point mutations in the maternal oocytes and fetal germ cells, there is a small but apparently real increase in the incidence of malignancy and leukemia in children who were exposed to diagnostic radiation in utero. Some obstetricians use radiographic pelvimetry in cases of fetal breech presentation to assess whether fetal presentation, position, and lie are appropriate for vaginal delivery. The hope is to save a parturient from a long, futile labor and a hazardous delivery. Computed tomography and magnetic resonance imaging are associated with less or no ionizing radiation exposure, respectively; these methods are also more accurate than conventional radiographic pelvimetry. However, these methods also have limited ability to predict a successful vaginal delivery.
The Passenger
Fetal size and the relationship of the fetus to the maternal pelvis affect labor progress. The lie of the fetus (the relationship of the long axis of the fetus to the long axis of the mother) can be transverse, oblique, or longitudinal. In the first two, vaginal delivery is impossible unless the fetus is very immature.
The presentation denotes that portion of the fetus overlying the pelvic inlet. The presentation may be cephalic, breech, or shoulder. Cephalic presentations are further subdivided into vertex, brow, or face presentations, according to the degree of flexion of the neck. In more than 95% of labors at term, the presentation is cephalic and the fetal head is well flexed (i.e., vertex presentation).
The position of the fetus denotes the relationship of a specific presenting fetal bony point to the maternal pelvis. In vertex presentations, that bony point is the occiput. During vaginal examination, palpation of the sagittal suture and fontanels permits determination of the fetal position. Positions of the occiput in early labor are listed in Box 18-1. Other markers for position are the sacrum for breech presentation, the mentum for face presentation, and the acromion for shoulder presentation. (See Chapter 35 for a discussion of nonvertex presentations.)
The Mechanism of Labor
The mechanism of labor refers to the changes in fetal conformation and position (cardinal movements; Box 18-2) that occur during descent through the birth canal during the late first stage and the second stage of labor.
The first cardinal movement is engagement, which denotes passage of the biparietal diameter (BPD) (i.e., the widest transverse diameter of the fetal head) through the plane of the pelvic inlet. A direct clinical determination of engagement cannot be made, but obstetricians assume that engagement has occurred if the leading bony point of the fetal head is palpable at the level of the ischial spines. This is true because the distance between the leading bony point and the BPD is typically less than the distance between the ischial spines and the plane of the pelvic inlet. If the leading bony point is at the level of the spines, the vertex is said to be at zero station. If the leading bony point is 1 cm above the level of the spines, the station is designated as −1. Similarly, +1, +2, and +3 indicate that the leading bony point is 1, 2, and 3 cm below the ischial spines, respectively (Figure 18-1). At +5 station, delivery is imminent. Station refers to palpation of the leading bony point. Often marked edema of the scalp (i.e., caput succedaneum) occurs during labor. In such cases, the bony skull may be 2 to 3 cm higher than the scalp.
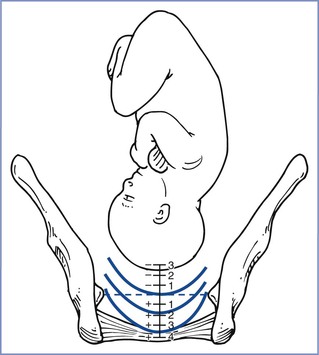
FIGURE 18-1 Stations of the fetal head. (Redrawn from Zlatnik FJ. Normal labor and delivery and its conduct. In Scott JR, DiSaia PJ, Hammond CB, Spellacy WN, editors. Danforth’s Obstetrics and Gynecology. 7th edition. Philadelphia, JB Lippincott, 1994:116.)
The second cardinal movement is descent, although it is artificial to separate descent from the other movements because descent occurs throughout the birth process. The third cardinal movement is flexion. A very small fetus can negotiate the average maternal pelvis without increased flexion. However, under the usual circumstances at term, the force from above and resistance from below enhance flexion of the occiput (Figure 18-2).
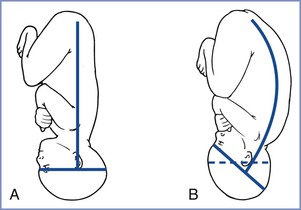
FIGURE 18-2 A, Relation of the head to the vertebral column before flexion. B, Relation of the head to the vertebral column after flexion. (Redrawn from Zlatnik FJ. Normal labor and delivery and its conduct. In Scott JR, DiSaia PJ, Hammond CB, Spellacy WN, editors. Danforth’s Obstetrics and Gynecology. 6th edition. Philadelphia, JB Lippincott, 1990:174.)
The fourth cardinal movement is internal rotation. At the level of the midpelvis, the fetus meets the narrowest pelvic dimension, which is the transverse diameter between the ischial spines. Because the BPD of the fetal head is slightly smaller than the suboccipitobregmatic diameter, in most labors the vertex negotiates the midpelvis with the sagittal suture in an anteroposterior direction. If this did not occur, a larger-than-necessary diameter would be forced to pass through the narrowest portion of the pelvis. Internal rotation describes the change in the position of the vertex from occiput transverse or oblique to anteroposterior. The occiput tends to rotate to the roomiest part of the pelvis; thus, in gynecoid pelves, the fetus is delivered in an occiput anterior position.
The next cardinal movement is extension, which occurs as the fetal head delivers (Figure 18-3). Subsequently, the occiput rotates to the side of the back (external rotation) as the shoulders pass through the midpelvis in an oblique diameter. The anterior shoulder moves under the pubic symphysis. With gentle downward traction, it passes from the birth canal, and expulsion of the remainder of the fetus occurs.
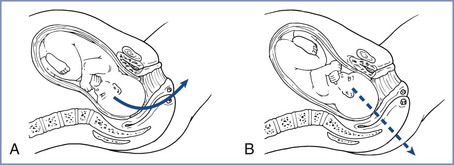
FIGURE 18-3 Vertex presentations. A, Occiput anterior position. B, Occiput posterior position. (Redrawn from Zlatnik FJ. Normal labor and delivery and its conduct. In Scott JR, DiSaia PJ, Hammond CB, Spellacy WN, editors. Danforth’s Obstetrics and Gynecology. 6th edition. Philadelphia, JB Lippincott, 1990:174.)
This description recounts events in the typical gynecoid pelvis. Abnormalities of the pelvis affect the mechanism of labor in specific ways. In an anthropoid pelvis, the anteroposterior diameter of the pelvic inlet exceeds the transverse diameter. Often internal rotation to the occiput posterior position rather than the occiput anterior position occurs. Because the pelvis is narrow transversely, further descent of the vertex occurs with the occiput in the posterior position. Delivery occurs with the occiput in the posterior position, or rotation to the occiput anterior position occurs just before delivery. In cases of persistent occiput posterior position, delivery occurs by flexion rather than extension of the fetal head (see Figure 18-3).
In platypelloid pelves, internal rotation may not take place. The widest diameter is the transverse diameter, and descent of the vertex may occur with the occiput in the transverse position; rotation to the occiput anterior position occurs only at delivery.
Clinical Course
Admission
When a patient enters the labor and delivery unit, the first question that must be asked is “why?” Did she come because of regular, painful uterine contractions; decreased fetal activity; vaginal bleeding; ruptured membranes; or some other reason? If the tentative diagnosis is labor, is she at term?
The time of the onset of labor and the presumed status of the membranes should be determined. Observation of the patient’s demeanor coupled with the assessment of cervical effacement and dilation will signal whether the patient is in early or advanced labor. Examination of the cervix is deferred in patients with vaginal bleeding in the second half of pregnancy, unless placenta previa has been ruled out by ultrasonography, to avoid exacerbation of bleeding. To prevent infection, cervical examination may also be deferred in patients with premature rupture of membranes and no labor.
The obstetrician also directs attention to the second patient: the fetus. Abdominal examination or ultrasonography is used to establish presentation and an estimate of fetal size. With most obstetric services, external electronic fetal heart rate (FHR) monitoring is used on admission to assess fetal condition. The baseline rate and variability and the presence or absence of accelerations and decelerations are of interest.
Subsequent Care
The maternal vital signs and FHR are recorded periodically. In some obstetric services, continuous electronic FHR monitoring is used universally; with other services, it is monitored via intermittent auscultation. In low-risk patients, recording the FHR every 30 minutes in the first part of the first stage of labor, every 15 minutes in the latter part of the first stage, and every 5 minutes in the second stage is perfectly acceptable. During early labor, the patient may ambulate or assume any position of comfort on the labor bed or in a chair. During advanced labor, many women choose to lie down. Choices concerning analgesia or anesthesia are made according to the patient’s wishes. Figure 18-4 shows a flow sheet (partogram) that may be useful for charting the course of labor.
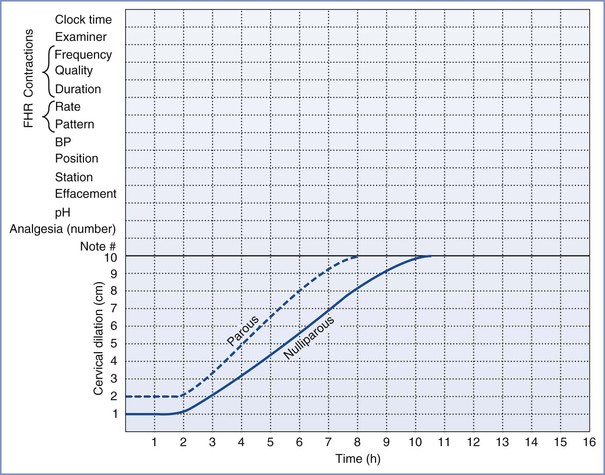
FIGURE 18-4 Flow sheet for charting labor progress. (From Zlatnik FJ. Normal labor and delivery and its conduct. FHR, fetal heart rate. BP, blood pressure. In Scott JR, DiSaia PJ, Hammond CB, Spellacy WN, editors. Danforth’s Obstetrics and Gynecology. 7th edition. Philadelphia, JB Lippincott, 1994:107.)
During labor, those providing obstetric care must focus on the following two critical questions:
1. Is the fetus tolerating labor in a satisfactory fashion, or is there evidence of fetal compromise (see Chapter 8)?
Labor Progress: The Labor Curve
One of the central tasks of those providing intrapartum care is to determine whether labor is progressing normally and, if not, to determine the significance of the delay and what the response should be. Parity is an important determinant of labor length. (Parity refers to previous pregnancies of at least 20 weeks’ gestation. A pregnant woman who is gravida 2, para 1 is pregnant for the second time, and her first pregnancy resulted in delivery after 20 weeks’ gestation.)
A generation of obstetricians is indebted to Emanuel Friedman, whose landmark studies of labor provide a framework for judging labor progress. Friedman’s approach was straightforward: He graphed cervical dilation on the y-axis and elapsed time on the x-axis for thousands of labors. He considered nulliparous and parous patients separately, and he determined the statistical limits of normal.5 The curve of cervical dilation over time is sigmoid shaped (Figure 18-5).
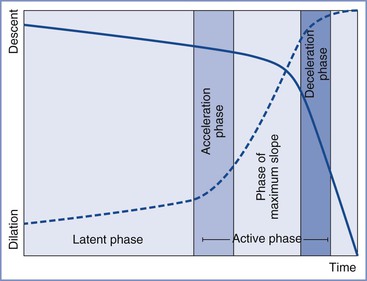
FIGURE 18-5 The Friedman curve. (From Friedman EA. Patterns of labor as indicators of risk. Clin Obstet Gynecol 1973; 16:172-83.)
Most authorities consider Friedman’s most important contribution to be his separation of the latent phase from the active phase of the first stage of labor. Many hours of regular, painful uterine contractions may take place with little appreciable change in the cervix. During this latent (or preparatory) phase, the cervix may efface and become softer. Quite abruptly, the active (or dilation) phase begins, and regular increases in cervical dilation are expected over time. The transition from the latent to the active phase of the first stage of labor does not occur at an arbitrary cervical dilation but rather is known—in retrospect—by change in slope of the cervical dilation curve. Peisner and Rosen6 evaluated the progress of labor for 1060 nulliparous women and 639 parous women. After excluding women with protracted or arrested labor, these researchers noted that 60% of the women had reached the latent-active phase transition by 4 cm of cervical dilation and 89% did so by 5 cm.
A nulliparous woman may labor for 20 hours without achieving appreciable cervical dilation; 14 hours is the limit of the latent phase in the parous woman. Difficulty in assigning length to the latent phase lies not with its end (determined from the change in slope of the cervical dilation curve) but rather with its beginning. The onset of labor is self-reported by the parturient. The uterus contracts throughout gestation, and the level of prelabor uterine activity and its perception are variable. Often both the patient and the physician are uncertain as to exactly when labor started.
According to Friedman, in the active phase of the first stage of labor, a nulliparous woman’s cervix should dilate at a rate of at least 1.2 cm per hour and a parous woman’s cervix should dilate at least 1.5 cm per hour. (The slopes of the dilation curves in Figure 18-5 represent the lower limits of normal.) If a woman’s cervix fails to dilate at the appropriate rate during the active phase of labor, she is said to have primary dysfunctional labor. Graphically, her cervical dilation “falls off the curve.” If cervical dilation ceases during a 2-hour period in the active phase of labor, secondary arrest of dilation has occurred.
More recent studies have reported slower rates of cervical dilation and engendered an ongoing transition toward the use of the “contemporary labor curve.”7,8 These curves reveal that cervical dilation is particularly slow prior to 6 cm and that the deceleration phase described by Friedman is usually absent. Therefore, 6 cm rather than 4 cm of cervical dilation more accurately reflects the start of the active phase in contemporary labor curves.8 Furthermore, in the active phase, absence of cervical change over at least 4 hours rather than 2 hours is a better definition of labor arrest. Estimates of contemporary rates of cervical dilation from 4 cm (when patients are often admitted) by parity are presented (Table 18-2). Nulliparous women have a slower cumulative rate of cervical dilation overall. However, prior to 6 cm of dilation, the times required to dilate 1 cm are similar between nulliparous and parous women.
TABLE 18-2
Rate of Spontaneous Cervical Dilatation by Parity
| Cervical Dilation | Nulliparous Median Time (h) (95th Percentile) | Parous Median Time (h) (95th Percentile) |
| First Stage | ||
| 4 to 5 cm | 1.3 (6.4) | 1.4 (7.1) |
| 5 to 6 cm | 0.8 (3.2) | 0.8 (3.4) |
| 6 to 7 cm | 0.6 (2.2) | 0.5 (1.8) |
| 7 to 8 cm | 0.5 (1.6) | 0.4 (1.2) |
| 8 to 9 cm | 0.5 (1.4) | 0.3 (1.0) |
| 9 to 10 cm | 0.5 (1.8) | 0.3 (0.9) |
| Second Stage | ||
| 10 cm to delivery (epidural) | 1.1 (3.6) | 0.4 (2.0) |
| 10 cm to delivery (no epidural) | 0.6 (2.8) | 0.2 (1.3) |
Modified from Zhang J, Landy HJ, Branch DW, et al.; for the Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010; 116:1281-7.
Abnormalities of the latent phase and active phase differ in associated factors, apparent causes, and significance. A prolonged latent phase is more likely if labor begins “before the cervix is ready.”5 Just as there is a wide range of prelabor uterine activity, so too is there a wide range of cervical softness, effacement, and dilation at the start of labor. In some women, appreciable cervical softening, effacement, and dilation take place in late pregnancy; thus, when clinical labor begins, the cervix may already be 3 to 4 cm dilated and completely effaced. Alternatively, in other women, there is no cervical effacement or dilation at the start of labor. Given these differences, it is not surprising that varying amounts of uterine contractile work are needed to cause dilation of the cervix. The most common factor associated with a prolonged latent phase is an “unripe” cervix at the start of labor. Some women with a prolonged latent phase are not in true labor at all but are in “false labor”; this diagnosis is made in retrospect. After hours of regular, painful contractions, uterine activity may cease without the occurrence of appreciable cervical dilation. Several hours or days later, the patient reappears in true labor. During the latent phase of labor, it is not known with certainty whether a woman is in true or false labor.
Recent studies refute the dictum that a prolonged latent phase alone is not associated with fetal compromise or cephalopelvic disproportion.9,10 An increased risk for cesarean delivery, chorioamnionitis, endometritis, excessive blood loss, depressed Apgar scores, and need for neonatal resuscitation have all been associated with a prolonged latent phase. An ongoing increase in the use of labor induction may be a mediating factor. Primary dysfunctional labor and arrest of dilation during the active phase may also indicate cephalopelvic disproportion.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree