Background
Emergency department use is common among pregnant women. Nonurgent emergency department use may represent care that would be better provided by an established obstetric provider in an ambulatory setting.
Objective
The objective of the study was to identify sociodemographic factors associated with nonurgent emergency department use in pregnancy.
Study Design
This is a cross-sectional study of women recruited during their postpartum hospitalization. Data regarding prenatal care and emergency department visits were collected from medical records; participants completed a survey with questions regarding demographics and emergency department use. Urgency of an emergency department visit was prespecified based on a priori criteria abstracted from medical record review. Women with any nonurgent emergency department use were compared with women without nonurgent emergency department use. Logistic regression was performed to identify factors associated with nonurgent emergency department use.
Results
Two hundred thirty-three women participated in this study; 197 (84%) received care in the emergency department during pregnancy. Eighty-three women (35.6%) had at least 1 visit to the emergency department that was nonurgent. In a regression analysis, the increased odds of nonurgent emergency department use was associated with a preferred language other than English (odds ratio, 2.02; 95% confidence interval,1.01–4.05) and lack of private insurance (odds ratio, 5.55; 95% confidence interval, 2.54–12.12). The 2 most common reasons for presentation to the emergency department were concern that there was an emergency (45%) or being referred by a health care provider (36%).
Conclusion
Women frequently use the emergency department during pregnancy, including visits for nonurgent indications. Identifying risk factors for nonurgent emergency department use in pregnancy is important for identifying women likely to use the emergency department, including for nonurgent visits, and the development of strategies to decrease nonurgent emergency department utilization in pregnancy.
Emergency departments (EDs) nationwide are being increasingly utilized for nonemergent medical care. Although many patients seeking medical care in the ED need urgent or emergent medical care, up to one third of patients seen in the ED have nonurgent problems that could have potentially been addressed in an outpatient setting. For chronic illnesses and conditions, continuity of care with an outpatient provider leads to less costly and higher-quality care for the patient. Nonurgent care received through the ED is usually not in the best interest of the patient or the health care system.
ED utilization among pregnant women is common despite the fact that pregnant women are generally regarded as having access to insurance and regularly scheduled medical care at outpatient prenatal visits. A national cohort study found that pregnancy-related problems were the fifth most common reason for presentation to the ED and the fourth most common ED discharge diagnosis in women aged 15–65 years old. Among a smaller cohort of pregnant women, 50% accessed the ED for care during their pregnancy. Despite this use, details on the utilization of ED care among pregnant women are limited.
Although many pregnant women may have an urgent or emergent medical problem that requires prompt ED evaluation, others likely choose to use the ED for nonurgent reasons. Nonurgent issues may be better addressed by the patient’s usual prenatal care provider in an outpatient setting rather than in the ED.
Understanding factors associated with urgent and nonurgent ED visits during pregnancy could assist in the identification of women at risk of using the ED for nonurgent indications and aid in the development of strategies to prevent identified women from seeking nonurgent care from an ED, optimizing both ED and prenatal care. The objective of this study was to identify sociodemographic characteristics associated with urgent and nonurgent ED use in a population of pregnant women.
Materials and Methods
This was a cross-sectional study of postpartum women who delivered in July and August 2012 at Women and Infants Hospital (WIH) in Providence, RI. WIH is a free-standing women’s hospital with an associated women’s ED, specializing in the evaluation of acute obstetric and gynecological issues. Labor and delivery triage is located and managed within this ED unit.
All women who delivered at WIH during the study period were screened for eligibility. Women were eligible for inclusion if they met the following criteria: (1) were older than 18 years at the time of delivery, (2) spoke English or Spanish, (3) were available in their hospital room for eligibility screening, (4) were willing to participate, and (5) were able to give informed consent. Women were excluded if they delivered a stillborn or previable fetus or if they obtained prenatal care from a solo practitioner, a maternal-fetal medicine subspecialist, or an obstetrician who was not affiliated with WIH.
Women determined to be eligible by medical record prescreen were approached on postpartum day 1 or postoperative day 2. Trained study staff performed a second screen to determine final eligibility and offer participation to eligible women. Informed consent was signed by all participants. The WIH Institutional Review Board approved the study (Institutional Review Board number 12-0029).
Study staff reviewed the medical record of participants and collected specific data about WIH ED visits during pregnancy. An urgent visit was defined as meeting any of the following criteria: (1) hospital admission or transfer to another facility, (2) greater than 1 L of intravenous fluids received, (3) intravenous medications received, (4) documentation that the participant was sent to the ED by a provider or other facility, or (5) the chief complaint was a sign of a pregnancy complication or labor.
The Emergency Severity Index assigned was collected but not used in our categorization of urgency. Signs of a pregnancy complication or labor included vaginal bleeding in the second or third trimester, leaking fluid, regular frequent painful contractions (defined as every 5 minutes or less), or decreased fetal movement at greater than 20 weeks’ gestational age.
Ultimately, we were not able to reliably determine from the record whether an ED visit was prompted by provider referral; therefore, this criterion was not used to determine the urgency of the visit. Based on these criteria participants were categorized into 2 groups: women with any nonurgent ED use during pregnancy and women without nonurgent ED use, defined as no ED use or urgent ED use only.
Information about maternal demographics and prenatal care was also collected from the medical record. Sociodemographic and clinical data collected included maternal age; parity; insurance type (none, public, or private); provider type (private practice vs community based, which included hospital-based clinics and community health centers); number of prenatal visits; missed appointments; antepartum complications; mode of delivery; use of ancillary services during pregnancy; and laboratory testing.
The adequacy of prenatal care was determined using the Adequacy of Prenatal Care Utilization Index, which combines gestational age at the time of the initiation of prenatal care with the proportion of prenatal visits attended to calculate the adequacy of prenatal care.
Prenatal care was categorized as inadequate if the initiation occurred after 14 weeks’ gestational age and/or the participant attended fewer than 50% of the expected visits. All other categories required prenatal care initiation prior to 14 weeks’ gestational age and were assigned based on the attendance at the expected prenatal care visits with categorization of intermediate, adequate, or adequate-plus prenatal care pertaining to attendance at 50–79%, 80–109%, or ≥110% of expected visits, respectively.
At the time of enrollment, participants completed a health and demographic questionnaire constructed by study investigators. The questionnaire included 40 questions regarding medical history, prenatal care, and demographic characteristics including race, educational level completed, socioeconomic status, living situation, and social supports. Language preference was defined by the following survey question: “What language do you use the most (with family and friends)?”
Participants were also asked whether they used the ED during pregnancy. If they reported ED use, they were asked to recall details about a maximum of 3 ED visits, including symptoms that prompted them to present to the ED, why they chose the ED for their care, whether they called their provider prior to presenting to the ED, how they got to the ED, and with whom they presented to the ED. Participant self-reported details about ED use during pregnancy were not linked to specific ED episode data collected through retrospective chart review.
Lastly, participants were also administered the Test of Functional Health Literacy–Short Version. This is a self-administered questionnaire validated in both English and Spanish for the assessment of health literacy. Similar to other studies, we combined marginal and inadequate scores to represent limited health literacy. Limited health literacy suggests an inability to read and interpret health-related information.
Data were analyzed using SAS 9.3 (SAS Institute, Cary, NC). Categorical variables were analyzed using a χ 2 or Fisher exact test, and continuous variables were analyzed using a Student t test and Wilcoxon rank sum tests. Women categorized as without nonurgent ED use were compared with those with any nonurgent ED visits. A logistic regression was performed to estimate the association between selected demographic characteristics and nonurgent ED use during pregnancy.
All demographic characteristics that were associated in bivariate analyses ( P < .05) with nonurgent ED use during pregnancy were considered for incorporation into a full model. To ensure a sufficient number of outcomes per covariate (10 or more), the number of predictor variables was reduced by removing variables highly correlated with other covariates. When a strong association (phi coefficient or Cramer’s V ≥0.4) between potential covariates was identified (such as insurance and provider status), we selected the variable more strongly associated with the outcome in the unadjusted models. We used the final full model to estimate odds ratios and 95% confidence intervals. Model fit was assessed by the c-statistic and Hosmer-Lemeshow goodness-of-fit test.
Results
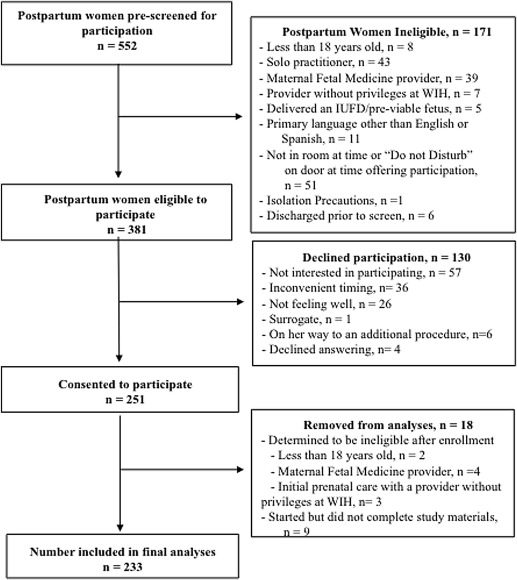
Between July and August 2012, 552 postpartum women were screened for eligibility. One hundred seventy-one women were ineligible or unavailable at the time of recruitment. Of the 381 eligible women, 251 women (65.9%) agreed to participate in the study and 233 women completed the health literacy screen and questionnaire (see Figure ). Of the women who completed participation, 197 (84.5%) used the ED during pregnancy for a total of 498 ED visits. Thirty-six women (15.5%) had no recorded ED use and 83 women (35.6%) had at least 1 ED visit that was categorized as nonurgent.
Several differences were noted between the women with any nonurgent ED visits and the women without nonurgent ED visits ( Table 1 ). Compared with the women without nonurgent ED visits, the women with any nonurgent ED visits were younger (26 vs 31 years, P < .001), more likely to identify as Hispanic (49.4 vs 18.7%), to have public insurance (86.7 vs 41.3%, P < .001), to make less than $20,000 per year (51.8 vs 27.3%, P < .001), to be single (19.3 vs 6.7%, P = .003), and to have a community-based obstetrician-gynecologist provider (38.6 vs 20.8%, P = .004).
| Variable | Total a | Any nonurgent ED use a | Without nonurgent ED use a | P value |
|---|---|---|---|---|
| Total, n (row %) | 233 | 83 (35.6) | 150 (64.4) | |
| Age, median (range) | 29 (18–44) | 26 (18–42) | 31 (18–44) | < .001 |
| Parity, n, % | ||||
| Primiparous | 96 (41.2) | 30 (36.1) | 66 (44.0) | .243 |
| Multiparous | 137 (58.8) | 53 (63.9) | 84 (56.0) | |
| GA at delivery | ||||
| Median (range) | 39.0 (26.0–41.0) | 39.0 (26.0–41.0) | 39.0 (33.0–41.0) | .013 |
| [IQR] | [38.0-40.0] | [38.0-39.0] | [39.0-40.0] | |
| Race, n, % b | ||||
| Black or African American | 14 (6.0) | 4 (4.8) | 10 (6.7) | < .001 |
| Hispanic | 69 (29.6) | 41 (49.4) | 28 (18.7) | |
| White, non-Hispanic | 126 (54.1) | 30 (36.1) | 96 (64.0) | |
| Other (including no selection) | 24 (10.3) | 8 (9.6) | 16 (10.7) | |
| Language used at home, n, % b | ||||
| English | 173 (74.2) | 48 (57.8) | 125 (83.3) | < .001 |
| Spanish | 43 (18.5) | 28 (33.7) | 15 (10.0) | |
| Both | 14 (6.0) | 6 (7.2) | 8 (5.3) | |
| Other | 3 (1.3) | 1 (1.2) | 2 (1.3) | |
| Insurance, n, % | ||||
| None/public | 134 (57.5) | 72 (86.7) | 62 (41.3) | < .001 |
| Private | 99 (42.5) | 11 (13.3) | 88 (58.7) | |
| Provider, n, % | ||||
| Community | 63 (27.2) | 32 (38.6) | 31 (20.8) | .004 |
| Private (all others) | 169 (72.8) | 51 (61.4) | 118 (79.2) | |
| Education level, n, % b | ||||
| Up to and including completion of high school or GED program | 92 (39.5) | 50 (60.2) | 42 (28.0) | < .001 |
| Any education after high school | 141 (60.5) | 33 (39.8) | 108 (72.0) | |
| Health literacy, n, % | ||||
| Marginal/inadequate | 12 (5.2) | 7 (8.5) | 5 (3.3) | .120 |
| Adequate | 220 (94.8) | 75 (91.5) | 145 (96.7) | |
| Relationship status, n, % b | ||||
| Partnered | 207 (88.8) | 67 (80.7) | 140 (93.3) | .003 |
| Single/divorced/separated | 26 (11.2) | 16 (19.3) | 10 (6.7) | |
| Annual income, n, % b | ||||
| Unemployed or <$20,000 | 84 (36.1) | 43 (51.8) | 41 (27.3) | < .001 |
| $20,000 or greater | 127 (54.5) | 28 (33.7) | 99 (66.0) | |
| No answer | 22 (9.4) | 12 (14.5) | 10 (6.7) |
a May not equal the total because of missing data
Women with any nonurgent ED use were also less likely to be white (36.1 vs 64.0%), to speak only English at home (57.8 vs 83.3%, P < .001), and to have completed education beyond high school (39.8 vs 72%, P < .001). The observed difference in health literacy was not statistically significant.
More women with nonurgent ED visits reported an unplanned pregnancy compared with women without nonurgent ED use (47.0 vs 32.0%, P = .024) ( Table 2 ). The timing of the initiation of prenatal care was similar in both groups, with the majority of women (82.5%) seeking care before the second trimester of pregnancy. Women with any nonurgent ED use were more likely than women without nonurgent ED use to have missed a prenatal care visit (32.5% vs 15.0%, P = .002).



