Normal Structure and Function of the Gastrointestinal Tract
Alan N. Mayer
ANATOMY AND HISTOLOGY
The gastrointestinal (GI) tract is a continuous tube beginning at the mouth and ending at the anus (Fig. 381-1). Its main function is to digest food and absorb nutrients and fluid. It is subdivided into 4 regions: (1) esophagus, (2) stomach, (3) small intestine, and (4) large intestine. The liver and pancreas directly communicate with the GI tract via ducts that join with the duodenum, the most anterior segment of small intestine. At the cellular level, the tissue architecture of the gut tube is similar throughout, consisting of 4 concentric layers.1 From inner to outer they are (1) mucosa, (2) submucosa, (3) muscularis propria (externa), and (4) adventitia or serosa. The mucosa is composed of epithelium, lamina propria, and muscularis mucosae (Fig. 381-2).
The epithelium throughout the GI tract is a highly proliferative tissue because it continuously undergoes renewal. The source of new epithelial cells is a stem cell compartment located in the most basal zone.2
The boundary between the epithelium and the lamina propria is formed by the basement membrane. It is made of extracellular matrix proteins elaborated by both the epithelium and the lamina propria cells. It serves an important function in the maintenance of a differentiated, functional epithelium.
The lamina propria contains fibroblasts and myofibroblasts that regulate epithelial proliferation and differentiation. Also in the lamina propria are immune cells, nerves, lymphatics, and blood vessels, all of which support the epithelium and guard against invasion by pathogens. Embedded within the lamina propria are epithelial glands that are contiguous with the surface epithelium and that open into the lumen. The muscularis mucosae is a thin band of smooth muscle that separates the mucosa layer from the underlying submucosa and provides additional structure and motility to the mucosa.
The submucosa consists of supporting collagenous fibers, larger blood vessels, lymphatics, nerve fibers and ganglia, and occasional lymphoid follicles. In the duodenum, the submucosa also contains Brunner glands that secrete bicarbonate to neutralize gastric acidity.
The muscularis propria consists of 2 bands of smooth muscle with an intervening layer of nerves and ganglia, the myenteric plexus. Coordinated contraction and relaxation of the circular (inner) and longitudinal (outer) muscle layers is required for gut peristalsis.
The outermost layer, the adventitia, consists of connective tissue and adipose. In many areas, the GI tract is surrounded completely by a sheath of mesentery or serosa, which tethers the gut tube to the body wall and serves as a conduit for major blood vessels and lymphatics.
Despite the overall similar architecture, specialization of the tissue layers, particularly the mucosa, confers specific functions to the different anatomic regions of the GI tract.
 ESOPHAGUS
ESOPHAGUS
The esophagus extends from the posterior pharynx to the stomach, serving as a conduit for the passage of food. Esophageal epithelium is nonkeratinized, stratified, and squamous, designed to withstand abrasion as ingested food passes through it. Submucosal glands secrete mucins for lubrication and acid protection.
The muscularis propria of the esophagus is composed of a mixture of skeletal and smooth muscle fibers in the upper third, mixed fibers in the middle third, and smooth muscle in the distal third. Both the upper and lower openings of the esophagus remain closed by the tonic contraction of the muscularis propria. These sphincters relax in a coordinated fashion during swallowing. The lower esophageal sphincter prevents regurgitation of acidic stomach contents and ingested food back into the esophagus. 
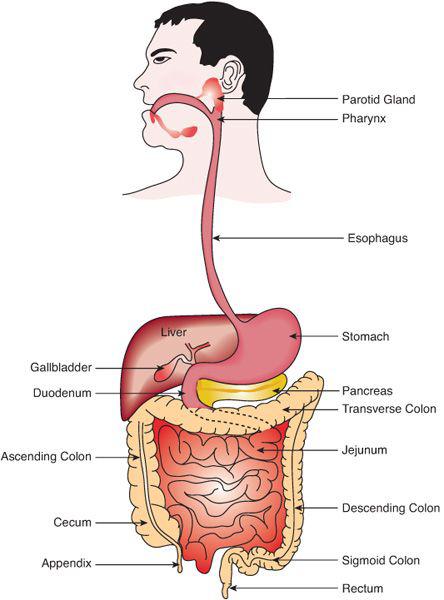
FIGURE 381-1. The gastrointestinal tract.
 STOMACH
STOMACH
The stomach serves as a reservoir for ingested food and, through a combination of physical movement and chemical digestion, breaks down food into smaller particles. The largest region of the stomach is the gastric body, which is characterized grossly by thick mucosal folds or rugae (eFig. 381.1  ). The gastric body or corpus is the acid-secreting portion of the stomach. It is characterized at endoscopy by thick mucosal folds or rugae; it extends distally to the incisura on the lesser curvature. The fundus is the dome-shaped area immediately above the gastric body and, like the corpus, is lined with oxyntic mucosa. The body is lined by mucosa containing deep glands that contain acid-secreting parietal cells and pepsinogen-secreting chief (oxyntic) cells. Secreted acid serves as a barrier to bacterial colonization of the small intestine and enables the enzyme pepsin to initiate the digestion of proteins. Parietal cells also secrete intrinsic factor, which is necessary for the absorption of vitamin B12 in the ileum.
). The gastric body or corpus is the acid-secreting portion of the stomach. It is characterized at endoscopy by thick mucosal folds or rugae; it extends distally to the incisura on the lesser curvature. The fundus is the dome-shaped area immediately above the gastric body and, like the corpus, is lined with oxyntic mucosa. The body is lined by mucosa containing deep glands that contain acid-secreting parietal cells and pepsinogen-secreting chief (oxyntic) cells. Secreted acid serves as a barrier to bacterial colonization of the small intestine and enables the enzyme pepsin to initiate the digestion of proteins. Parietal cells also secrete intrinsic factor, which is necessary for the absorption of vitamin B12 in the ileum.
The gastric antrum extends from the incisura to the pylorus with a smooth (ie, nonrugose) mucosal surface. Glands in the antrum differ from those in the body in that they produce less acid, more mucus, and contain specialized cells that secrete hormones known as enterochromaffin cells. The stomach is also distinguished by having 3 layers in the muscularis externa—oblique, circular, and longitudinal—which enable vigorous mixing of ingested food. An important hormone secreted by the antrum is gastrin, which stimulates parietal cells to secrete acid. The muscularis propria of the stomach uniquely contains 3 layers—an outer longitudinal, inner circular, and innermost oblique layer—that allow dramatic variation in stomach size and contractile patterns. The blood supply of the stomach comes from 5 arteries, all of which arise from the celiac axis and anastomose freely on the external surface. Venous return is through the portal venous system.
 SMALL INTESTINE
SMALL INTESTINE
The small intestine is the largest section of the gastrointestinal tract and is responsible for the bulk of its digestive and absorptive functions. The first portion, the duodenum, extends from the pylorus to the ligament of Treitz, forming a C-loop around the head of the pancreas. The common bile duct and pancreatic ducts enter the duodenum at the ampulla of Vater. The remainder of the small bowel is approximately 200 to 250 cm in length in the term newborn infant, and it reaches 350 to 600 cm in the adult. The proximal 40% is conventionally called the jejunum, and the remainder the ileum.
The luminal surface of the small intestine is covered by a lawn of fingerlike projections called villi, which increase the surface area for digestion and absorption (eFig. 381.2  ). Invaginations at the bases of the villi are the crypts of Lieberkühn where epithelial stem cells are located. Every 5 to 7 days, the epithelium is continuously replenished by new cells derived from the crypts. There are 4 epithelial subtypes: enterocytes, goblet cells, enteroendocrine cells, and Paneth cells. Enterocytes account for over 90% of the epithelial cells. At the sub-cellular level, enterocytes have a specialized apical region called the brush border that contains numerous digestive enzymes and transport proteins. Goblet cells secrete mucus and enteroendocrine cells secrete a wide spectrum of hormones. Lymphoid aggregates are present throughout the submucosa and occasionally extend into the mucosa. Their size and number increase in the ileum, where they are known as Peyer patches.
). Invaginations at the bases of the villi are the crypts of Lieberkühn where epithelial stem cells are located. Every 5 to 7 days, the epithelium is continuously replenished by new cells derived from the crypts. There are 4 epithelial subtypes: enterocytes, goblet cells, enteroendocrine cells, and Paneth cells. Enterocytes account for over 90% of the epithelial cells. At the sub-cellular level, enterocytes have a specialized apical region called the brush border that contains numerous digestive enzymes and transport proteins. Goblet cells secrete mucus and enteroendocrine cells secrete a wide spectrum of hormones. Lymphoid aggregates are present throughout the submucosa and occasionally extend into the mucosa. Their size and number increase in the ileum, where they are known as Peyer patches.
 LARGE INTESTINE
LARGE INTESTINE
The large intestine recovers fluids and electrolytes from the gastrointestinal tract lumen before their loss in feces with undigestible materials. The large intestine begins at the cecum, from which extends a narrow terminal extension called the vermiform appendix. It includes the ascending, transverse, and descending colons, the sigmoid, and the rectum, ending at the anus (Fig. 381-1). The epithelial lining contains absorptive cells with microvilli, which increase absorptive area. Mucosal glands have an abundance of mucus-producing goblet cells and rare endocrine cells. The muscularis propria contains circular and longitudinal muscle layers throughout, the latter of which are condensed into 3 thick bundles termed teniae coli.
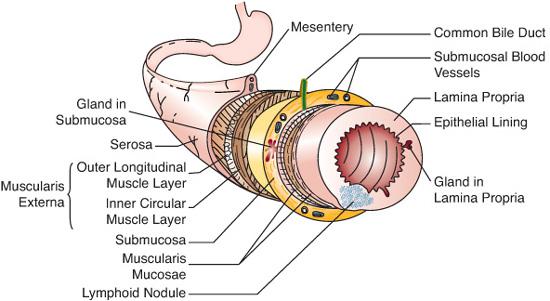
FIGURE 381-2. Tissue architecture of the gastrointestinal tract. (From Gartner L, Hiatt J. Color textbook of histology. Philadelphia: Saunders; 2007.)
EMBRYOLOGY AND DEVELOPMENTAL BIOLOGY
The gastrointestinal (GI) tract is a composite structure with components derived from all 3 germ layers. The inner epithelial lining is derived from the endoderm, but the surrounding layers come from mesoderm and ectoderm. Development of the GI tract can be divided into distinct phases: formation of the endoderm, morphogenesis and patterning of the gut tube, and organ morphogenesis and terminal differentiation.3-5
 EARLY DEVELOPMENT
EARLY DEVELOPMENT
During the third week of gestation, the endoderm forms during gastrulation, resulting in a trilaminar disk.7 A number of factors that promote endoderm formation are conserved across phyla, including Nodal signaling factors that direct a subset of blastomeres into the endoderm lineage. Nodals are members of the transforming growth factor (TGF)-β family of signaling molecules; they direct the expression of homeobox transcription factors in the MIX family. Other transcription factors acting downstream of Nodals include GATA4, GATA5, and GATA6, the homeobox factor SOX17, and the forkhead transcription factors FOXA1, FOXA2, and FOXA3.6 The gut tube forms by folding during the fourth week of gestation (eFig. 381.3  ).8 The ectoderm and endoderm of the trilaminar germ disk grow at different rates, which results in its folding inward to form a tube lined by endoderm, with ectoderm on the embryonic external surface. The endoderm-lined tube closes completely to form the foregut and hindgut, which terminate at the buccopharyngeal membrane and cloacal membranes respectively. The midgut portion of the tube remains open to the yolk sac until the sixth week of gestation, when the neck of the yolk sac is reduced to a slim stalk, the omphaloenteric (vitelline) duct. Persistence of the omphaloenteric duct can result in a spectrum of anomalies, ranging in severity from omphalocele to the more common Meckel diverticulum.
).8 The ectoderm and endoderm of the trilaminar germ disk grow at different rates, which results in its folding inward to form a tube lined by endoderm, with ectoderm on the embryonic external surface. The endoderm-lined tube closes completely to form the foregut and hindgut, which terminate at the buccopharyngeal membrane and cloacal membranes respectively. The midgut portion of the tube remains open to the yolk sac until the sixth week of gestation, when the neck of the yolk sac is reduced to a slim stalk, the omphaloenteric (vitelline) duct. Persistence of the omphaloenteric duct can result in a spectrum of anomalies, ranging in severity from omphalocele to the more common Meckel diverticulum.
 GUT PATTERNING AND MORPHOGENESIS
GUT PATTERNING AND MORPHOGENESIS
The primitive gut tube can be divided into 3 anatomic segments, the foregut, midgut, and hindgut, based on its blood supply. The fore-gut gives rise to the pharynx, respiratory tract, esophagus, stomach, and proximal duodenum (eFig. 381.4  ). At approximately 3 weeks of gestation, the respiratory diverticulum or lung bud develops as a ventral outpouching of the foregut. A septum forms in the foregut to separate the trachea from the prospective esophagus, and defects at this stage can lead to esophageal atresia or tracheoesophageal fistula.8
). At approximately 3 weeks of gestation, the respiratory diverticulum or lung bud develops as a ventral outpouching of the foregut. A septum forms in the foregut to separate the trachea from the prospective esophagus, and defects at this stage can lead to esophageal atresia or tracheoesophageal fistula.8
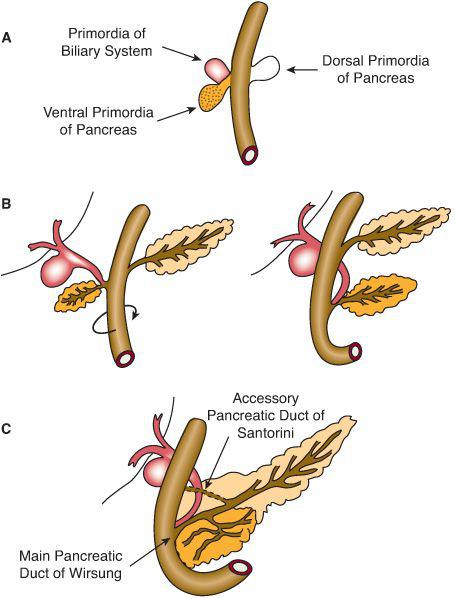
During the fifth week of embryonic development, the dorsal wall of the stomach grows faster than the ventral wall, thus forming the greater and lesser curvatures of the stomach. The stomach and liver rotate around a craniocaudal axis so that by the eighth week of gestation the greater curvature of the stomach lies to the left and the liver to the right side of the abdominal cavity. The liver, gallbladder, and ventral pancreatic bud develop from a ventral bud immediately caudal to the prospective stomach (Fig. 381-3). A separate dorsal pancreatic bud gives rise eventually to the body of the pancreas. Rotation of the duodenum results in the fusion of the pancreatic buds to form a single pancreas, followed by the unification of the pancreatic and bile ducts by the sixth week. Failure of these processes can result in annular pancreas or pancreas divisum, respectively.9
The jejunum, ileum, cecum, appendix, proximal colon, and distal half of the duodenum are derived from the midgut, supplied by the superior mesenteric artery. As the midgut elongates, there is insufficient space inside the peritoneal cavity, so it herniates into the extraembryonic coelom through the umbilical cord.8 During this period, the gut rotates counterclockwise about the axis of the superior mesenteric artery, a total of 270 degrees. After it returns into the abdominal cavity, it attaches to the posterior abdominal wall via its mesentery in a diagonal pattern extending from the left upper quadrant to the right lower quadrant (eFig. 381.5  ). Failure of midgut rotation or fixation of the mesentery results in malrotation, which can predispose to midgut volvulus around the superior mesenteric artery.
). Failure of midgut rotation or fixation of the mesentery results in malrotation, which can predispose to midgut volvulus around the superior mesenteric artery.
The hindgut gives rise to the left one third of the transverse colon, descending colon, and rectum. The cloaca is a transient structure derived from the end of the primitive hindgut. Between the fourth and sixth weeks, the cloacal lumen divides into the rectum posteriorly and the urogenital sinus anteriorly. The urogenital sinus gives rise to the bladder, urethra, and vestibule of the vagina. The rectum is contiguous with a depression in the ectoderm called the anal pit; this pit breaks down to permit continuity between the endodermal lining of the rectum and the ectodermal lining of the anus.7
 MOLECULAR GENETICS OF INTESTINAL DEVELOPMENT
MOLECULAR GENETICS OF INTESTINAL DEVELOPMENT
Numerous molecular pathways have been associated with the patterning, cytodifferentiation, and proliferation of intestinal enterocytes. These include the Wnt, TGF-β, and hedgehog signaling pathways. In addition, transcription factors known to be involved include the gata, forkhead, caudal-related (CDX), and HOX families as discussed in more detail in additional text on DVD.10
 GASTROINTESTINAL MUSCLE DEVELOPMENT
GASTROINTESTINAL MUSCLE DEVELOPMENT
The muscle coat of the gastrointestinal tract consists of the muscularis mucosa, an inner circular layer, and an outer longitudinal layer. The thickness of each muscle layer increases through gestation and after birth. The inner layer of circular muscle consists of a 3-cell to 8-cell-thick specialized layer of fibroblasts and muscle cells containing numerous junctions between cells. Termed the interstitial cells of Cajal, this layer generates the basic electrical rhythm, or slow waves, of the gastrointestinal tract.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


