Nutritional Issues: Toddler to Adolescent
Margaret Kirby and Praveen S. Goday
CHANGING REQUIREMENTS DURING DEVELOPMENT
The rate of physical growth during the toddler, preschool, and childhood years slows substantially when compared to the growth rate of an infant. A growth spurt that requires large increases in caloric intake occurs at puberty. Nutrient needs vary accordingly and substantially, as outlined in the dietary reference intakes (DRIs) for various age ranges (Chapter 23, eTable 23.1  ). Calorie needs have the greatest variability. The DRIs for energy for 1 to 2 years of age are based on age and weight, while those after 3 years include allowances for gender, height, and physical activity (Chapter 23, eTables 23.1 and 23.2
). Calorie needs have the greatest variability. The DRIs for energy for 1 to 2 years of age are based on age and weight, while those after 3 years include allowances for gender, height, and physical activity (Chapter 23, eTables 23.1 and 23.2  ). The general guidelines must be adjusted to account for individual variation in body size, stage of growth, physical activity, and state of health or illness.
). The general guidelines must be adjusted to account for individual variation in body size, stage of growth, physical activity, and state of health or illness.
Protein requirements are based on age and weight, with the requirement decreasing with age relative to weight but the total requirement increases with age. Additional factors, such as growth rate and state of health or illness, impact upon protein needs. It is important to recognize that recommended protein intakes assume high-quality protein providing amino acids essential to humans, such as eggs, milk, meat, poultry, and fish. If protein is primarily derived from lower-quality plant protein sources, the total requirement is increased. North American childhood diets generally contain more than adequate amounts of protein, but certain groups, including vegetarians, children with severe food allergies, those with limited access to foods, and children with severe food selectivity, are at risk for inadequate protein intake.
Fat requirements decrease from infancy through early childhood. Fat provides 40% to 50% of total calorie intake for infants. Restriction of fat intake in children under 2 years old is not advised because it may compromise growth.1 However, fat intake should gradually be decreased to approximately 30% by age 5 years and through adolescence. This decrease occurs as children transition from breast milk or infant formulas during the first year, whole milk during the second year, and then to lower fat milk after age 2. Intake of fruits, vegetables, and whole grains products should gradually decrease.
From age 5 years to early adolescence is a period of slow but steady growth. Dietary intakes of iron, calcium, zinc, and vitamins B6, A, D, and C are often less than recommended, but deficiencies are unlikely because most children in the United States have access to fortified foods. Ideally, apart from adequate intake of energy and protein, children obtain their vitamins and minerals from a variety of nutrient-dense foods, including whole grain cereals, fruits, and vegetables. The nutritional requirements of adolescents increase at the time of the pubertal growth spurt. The nutrient needs of individual teenagers differ greatly, being associated more with their growth rate than with chronological age.
Adolescents are at risk of deficiencies in two important minerals: iron and calcium. Rapid growth leads to an increased requirement for iron at a time when menstrual blood losses commence in adolescent females. The DRIs for iron for 14- to 18-year-olds are 11 mg/day in boys and 15 mg/day in girls (see Chapter 23, eTable 23.3  ). Teenagers should be encouraged to eat more iron-rich foods from animal sources (lean meats and fish) and from plant sources (beans, dark green vegetables, nuts, and iron-fortified cereals).
). Teenagers should be encouraged to eat more iron-rich foods from animal sources (lean meats and fish) and from plant sources (beans, dark green vegetables, nuts, and iron-fortified cereals).  Calcium requirements are discussed in the section that follows on “Bone Health.”
Calcium requirements are discussed in the section that follows on “Bone Health.”
Although the DRIs provide guidelines for vitamin and mineral intake throughout development, this is best achieved by encouraging ingestion of food choices from all major food groups, including dairy, protein sources, fruits, vegetables, and whole grains. Clinical signs of specific nutrient deficiencies are rare in the United States (see Table 23.3). 
COMMON CAUSES OF NUTRITIONAL INADEQUACY
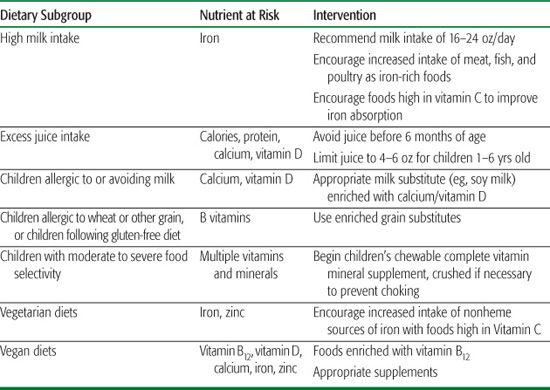
Table 27.1 lists subgroups of otherwise healthy young children whose feeding patterns place them at risk for specific nutrient deficiencies. Obtaining information from parents regarding their young children’s intake can be an important tool for screening for nutrient inadequacy. Children with chronic disorders that cause malabsorption of nutrients (see Chapter 408) or increased nutrient requirements due to excessive energy needs (eg, chronic infection, cardiac disorders, cerebral palsy, endocrine or metabolic disorders) may require substantial increases in caloric intake. Those with substantial protein loss from the skin, urine, or gastrointestinal tract may require increased protein intake. Micronutrient and vitamin requirements may be increased with specific disorders.
Table 27-1. Dietary Subgroups at Risk for Nutrient Deficiencies
CHANGES IN DIET DURING DEVELOPMENT
Family members provide the primary influence on the attitudes and behaviors of children with regard to food. Foods offered early in a child’s life shape the child’s future food preferences. Parents can also guide their children by modeling healthy food choices and portion sizes. Regular family mealtimes also encourage healthy eating habits. Regular consumption of meals and healthy snacks is essential for a child’s nutritional health. All children and adolescents should eat a diet containing whole-grain foods, fruits, and vegetables. Iron-containing foods should be encouraged, along with a diet rich in calcium and vitamin D. Breakfast is perhaps the most important meal but is the most often overlooked. Regular physical activity will help prevent obesity and osteoporosis. Snacks and fast foods are problematic when they are high in sugar or fats, and availability of these should be limited in quantity and frequency.
The diet changes from 100% liquid to a combination of liquids and solids as children advance from infancy through childhood. Texture advances parallel the development of oral-motor and swallowing skills (see Table 25.2). These transitions occur over the first several years of life and support the gradual development of independence in feeding, appropriate selection of foods, and independent acquisition of appropriate healthy foods.
 FOOD SELECTIVITY
FOOD SELECTIVITY
The development of feeding independence includes learning to express food preferences. A child’s food choices are strongly influenced by culture, family food preferences, food access, food restriction, and mealtime environment.3 This learning process can be associated with difficulties when children become overly picky and selective in their food choices. Approximately 20% of parents view their toddler as having eating problems.4 For most children, these problems consist of typical “picky eating” behavior and reflect a normal developmental process characterized by erratic appetite, easy distractibility at mealtimes, variable food intake, food jags, preference for sweets, and limited acceptance of vegetables and meats. Overly picky eating can usually be avoided if caregivers recognize these behaviors as part of normal development. Providing a supportive feeding environment that includes regular mealtime and snack schedules, limiting grazing behavior between meals, and offering a variety of nutritious foods in appropriate portion sizes generally prevents major problems from developing. Repeated exposures of nonpreferred foods facilitates acceptance of a healthy, culturally appropriate diet.
Some children become highly selective such that it may limit growth, impinge on normal social interactions, or have health consequences due to either macronutrient or micronutrient deficiencies. This may occur in otherwise healthy children (eg, refusal of solids with a choking phobia following an episode of choking5), but it is more frequent in children with autism spectrum disorder or developmental delays.2 In these instances, consultation with a pediatric dietitian to obtain a complete nutrient analysis and assure adequate nutrient intake is warranted. Behavioral therapy is usually very effective to promote expansion of the diet. In severe cases, this may require a structured inpatient program.
 RISK OF CHOKING WITH DIET ADVANCEMENT
RISK OF CHOKING WITH DIET ADVANCEMENT
Choking due to provision of inappropriate food textures and bite sizes is problematic during the initial introduction of solids and remains a concern up to the age of 4 years. Adequate skills for chewing and swallowing develop steadily through the first 3 years of life. Simple precautions recommended to prevent choking include the following: (1) Food textures should be gradually advanced from smooth to mashed or ground, and then to soft chewable table foods to support development of chewing skills. (2) Certain high-risk choking foods should be avoided for children younger than 3 years, including nuts, hard pieces of fruits and vegetables, popcorn, peanut butter, hot dogs, and round candy. (3) Children should not be allowed to eat while running or playing or while in the car, and they should be monitored at all times during meals and snacks.6
DIET EFFECTS ON HEALTH
Childhood dietary intake has myriad potential effects on long-term health, including potential impact on the later development of atherosclerosis, bone health, and metabolic syndrome. The World Health Organization recently recommended ranges for nutrient intakes in adults that are intended to reduce the long-term risk of chronic disorders such as atherosclerosis, diabetes, and osteoporosis.7 These include recommendations for total fat intake of 15% to 20% of total energy intake with less than 10% total as saturated fatty acids, and less than 1% as trans fatty acids; total carbohydrate intakes of 55% to 75% of total energy intake with less than 10% as added sugars to foods or as sugars from honey, syrups, or fruit juices; and 10% to 15% of energy being as protein. Cholesterol intakes of less than 300 mg/day and sodium chloride intakes of 2 to less than 5 g/day are also recommended.
Diet selections may affect specific health issues, such as defecation patterns, oral health, and bone health, in early childhood and adolescence.
 CONSTIPATION
CONSTIPATION
Dietary selections may contribute to problems of constipation, and constipation may impair appetite. Formula selection may alter stool consistency in infants. Formula containing prebiotics and probiotics may soften stools.8,9 Some infants with cow milk allergy may present with symptoms of constipation, and a change to a hydrolyzed formula improves symptoms.10 Iron-containing formulas do not contribute to constipation despite a widely held belief that they do so.11 Inadequate fiber and fluid in a young child’s diet can cause constipation.12 However, excess fiber intake can impair absorption of micronutrients. This can occur with high intake of phytate-containing foods, impairing absorption of calcium, iron, copper, magnesium, and zinc. Recommendations of the American Health Foundation for fiber intake for children over 2 years are endorsed by the American Academy of Pediatrics; recommended goals for fiber intake are calculated as the child’s age plus 5 to 10 g/day. For example, in a 3-year-old child, this would be equivalent to a recommended 8 to 13 g/day. 
 ORAL HEALTH
ORAL HEALTH
Adequate intake of protein; calories; vitamins A, C, and D; calcium; and fluoride affect the timing of tooth eruption, tooth size, or tooth mineralization.13,14 Poor oral health can impair a child’s intake, particularly of chewable foods. Dietary intake and feeding practices that negatively impact oral health include sleeping or grazing with a bottle of milk, juice, or liquid other than water (promoting “milk caries”); use of a pacifier dipped in sugar or other sweetened substance; and frequent grazing during the day, especially with sucrose-containing or other sweetened foods. Intake of excessive soda beverages is associated with poor oral health.15 Good oral hygiene and healthful dietary practices are positively associated with oral health.
 BONE HEALTH
BONE HEALTH
Peak bone mass is achieved during adolescence. Bone accrual during adolescence is vital to reduce the risk of later osteoporosis. During peak adolescent growth, calcium retention is, on average, about 200 mg/day in girls and 300 mg/day in boys. Because the efficiency of calcium absorption is only around 30%, the diet needs to supply adequate calcium to improve peak bone mass. The dietary reference intake for calcium in adolescents is 1300 mg/day. This can be achieved by consuming 3 cups per day (2 cups for children ages 2–8) of fat-free or low-fat milk or equivalent milk products; however, all children and adolescents need to consume 4 cups of vitamin D–fortified milk to achieve an adequate intake of vitamin D. Children who do not obtain their vitamin D from milk and other dietary sources should receive supplemental vitamin D of 400 IU/day. In addition to calcium and vitamin D, phosphorus is necessary for optimum bone health. The other crucial element is physical activity with weight-bearing exercise.
VEGETARIAN DIETS
Approximately 7 million Americans (2.3% of the US population) follow a vegetarian diet and consume no fish, meat, or poultry.16 The American Dietetic Association and the Food and Nutrition Board of the National Research Council consider properly planned, balanced vegetarianism to be an acceptable diet alternative if it is appropriately supplemented.17 Vegetarians typically are classified according to the types of protein they are willing to consume. Pollovegetarians will eat poultry but no red meat; pescovegetarians will eat only fish and other seafood; and lactoovovegetarians consume milk, dairy products, and eggs but no seafood or meat. The total or strict vegetarian, or vegan, will not eat any animal products, and he or she eats exclusively foods of plant origin. The risks of malnutrition are greatest in the vegan. For children on vegan diets, the greatest problem is attaining adequate caloric intakes because they consume foods with a low caloric density. Pregnant and lactating women, infants, and children are at most risk from these diets because they have increased nutritional demands from anabolism. Adolescents are also at particular risk; although dietary experimentation is part of the normal developmental process, when vegetarianism occurs at the time of the pubertal growth spurt and there is lack of knowledge regarding ingestion of a safe vegetarian diet, risks associated with vegetarianism increase in relation to the restrictiveness of the diet and/or lack of adequate planning. Children consuming a partial or semi-vegetarian diet are at little risk and are actually more likely to be complying with dietary recommendations for the prevention of chronic illness than are children on a typical Western diet.
Vegetarian diets that contain a complete source of protein containing the essential amino acids required by humans, such as eggs, milk, fish, or poultry, can easily be planned for nutritional adequacy.18 Diets that contain only plant proteins, which are incomplete (they do not contain a full complement of essential amino acids), require much more detailed planning. Typically, nuts, seeds, and grains (foods containing methionine) are combined with legumes (containing lysine) at the same meal so that adequate amounts of all essential amino acids are available for protein synthesis. This process, known as mutual supplementation, assures that there are no unduly limiting amino acids and that there is adequate dietary protein for protein synthesis. Recent research suggests that complementary proteins need not be consumed at the same meal. The consumption of essential amino acids over the course of the day should ensure adequate nitrogen retention and usage in healthy individuals. On the introduction of protein-rich foods into the infant’s diet, pureed tofu, legumes, or cottage cheese is recommended.
Intake of adequate minerals, especially iron, calcium, and zinc, is also difficult without consumption of animal products. Plant foods contain only nonheme iron, which is more susceptible to inhibitors of iron absorption than is heme iron (derived from meat, chicken, and fish). Therefore, even when a vegetarian diet consists of a higher total iron content than the standard Western diet, poor absorption of iron from plant sources can result in decreased body iron stores. Ingestion of high vitamin C–containing foods aids in nonheme iron absorption.
Adequate calcium intake is of particular concern for children who consume a vegan diet. Foods rich in calcium, such as calcium-fortified soy milk and juices, should be encouraged. Vegan diets also tend to be deficient in vitamin D, and it is therefore recommended that children be exposed to sunlight and provided with vitamin D–fortified foods to meet their needs. Infants and young children receiving a vegetarian diet should receive a sufficient amount (∼ 1000 mL) of milk (breast milk or formula) and dairy products to meet their vitamin D needs.19 The bioavailability of zinc from plant sources is low. As a result, vegetarians show a lower intake of zinc than do nonvegetarians. It is recommended that vegetarians strive to exceed the recommended dietary allowances for zinc. Supplementation of vitamins and minerals may be necessary to prevent deficiency.
Vitamin B12 is found only in products of animal origin, and this poses an important and serious risk to those vegetarians who do not consume animal products. Vegans must obtain vitamin B12 by using supplements or by eating vitamin B12–fortified foods, including soy milk, yeast, and cereals. Although adults may take several years to develop vitamin B12 deficiency, infants who are breast-fed by mothers who are marginally deficient themselves are likely to be at risk of vitamin B12 deficiency. Vegan mothers should be supplemented with vitamin B12 throughout pregnancy and lactation. Vegan infants are at risk of deficiencies in energy, protein, vitamin D, riboflavin, calcium, iron, and zinc apart from vitamin B12. A combination of these deficiencies can lead to poor growth and psychomotor retardation.20 It is recommended that infants and young children not receive a vegan diet.21
Dietary counseling is important to aid vegetarians in selection of appropriate food combinations to maintain good health. The more restrictive the diet and the younger the child, the greater is the need for professional nutritional advice.
VITAMIN AND MINERAL SUPPLEMENTATION
The use of vitamin and mineral supplements is fairly common in the United States with an estimated 54% of preschool children taking some type of supplement.22 Healthy children who eat adequate amounts of a variety of foods probably do not need supplements. The requirement for a supplement depends on a child’s nutrient intake, age, stage of growth, and medical status. If caregivers choose to give their child a supplement, a standard pediatric vitamin-mineral supplement with nutrients no higher than the DRI should be used, and megadoses avoided. The components of typical multivitamin supplements are listed in eTable 27.1.  Megavitamin and megamineral therapies are often advocated as “natural therapies” by various healers, but there is little evidence to support these contentions, and there are associated risks of such therapy.
Megavitamin and megamineral therapies are often advocated as “natural therapies” by various healers, but there is little evidence to support these contentions, and there are associated risks of such therapy.
Subgroups of young children who may be at nutritional risk and may benefit from an appropriate supplement prescription are (1) children with anorexia and poor growth, (2) children with a chronic illness such as cystic fibrosis, (3) children with multiple food allergies, (4) children receiving a vegetarian diet, and (5) children with severe food selectivity who avoid one or more basic food groups. Evaluation of the dietary intake of these children provides a guideline for appropriate supplement recommendation.
FOOD FADDISM AND NUTRITION QUACKERY
Food faddism and quackery involve unusual patterns of food behavior that are often enthusiastically promoted and/or adopted by their adherents. Typically, nutrition faddists and quacks claim that a particular food or nutrient has a specific therapeutic value, can cure disease, or has only positive effects. They downplay or totally ignore any negative or side effects. They may claim that dietary supplements such as vitamins or special nutrients are routinely needed to achieve a healthy balanced diet or that amino acid supplements have special values unto themselves and that supplements will enhance stamina, endurance, and muscle growth. A particular regimen often is claimed to achieve particular benefits (eg, to cure obesity). Frequently, the proposed beneficial product can be purchased through only one particular company or source, and proponents discredit “conventional” sources of information as not being credible, while providing testimonials or a celebrity endorsement as their evidence of efficacy.
Food faddism and quackery cause harm in many ways. They cost the economy billions of dollars a year in useless expense. Sometimes, patients are harmed indirectly through delays in seeking useful treatment or advice. Direct harm ensues when a so-called alternative treatment causes death, serious injury, or unnecessary suffering. Psychological harm is inevitable when vulnerable and sometimes desperate individuals blame themselves for ineffective therapy. Surprisingly, this may result in making them even more susceptible to future deception. Finally, there is an incalculable harm to our society when the general public uses erroneous and unfounded beliefs as a foundation for unrealistic expectations about nutrition and health. These unrealistic expectations often seriously undermine confidence in the scientific approach to problems in general and to legitimate providers of health care in particular.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


