Background
Urologic cancer has a lower prevalence in women compared with men; however, there are no differences in the recommended evaluation for women and men with microscopic hematuria.
Objectives
The purpose of this study was to identify risk factors that are associated with urologic cancer in women with microscopic hematuria and to determine the applicability of a hematuria risk score for women.
Study Design
We conducted a retrospective cohort study within an integrated healthcare system in Southern California. All urinalyses with microscopic hematuria (>3 red blood cells per high-power field) that were performed from 2009–2015 were identified. Women who were referred for urologic evaluation were entered into a prospective database. Clinical and demographic variables that included the presence of gross hematuria in the preceding 6 months were recorded. The cause of the hematuria, benign or malignant, was entered into the database. Cancer rates were compared with the use of chi-square and logistic regression models. Adjusted risk ratios of urologic cancer were estimated with the use of multivariate regression analysis. We also explored the applicability of a previously developed, gender nonspecific, hematuria risk score in this female cohort.
Results
A total of 2,705,696 urinalyses were performed in women during the study period, of which 552,119 revealed microscopic hematuria. Of these, 14,539 women were referred for urologic evaluation; clinical data for 3573 women were entered into the database. The overall rate of urologic cancer was 1.3% (47/3573). In women <60 years old, the rate of urologic cancer was 0.6% (13/2053) compared with 2.2% (34/1520) in women ≥60 years old ( P <.01). In women who reported a history of gross hematuria, the rate of urologic cancer was 5.8% (20/346) compared with a 0.8% (27/3227) in women with no history of gross hematuria ( P <.01). In multivariate analysis, > 60 years old (odds ratio, 3.1; 95% confidence interval, 1.6–5.9), a history of smoking (odds ratio, 3.2; 95% confidence interval, 1.8–5.9), and a history of gross hematuria in the previous 6 months (odds ratio, 6.2; 95% confidence interval, 3.4–11.5) were associated with urologic cancers. A higher microscopic hematuria risk score was associated with an increased risk of cancer in this test cohort ( P <.01). Women in the highest risk group had a urologic cancer rate of 10.8% compared with a rate of 0.5% in the lowest risk group.
Conclusions
In this female population, >60 years old and a history of smoking and/or gross hematuria were the strongest predictors of urologic cancer. Absent these risk factors, the rate of urologic cancer did not exceed 0.6%. A higher hematuria risk score correlated significantly with the risk of urologic cancer in this female test cohort.
M icroscopic hematuria (MH) is defined by the American Urologic Association (AUA) as ≥3 red blood cells (rbc) per high-power field (hpf) on a properly collected urinary specimen in the absence of an obvious benign cause. Because MH has been associated with underlying urologic cancer, the AUA recommends evaluation with cystoscopy and upper tract imaging, preferably with computer tomography (CT) scan, for all patients >35 years of age with this finding. This evaluation can be associated with discomfort, urinary tract infection, radiation exposure, and increased cost to the healthcare system. Additionally, adherence to these recommendations, particularly by primary care providers, is low.
Although MH is common, the overall prevalence of urologic cancers in the general population is low (0.1-3%), particularly in women, whose risk of bladder cancer is 3- to 4-fold lower, and risk of renal cancer is 2-fold lower, compared with men. In patients with MH at Kaiser Permanente Southern California (KPSC), the overall rate of urologic cancer was 0.7%. In women, the urologic cancer rate exceeded 1% only in patients >40 years and with >100 rbc/hpf. Despite the low overall prevalence of urologic cancer and its sex disparity, the AUA guidelines for the evaluation of MH are not sex specific . The prevalence of MH may be higher in women because of benign conditions; therefore, universal evaluation may not be appropriate for women, as recently highlighted by Harmanli and Yuksel.
We previously described a hematuria risk score that derived from a model of risk factors for urologic cancer. In this model, 4 points were given for age >50 years and/or history of gross hematuria, and 1 point was given for smoking, male sex, and/or >25 rbc/hpf (maximum score, 11). Patients were stratified into low (score, 0-4), moderate (score, 5-8) and high-risk (score, 9-11) groups in an attempt to further inform and promote adherence to hematuria guidelines within KPSC.
Given the low prevalence of urologic cancer in women and possible unintended consequences as a result of diagnostic evaluation, our primary aim was to further delineate risk factors for urologic cancer specific to women with MH. Our secondary aim was to evaluate the applicability of the hematuria risk score for women in this test cohort. We hypothesized that the risk of urologic cancer would be highest among older women, smokers, and women with a history of gross hematuria and that a previously validated hematuria risk score would be an accurate model for the prediction of urologic cancer risk in women.
Methods
We conducted an Institutional Review Board approved cohort study using data that were abstracted from the electronic medical record within KPSC from January 1, 2009, to June 30, 2015. KPSC is an integrated healthcare delivery system that provides care for >4 million members. Members obtain all healthcare, with rare exception, within this system.
We collected data on the total number of urinalyses that were performed, the number of those with MH on urine microscopy, and the number of women referred for its evaluation. Hematuria was identified by querying urine microscopy findings within the electronic health record and recording the RBC per HPF on urine microscopy. Referrals to the Urology Department for hematuria were obtained from the electronic health record with the use of ICD-9 codes 599.70-2. Patient data were evaluated according to a protocol that was derived from the AUA best practice recommendations. A prospective database was used to record clinical and demographic variables of patients who had undergone evaluation for MH. Patients who were >18 years old were eligible for entry into the database. Urologist participation was voluntary; therefore, the database is a convenience sample of patients who had been referred for evaluation of MH. Data on this cohort through 2011 have been published previously. The current cohort includes women from the original data set and additional patients through June 30, 2015.
Clinical and demographic variables that included age, race/ethnicity, and smoking history were abstracted from the electronic health record. Urologists (n=139/300) who participated in the voluntary database entered additional patient risk factors that included (1) history of gross hematuria within the past 6 months, (2) urinary tract imaging results, (3) cystoscopy findings, and (4) cause of hematuria, if determined. Urinalyses were categorized according to degree of hematuria: 0–3, 4–10, 11–25, 26–50 and >50 rbc/hpf.
To ensure accurate and complete capture of all urologic cancers, we used 3 methods. For the purposes of the study, we defined urologic cancer as cancer that involved the bladder, ureters, and/or kidneys. The initial list of patients with urologic cancer was obtained from the clinical database. The medical record numbers of all patients with urologic cancer were then cross-referenced with the KPSC cancer registry, which is a comprehensive list of all patients who were diagnosed with cancer and available through June 2015. Cohort patients were followed for up to a year through the cancer registry. The overall prevalence of urologic cancer in women within KPSC was calculated to ensure that the prevalence in our cohort accurately represented the prevalence in the larger population. Finally, chart review was performed to confirm a pathologic cancer diagnosis for each case.
Given our primary aim to delineate risk factors for urologic cancer in women with MH, the present analyses were stratified by gender. Rates of urologic cancer in men are provided for the purpose of comparison only. Cohort characteristics were described with the use of percentages. Bivariate associations were evaluated with the use of the chi-square test and logistic regression models. Risk ratios of urologic cancer were estimated with the use of multivariate regression analysis.
We evaluated the applicability of the previously defined hematuria risk score to this female cohort. For statistical analyses, patients were stratified according to the previously described risk score into low- (score, 0–4), moderate- (score, 5–8), and high-risk (score, 9–10) groups. We then evaluated the risk score separately for bladder and renal cancer in women. Patients were further stratified by age, history of gross hematuria, and positive (>3 rbc/hpf) or negative (0-3 rbc/hpf) microscopy. Probability values of <.05 were considered statistically significant. Data analysis was performed with SAS software (version 9.3; SAS Institute Inc, Cary, NC).
Results
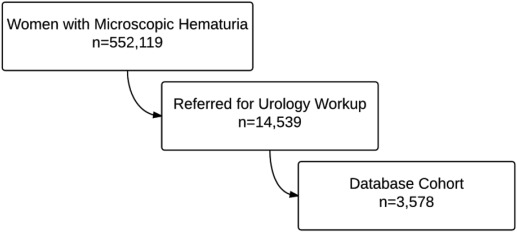
From January 1, 2009, to June 30, 2015, 3,742,348 urinalyses were performed on 2,705,696 women, 552,119 of whom (20%) had >3 rbc/hpf; this number includes those patients with an identified benign cause of MH, such as urinary tract infection, who were not referred for further evaluation. Of the women with MH, 14,539 women (2.6%) were referred for urologic evaluation, and 3573 women (25%) had data entered into the database and were included in the study ( Figure ). In this study cohort, urolithiasis was cited as the cause of MH in 24%, of urinary tract infection in 2%, and urologic cancer in 1% (n=34). Most women (74%) did not have an identified cause of their MH.
The demographic and clinical characteristics of the women in the cohort are presented in Table 1 . Most of the women were white or Hispanic, >50 years of age, and nonsmokers and had 4–24 rbc/hpf on urine microscopy. There were 693 women, 19.5% of the cohort, whose data were entered into the database with 0–3 rbc/hpf on microscopy. The rate of urologic cancer in the study cohort of was 1.3% (47/3573 women; Table 2 ). In univariate analysis, risk factors that were associated with cancer were increasing age, history of gross hematuria in the previous 6 months, degree of MH on microscopy, and current or previous smoking (all P <.05; Table 3 ).
| Variable | Total (n=3573), n (%) | No cancer (n=3526), n (%) | Cancer (n=47), (%) | P value | Bladder (n=34), n (%) | Renal (n=10), n (%) | Ureteral (n=3), n (%) |
|---|---|---|---|---|---|---|---|
| Age, y | <.001 | ||||||
| <40 | 436 (12.2) | 435 (99.8) | 1 (0.2) | 1 (0.2) | 0 | 0 | |
| 40-59 | 1617 (45.2) | 1605 (99.3) | 12 (0.7) | 6 (0.4) | 6 (0.4) | 0 | |
| ≥60 | 1520 (42.6) | 1486 (97.8) | 34 (2.2) | 27 (1.8) | 4 (0.3) | 3 (0.2) | |
| Race | .003 | ||||||
| White | 1413 (39.6) | 1384 (97.9) | 29 (2.1) | 20 (1.4) | 7 (0.5) | 2 (0.1) | |
| Latina | 1046 (29.3) | 1041 (99.5) | 5 (0.5) | 2 (0.2) | 2 (0.2) | 1 (0.1) | |
| Other | 1114 (31.1) | 1101 (98.8) | 13 (1.2) | 12 (1.1) | 1 (0.1) | 0 | |
| Smoking status | <.001 | ||||||
| Never | 2120 (59.3) | 2101 (99.1) | 19 (0.9) | 11 (0.5) | 8 (0.4) | 0 | |
| Current/former | 933 (26.1) | 907 (97.2) | 26 (2.8) | 21 (2.3) | 2 (0.2) | 3 (0.3) | |
| Passive/unknown | 520 (14.6) | 518 (99.6) | 2 (0.4) | 2 (0.4) | 0 | 0 | |
| Degree of hematuria, (rbc/hpf) | .003 | ||||||
| 0-3 | 693 (19.5) | 686 (99.0) | 7 (1.0) | 3 (0.2) | 3 (0.4) | 1 (0.1) | |
| 4-25 | 1887 (52.7) | 1870 (99.1) | 17 (0.9) | 13 (0.7) | 4 (0.2) | 0 | |
| ≥25 | 812 (22.7) | 792 (97.5) | 20 (2.5) | 16 (2.0) | 2 (0.2) | 2 (0.2) | |
| Unknown | 181 (5.1) | 178 (98.3) | 3 (1.7) | 2 (1.1) | 1 (0.1) | 0 | |
| History of gross hematuria | <.001 | ||||||
| No | 3227 (90.4) | 3200 (99.2) | 27 (0.8) | 20 (0.6) | 7 (0.2) | 0 | |
| Yes | 346 (9.6) | 326 (94.2) | 20 (5.8) | 14 (4.0) | 3 (0.9) | 3 (0.9) |
a Based on agreement of urology chiefs within Kaiser Permanente, hematuria was defined as greater than 3 rbc/hpf; however, all patients whose data were entered into the database were included for analysis.
| Variable | Female (n=3573), n (%) | Male (n=2966), n (%) | P value |
|---|---|---|---|
| All urologic cancer | 47 (1.3) | 172 (5.8) | <.01 |
| Renal | 10 (0.3) | 31 (1.1) | .03 |
| Bladder | 34 (1.0) | 140 (4.7) | <.01 |
| Ureteral | 3 (0.1) | 1 (0.03) | .13 |
| Age <60 y a | |||
| All urologic cancer | 13 (0.6) | 38 (2.5) | <.01 |
| Renal | 6 (0.3) | 12 (0.8) | .03 |
| Bladder | 7 (0.3) | 26 (1.7) | <.01 |
| Ureteral | 0 | 0 | 1.0 |
| Age ≥60 b | |||
| All urologic cancer | 34 (2.2) | 134 (9.1) | <.01 |
| Renal | 4 (0.3) | 19 (1.3) | <.01 |
| Bladder | 27 (1.8) | 114 (7.7) | <.01 |
| Ureteral | 3 (0.2) | 1 (0.1) | .37 |
| Factors associated with urologic cancer in women a | Odds ratio (95% confidence interval) | |
|---|---|---|
| Unadjusted (n=3578) | Adjusted (n=3578) | |
| Age ≥ 60 y | 3.6 (1.9–6.8) | 3.1 (1.6–5.9) |
| History of smoking | 3.4 (1.9–6.1) | 3.2 (1.8–5.9) |
| Microscopic hematuria >25 rbc/hpf | 2.0 (1.1–3.6) | 1.8 (0.9–3.2) |
| Gross hematuria | 7.2 (4.0–13.1) | 6.2 (3.4–11.5) |
a Variables included in the model: age, history of smoking, degree of hematuria, report of gross hematuria.
When stratifying patients by age, we evaluated the previous cutoff of 50 years and found age ≥60 years to be a stronger predictor of cancer in the female cohort, with the area under the ROC receiver operating characteristic curve in bivariate analysis increasing from 0.59–0.65. In women who were <60 years old, the rate of urologic cancer was 0.6% (13/2053) compared with 2.2% (34/1520) in women ≥60 years (p<0.01). The rate of renal cancer was 0.3% (6/2,053) in women who were <60 years old and 0.3% (4/1520) in women who were ≥60 years old ( P =.87). In women who were <60 years old, the rate of bladder cancer was 0.3% (7/2053) compared with 1.8% (27/1520) in women who were ≥60 years old ( P <.01). In women who were <40 years old, there were no renal cancers and 1 bladder cancer, which yielded an overall urologic cancer rate of 0.2% (1/436; Table 1 ).
We further stratified the analyses by patient report of gross hematuria. In patients with gross hematuria, the rate of cancer was 1.6% (2/129) in those with negative microscopy (0–3 rbc/hpf) and 8.3% (18/217) in those with positive microscopy (>3 rbc/hpf; P =.01). In women without gross hematuria, the rate of cancer was 1.1% (8/745) in those with negative microscopy and 0.8% (19/2482) in those with positive microscopy ( P =.42; Table 4 ). The positive predictive value of positive MH with a history of gross hematuria is 0.08 (18/217 women). In women with MH without a history of gross hematuria, the positive predictive value is 0.008 (19/2482 women).



