Fig. 20.1
Ligation and section of the superior sigmoid arteries, conservation of the inferior sigmoid artery, and the Riolan arcade
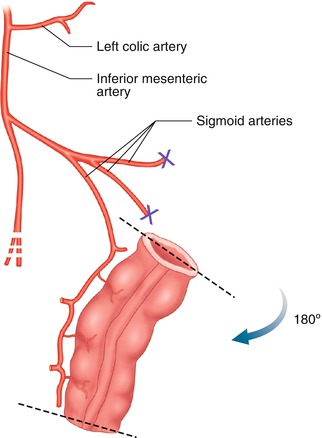
Fig. 20.2
Rotating the graft 180° for a colovestibular anastomosis without tension
Step Three: Colovestibular Anastomosis
A U–shaped incision is made in the vaginal stump laparoscopically, to protect the urethra and to provide a flap large enough to allow for colovestibular anastomosis (Fig 20.3). The sigmoid graft is turned 180°. The colovestibular anastomosis is performed through the perineal route with Vicryl 3-0 sutures, after the staples are removed.
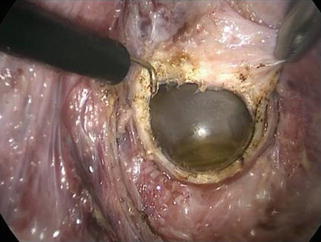
Fig. 20.3
A U-shaped incision is made in the vaginal stump laparoscopically
Step Four: Graft Sacropexy
To prevent a prolapse of the sigmoid transplant, the end of the neovagina is fixed to the sacral promontory with two nonresorbable stitches, and the laparoscopy is completed.
Step Five: Assessment of Anatomical and Functional Results
Anatomical results are assessed by a first clinical examination under general anesthesia 1 month after surgery. We use Hegar dilatators (n° 28–32) to assess wound healing and vaginal patency.
Afterwards, the patient must practice dilatation of the graft until she begins sexual activity.
Complications
Immediate Complications
Two women developed a major complication: a pelvic hematoma due to bleeding in the perineal cleavage. It required surgical re-exploration and hemostasis.
Rectal injury occurred in two patients during the perineal route. The wound was detected immediately and sutured without any further complication. Four complications resulted from using the peritoneal route for cleavage.
Later Complications
Anatomical results of sigmoid vaginoplasty were good. Shrinkage of the graft remains the primary complication (17 %). It is, however, easy to repair with a dilatator. Prolapse of the neovagina occurred in 4 % of the patients in our series and has been described by other authors [15, 16]. We have had no such cases since making the sacropexy a systematic part of the procedure.
Excessive mucus production has been reported [17, 18]. It can be reduced by choosing a short graft and by vaginal douching. Colitis of the bowel graft has also been described [17, 18], and, in one cases, mucinovs adenocarcinoma [17, 18]. We had one such case in our series, 11 years after the graft. The graft has been removed, but hepatic metastases have developed.
In the case of persistent bleeding, an endoscopy and biopsies of the graft must be considered.
Functional Results and Sexual Function
Materials and Methods
In 2010, a questionnaire analyzing sexual function was sent to the women included in our series since 1992.
Two standardized questionnaires were used: the Female Sexual Function Index (FSFI©) [19] and the Female Sexual Distress Scale – Revised (FSDS-R©) [20, 21]. These questionnaires were addressed to 11 women for whom vaginal dilatation was recommended and to 48 who had had a sigmoid vaginoplasty.
Rosen’s FSFI included 19 items analyzing 6 separate domains of the functional aspect of female sexuality: desire, arousability, orgasm, lubrication, comfort, and quality of sexual life. The total FSFI score, which had a maximum of 36, was obtained by summing the six domain scores. Patients with a total score ≤26.55 were defined with sexual dysfunction [19]. The next 13 questions of the questionnaire came from the FSDS-R (Female Sexual Distress Scale-Revised) [20, 21] and assessed psychological distress in women with hypoactive sexual desire disorder, as described by Derogatis. A score above 11 (maximum: 52) suggested sexual distress.
We included 12 additional questions concerning details on sexual intercourse, vaginal discharge, pelvic pain, self-esteem, depression, and gestational surrogacy.
Functional Results
The women’s mean age at the time they completed the questionnaire was 24 years, and the mean time after surgery was 6 years (range: 10 months–17.8 years).
In all, 40 (68 %) women responded to the questionnaire: 35 (73 %) of the 48 who had surgery and 5 (45 %) of the 11 treated by vaginal dilatation. Six (10 %) were lost to follow-up and 13 (22 %) did not return the questionnaire. One wrote to state that the subject was too intimate to be discussed in a mail questionnaire.
Table 20.1 shows the FSFI and FSDS-R scores.
Table 20.1
Functional results (FSFI and FSDS-R scores) of women treated by sigmoid vaginoplasty or Frank method
Procedure | No. of patients | No. of responses | FSFI© | FSDS-R® | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
Desire | Arousability | Lubrication | Orgasm | Satisfaction | Comfort | Total score | ||||
Sigmoid vaginoplasty | 48 | 35 (73 %) | 4.36 | 4.74 | 5.18 | 4.44 | 5.35 | 3.93 | 28.00 | 21.35 |
±0.9 | ±0.7 | ±0.9 | ±1.1 | ±0.6 | ±1.2 | ±3.1 | ±12.2 | |||
Franks method | 11 | 5 (45 %) | 4.65 | 5.10 | 5.10 | 4.80 | 5.40 | 5.20 | 30.25 | 18.40 |
±1.3 | ±1.0 | ±1.1 | ±0.9 | ±1.2 | ±1.1 | ±6.2 | ±15.4 | |||
Total | 59 | 40 (68 %) | – | – | – | – | – | – | – | – |
p (Wilcoxon exact Test) | – | – | 0.64 | 0.34 | 0.93 | 0.61 | 0.57 | 0.06 | 0.13 | 0.72 |
Table 20.2 summarizes responses to the additional questions concerning intercourse frequency, vaginal discharge, pelvic pain, self-esteem, depression, and surrogacy.
Table 20.2
Answers to additional questions concerning intercourse frequency, vaginal discharge, pelvic pain, self-esteem, depression, and surrogacy
Questions | Sigmoid vaginoplasty | Frank method | All patients | p | |
|---|---|---|---|---|---|
Mean time before first intercourse after treatment (in months) | 7 | 5 | – | 0.54 | |
Frequency of vaginal intercourse | Occasionally | 8 (27 %) | 1 (25 %) | – | – |
1–2/week | 12(40 %) | 0 | – | – | |
2–3/week | 7 (23 %) | 2 (50 %) | – | – | |
Daily | 3 (10 %) | 1 (25 %) | – | – | |
Vaginal discharge discomfort | 23 (68 %) | 0 | – | – | |
Abdominal pain
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||