Neonatal Hypotonia
HISTORICAL PERSPECTIVE
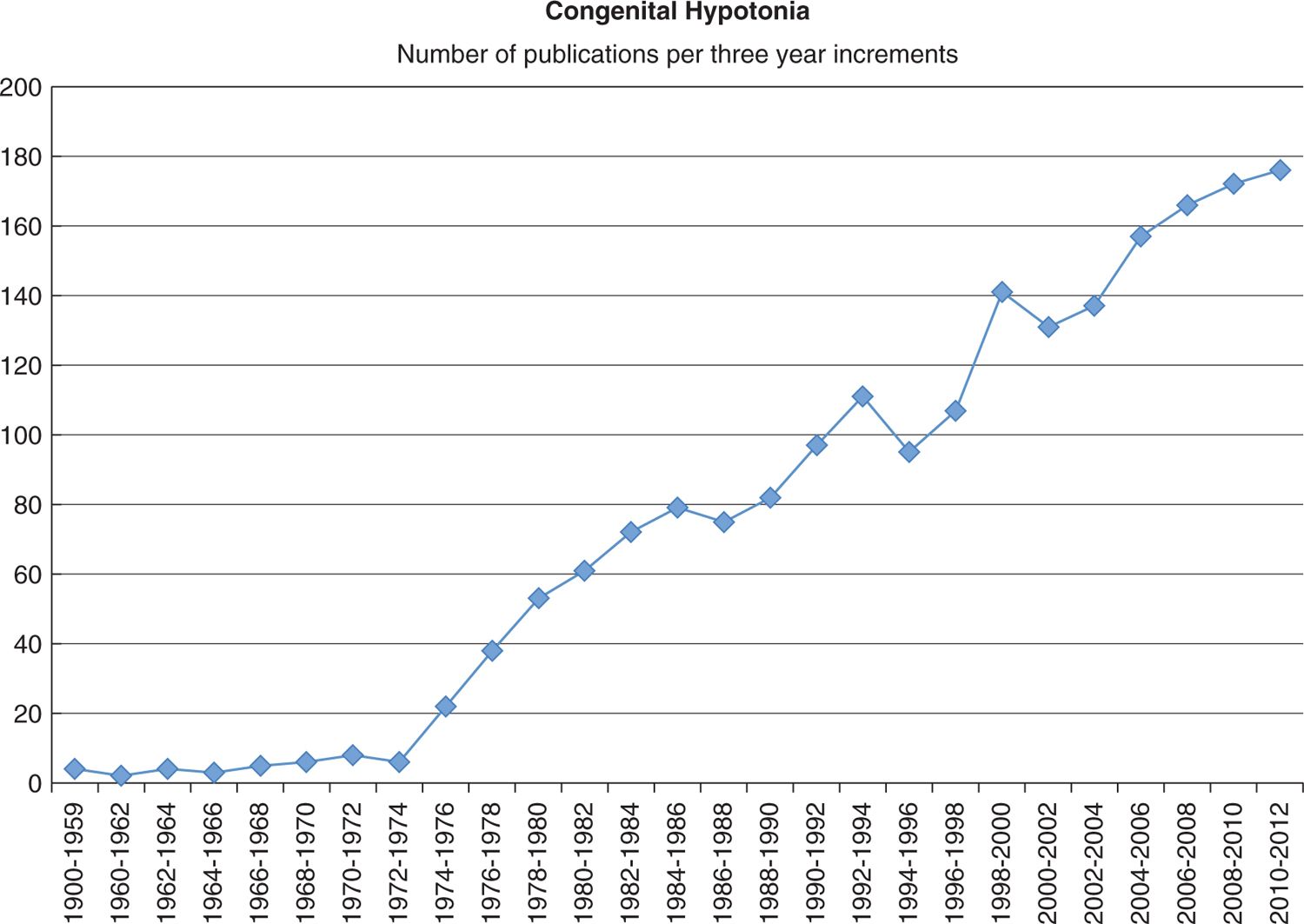
It is difficult to find any reference to neonatal hypotonia before the beginning of the 20th century. This may be in part related to the very high infant mortality rate and the fact that for most of history children were not considered of much value until they had reached the age of 7 or so, when they had survived the vicissitudes of childhood and could start working.1 With the advent of the Industrial Revolution and the fundamental changes in medicine that accompanied it, the first reports of infantile hypotonia were published (for an excellent summary of this history, refer to Victor Dubowitz’s seminal work on the floppy infant2). Since the 1970s, and likely as a result of the exponential improvements in diagnostic tools, the scientific publications dedicated to hypotonia have steadily accumulated (Figure 17-1).
FIGURE 17-1 Scientific publications dedicated to congenital hypotonia have steadily increased since 1972–1974.
The earliest reports2 of congenital hypotonia are probably those by Werdnig in 1891 and Hoffman in 1893. They independently described infants, apparently healthy at birth, who subsequently developed hypotonia and respiratory failure. Both of these authors described the pathology associated with spinal muscular atrophy (SMA). In 1900, Oppenheim described a series of infants born hypotonic and hyporeflexic who subsequently appeared to improve with no obvious residual pathology. He suggested the term myatonia congenita, later renamed amyotonia congenita. In 1957, Walton suggested the term benign congenital hypotonia to refer to cases in which the prognosis was “mild and may be overcome in time.”3 His major point was to distinguish patients with a grim prognosis, as is the case in SMA, from those who faired better. Although the choice of the term benign was an unfortunate one that has led to considerable confusion, the diagnostic challenge that he was facing is still the dilemma that faces today’s clinician. That is, what is the pathology behind the apparent hypotonia, and perhaps more importantly, what is the prognosis? The object of this chapter is to offer a rational approach to the diagnostic workup of the hypotonic infant.
DEFINITION: HYPOTONIA VS WEAKNESS
The first and perhaps most important step in evaluating a hypotonic infant is to ask the question: Is the infant truly hypotonic, or does the perceived hypotonia reflect weakness? The difference can be subtle but is of the essence since this difference is the first step in elucidating the etiology of the observed phenotype. Tone is generally defined as resistance to passive movement.4 Tone can be further divided into postural or truncal tone (proximal muscle groups) and phasic or peripheral tone (extremities). In contrast, weakness refers to lack of muscle strength.5 Therefore, in its simplest terms, strength can be thought of as the ability to generate movement and tone the ability to generate posture. It follows that weakness is the inability to maintain movement while hypotonia is the inability to generate posture. Thus, a 1-year-old child with a history of hypoxic ischemic encephalopathy (HIE) will likely demonstrate truncal hypotonia, peripheral spastic hypertonia, and diffuse weakness. This introduces one last concept that needs to be defined: spasticity. Spasticity is generally defined as velocity-dependent increase in tone. In other words, tone increases with increased speed of movement about a joint.
EPIDEMIOLOGY
There are no studies that have looked at the incidence or prevalence of neonatal hypotonia. This likely reflects the broad range of etiologies associated with congenital hypotonia as well as the challenges associated with objectively defining hypotonia. However, by gleaning information from papers reporting the incidence of specific etiologies of neonatal hypotonia, one can estimate the overall incidence. There seems to be a consensus that HIE and intracranial hemorrhage account for approximately one-third of all cases of hypotonia in term infants.6,7 In a retrospective chart review, Takenouchi et al reported the incidence and etiology of perinatal brain injury in term infants admitted to the New York Presbyterian Hospital neonatal intensive care unit (NICU).8 In their study, the reported incidence of HIE in term infants was 0.27 per 1000 births. Assuming that these numbers are representative of the larger population, one can then extrapolate the incidence of congenital hypotonia in term infants to be on the order of 0.8/1000 births. However, the incidence of “neonatal encephalopathy,” a global nonspecific term encompassing any congenital injury to the brain, is reported as 1 to 6 per 1000 live births. Since the most frequent presentation of neonatal encephalopathy is hypotonia,9 it is probable that the incidence of neonatal hypotonia is much higher than was extrapolated from the study mentioned above.
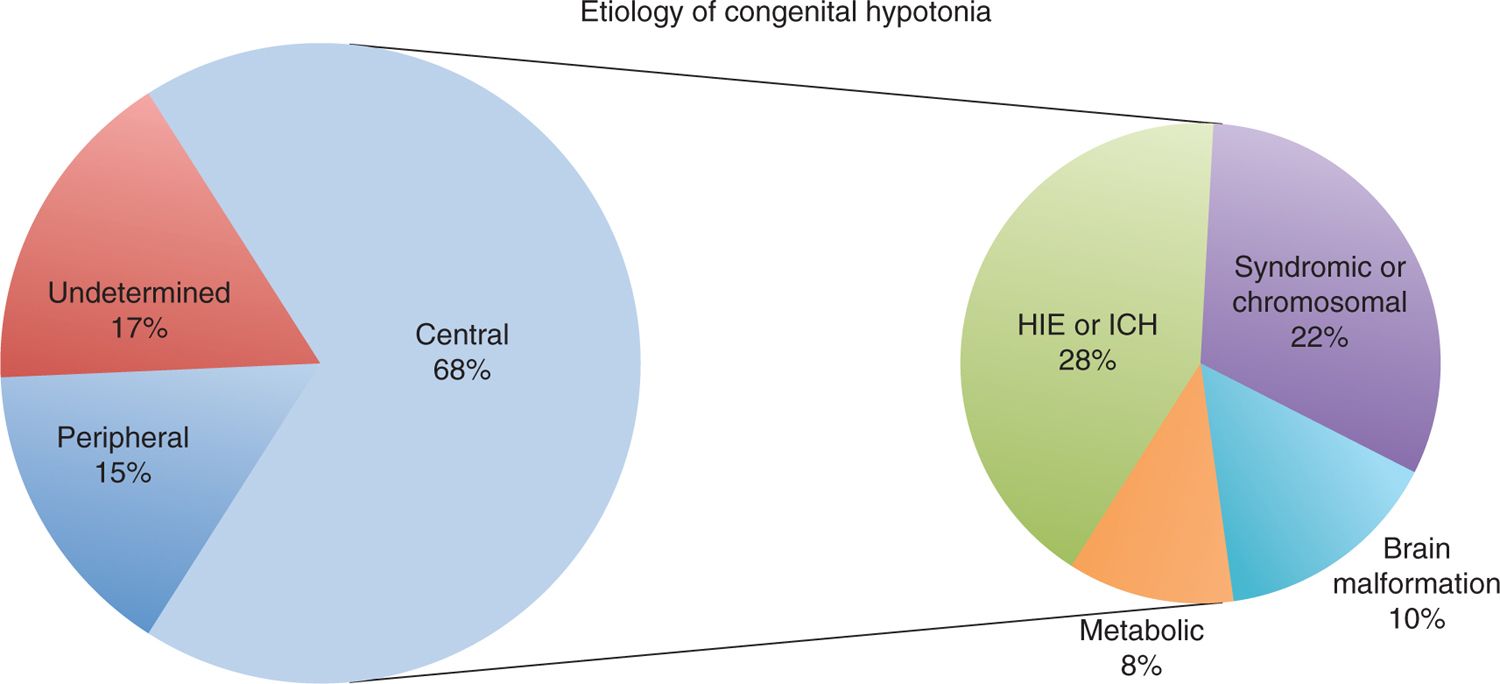
The etiology of neonatal hypotonia has been addressed in several retrospective studies.6,7,10,11 Most of these studies gave a similar distribution with regard to etiology (Figure 17-2). Typically, 66% to 88% of the hypotonia is classified as central, referring to causes in the central nervous system (CNS), while 9% to 34% is classified as peripheral, referring to causes in the peripheral nervous system, the neuromuscular junction, or the muscle itself. Of the central causes, HIE and intracerebral hemorrhage account for 28% to 42% of cases, chromosomal abnormalities and syndromic disorders (presumably chromosomal) account for 26% to 34% of cases, while the rest of the etiologies are spread among a wide variety of causes, ranging from migrational to metabolic disorders, each accounting for less than 10% of cases.
FIGURE 17-2 Etiology of congenital hypotonia among 144 infants. On the left is the percentage of congenital hypotonia due to central, peripheral, and undetermined causes. On the right is a further breakdown of the causes of central congenital hypotonia. HIE, hypoxic ischemic encephalopathy; ICH, intracranial hemorrhage. (Data from Laugel et al.11)
One retrospective study is unique in that it focused exclusively on causes of peripheral hypotonia.12 The purpose of this study was to evaluate whether classification of hypotonia as peripheral using standard physical examination parameters was an effective diagnostic approach to these infants. In this study, approximately 80% of the hypotonic infants had an identifiable disorder, and of those, 47% had a neuromuscular disorder. Interestingly, of the remaining 53% of infants, 10% had a genetic disorder, 10% a metabolic disorder, and 5% a CNS injury. Therefore, even after a careful clinical examination, more than a quarter of the infants were found to have evidence of CNS involvement (combining the genetic disorders, the metabolic disorders, and CNS injury). This illustrates well the conundrum clinicians face when evaluating the hypotonic infant: Even after a careful examination, hypotonia may appear peripheral in nature, yet the etiology will turn out to be central in many of the cases.
A SYSTEMATIC APPROACH TO CONGENITAL HYPOTONIA
So, how does one approach the hypotonic infant? Many different diagnostic approaches to the hypotonic infant have been proposed, starting with Walton in 1957, who classified the hypotonia into infantile muscular atrophy and related disorders, symptomatic hypotonia, and benign congenital hypotonia.13 In 1964, Rabe proposed a classification based on neuroanatomical location: CNS, spinal cord, spinal roots and peripheral nerves, myoneural junction, and muscle.14 Dubowitz, in his classic monograph on the floppy infant, argued for a classification of hypotonic infants in 2 groups: paralytic and nonparalytic.2 Dubowitz’s approach has the advantage of simplifying the initial evaluation of the hypotonic infant. In this system, the child is classified on the basis of his or her ability to generate any movement against gravity and to maintain posture. If either of these findings is present, the infant can be classified as belonging to the nonparalytic group, the vast majority of whom will have a CNS etiology for the hypotonia. A similar approach was advocated by Bodensteiner,4 who divided the hypotonic infants into (1) supraspinal conditions or central hypotonia and (2) segmental conditions or motor unit hypotonia. Both of these approaches have the merit of simplifying the initial evaluation of the hypotonic infant. However, additional clues that can help further delineate the etiology of the hypotonia can often be gleaned from the history and examination. In this chapter, we adopt a nomenclature similar to that proposed by Bodensteiner,4 dividing the hypotonia into central vs peripheral.
It is worth noting that the terminology has its limitations. For example, the spinal cord is part of the CNS. Yet, we (and many others) choose to group SMA (a disorder of the motor neurons as it originates in the ventral horn of the spinal cord) in the peripheral hypotonia group. This makes sense since it is the motor neuron, the first component of the neuromuscular unit, that is affected. One might argue that the “segmental” nomenclature suggested by Bodensteiner is more accurate. However, the terms central and peripheral are widely used and generally well accepted. Therefore, we keep this nomenclature.
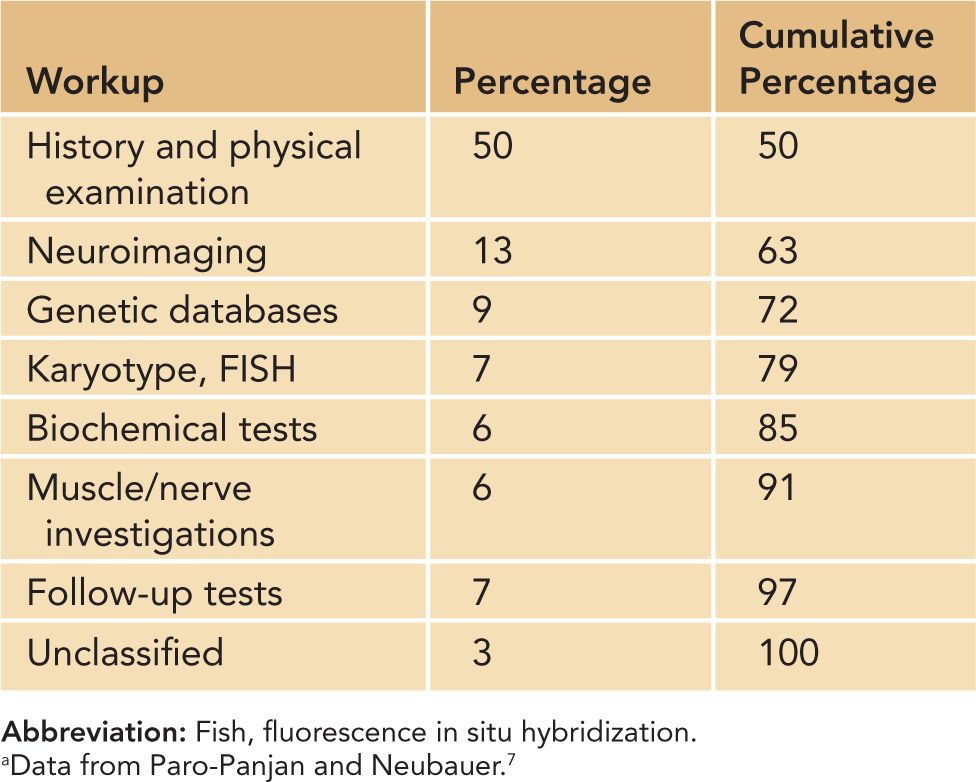
The following discussion reviews clues that can be uncovered from a careful history and physical examination. The importance of a good history and physical examination cannot be overstated. In a retrospective study of 138 hypotonic infants, Paro-Panjan and Neubauer7 found that 50% were properly classified on the basis of the history and physical examination alone, another 13% by neuroimaging, and the rest by other ancillary tests. None of the additional ancillary tests contributed to the classification of more than 10% of the study group7 (Table 17–1).
Table 17-1 Contribution of Various Aspects of evaluation to Diagnosis in Neonates With Congenital Hypotonia
Yet, the clues gleaned from the history and physical examination are often neither sensitive nor specific and should be framed within the larger clinical context, including ancillary tests. We believe that the best approach to the hypotonic infant is a staged approach. The initial classification into central vs peripheral hypotonia advocated by Dubowitz and many others is useful in establishing the initial diagnostic approach to the child. However, as further information becomes available, the differential diagnosis will evolve. The next section is written with this in mind. It reviews findings from the history, examination, and initial ancillary tests and how these might help narrow the wide spectrum of etiologies for congenital hypotonia.
History and Physical
It is essential to obtain a good history, as it will often uncover important clues regarding the diagnosis. The history should start with a careful history of the pregnancy. Was there poor prenatal care? Was there a history of alcohol or drug abuse? Was there a history of maternal illness during the pregnancy? A positive answer to any one of these questions markedly increases the risk for central hypotonia. This is in contrast to eliciting a history of decreased fetal movements, which is more frequently observed in peripheral hypotonia.11
A thorough family history is also important. In a retrospective review of 83 infants with hypotonia consistent with motor unit disorders, 50% of the infants who were the product of a consanguineous union had a metabolic disorder, while 20% of infants with a diagnosed condition had a positive family history of a similar condition.12
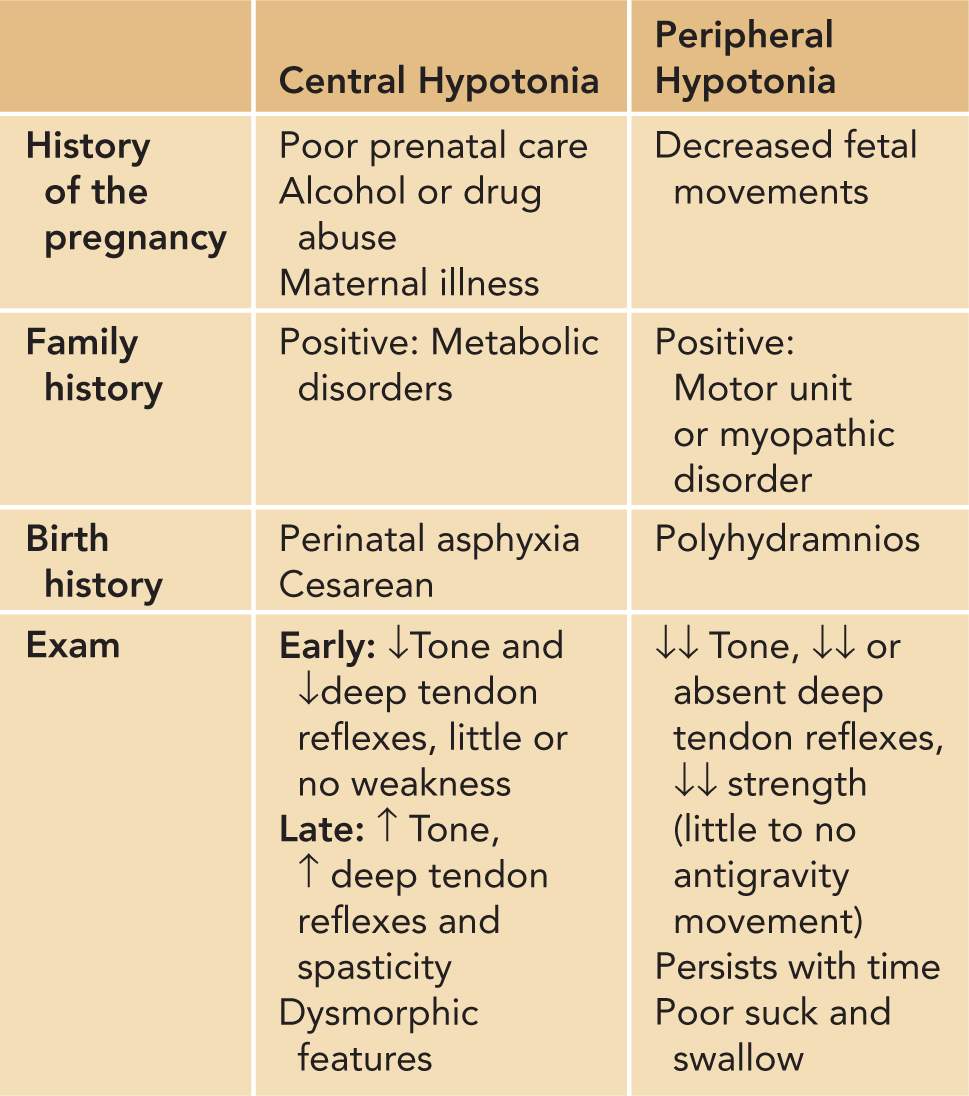
A detailed birth history is also essential. In a retrospective cohort study of 144 hypotonic infants, Laugel et al found that polyhydramnios was much more frequent in peripheral hypotonia, while delivery via cesarean section or a history of perinatal asphyxia was more frequently associated with central hypotonia.11 The contributions of the history and physical examination in distinguishing central from peripheral hypotonia are summarized in Table 17-2.
Table 17-2 Distinguishing Central From Peripheral Hypotonia by History and Physical Examination in Neonates Presenting With Congenital Hypotonia
Anatomical Localization
Cerebral Hypotonia
Central hypotonia can be divided in disorders caused by cerebral hypotonia and those caused by spinal cord dysfunction. Cerebral hypotonia, meaning hypotonia caused by abnormalities in the brain, has many etiologies, and it is unlikely that one can differentiate the causes of cerebral hypotonia based on examination alone. Nevertheless, some concepts may be useful when examining these infants. First and foremost, central hypotonia is usually not accompanied by weakness or hyporeflexia. If anything, in time the infant will display increased tone and reflexes, although initially, cerebral hypotonia may be easily confused as peripheral hypotonia, especially during the early phase of the illness, when there may be transient weakness and hyporeflexia.
When evaluating central hypotonia, it is useful to keep in mind the following broad categories of etiologies: systemic illness, genetic disorders, cortical dysgenesis and other malformations, deep-brain nuclei injury, brainstem and cerebellar dysfunction, and finally, spinal cord disruption. We return to each of these later in the chapter. The purpose of this section is to highlight common threads that may help with localization.
Systemic Illnesses
Systemic illnesses will often cause profound hypotonia from what can be thought of as an energy crisis imposed on the brain by the demands of the concurrent illnesses. These processes include sepsis and other infectious processes, congenital cardiac malformations, necrotizing enterocolitis, gastroschisis, and so on. Congenital metabolic disorders figure prominently in this group as well. Infants with such disorders will often appear normal at birth but will rapidly decompensate within the first 72 hours of life.
Genetic Disorders
Perhaps the most useful finding in identifying genetic disorders as a cause of cerebral hypotonia is the presence of dysmorphic features. Evidence for holoprosencephaly can be obvious (cyclopia) or much less obvious (single central incisor). If such abnormalities are found, it is important to look for other midline abnormalities, such as cleft lip or palate and congenital heart malformations. The presence of up- or down-slanting palpebral fissures, hypertelorism, or prominent bilateral epicanthal folds are often good indicators of a genetic disorder.
Cortical Dysgenesis and Other Malformations
Further clues may help sort the anatomical location of the central hypotonia. The presence of seizures is highly consistent with cortical abnormalities of both acquired and developmental etiologies.
Deep-Brain Nuclei Injury
With injury to deep-brain nuclei, as is seen in severe hypoxia (putamen) or severe hyperbilirubinemia (globus pallidus [GP] and subthalamic nucleus), one often observes hypotonia rapidly followed by increased tone, often within a few days to a few weeks of the injury.9
Brainstem and Cerebellar Dysfunction
Severe hypoxia, as can be seen with catastrophic peripartum events, can cause brainstem injury. This will often be clinically evident by cranial nerve dysfunction and feeding difficulties and is associated with high neonatal mortality.9 Cerebellar and brainstem malformations are often associated with profound hypotonia. For example, infants with Joubert syndrome15 (vermian and midbrain atrophy with the “molar tooth sign” on magnetic resonance imaging [MRI] or pontocerebellar hypoplasia16 [cerebellar hemisphere and pontine hypoplasia]) almost always present with congenital hypotonia.
Spinal Cord Disruption
Spinal cord disruption may occur as a result of trauma at the time of delivery or, more commonly, of spinal cord dysraphism. Spinal cord injury as a result of trauma during delivery remains a relatively rare event. The prevalence was reported as 1 per 29,000 live births in 1 study.17 The injuries are felt to be the result of both traction and compression injuries, with most of the injuries occurring in the cervical spine. The infants present with flaccid tetraplegia or paraplegia depending on the level of the injury and in time develop spasticity. Due to the mechanics of the injury, cervical and high-level thoracic spine injuries are much more common than lower-level injuries. It is important to keep in mind that the withdrawal reflex is a spinal reflex; thus, the withdrawal reflex will be present in spinal cord injury. Spinal dysraphisms resulting in spinal cord disruption sufficiently severe to cause congenital hypotonia will generally be evident in that almost all of these will be open malformations, with the 2 most common being myelomeningocele and myelocele.18 As opposed to traumatic birth injury, spinal dysraphisms tend to be more common at the lower thoracic and lumbar levels.
Peripheral Hypotonia
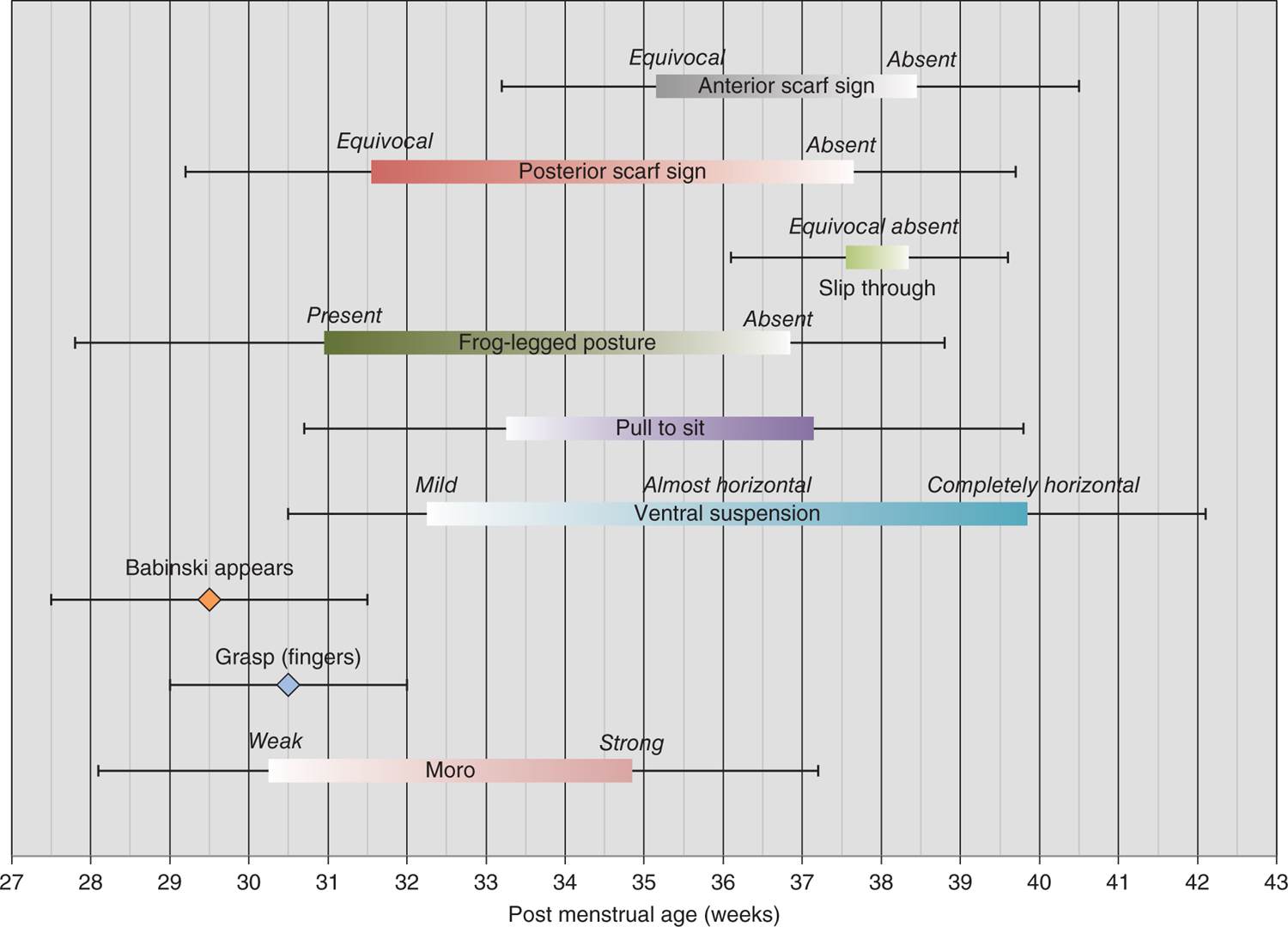
In contrast to cerebral hypotonia, peripheral hypotonia usually presents with profound weakness and an inability to maintain posture. This is often evident on examination by the classic “frog posture” or, as described by Dubowitz, the rag doll appearance of the infant.2 When lying prone on the examination table, these infants appear splayed out: the legs externally rotated, the arms inert parallel to the trunk, the shoulders falling backward. On horizontal suspension, the child will wrap around the hand of the examiner, while on vertical suspension the child will tend to slip due to the lack of tone in the shoulder girdle muscles. On traction of the upper extremities, the head will have a significant lag, and these infants often have a scarf sign, whereas on pulling 1 upper extremity across the chest the elbow will reach well beyond the midline. One consideration when examining the infant is the gestational age. As infants are delivered more and more prematurely, they have decreased tone that may be interpreted as pathogenic. In a longitudinal landmark study of 69 premature infants, Allen and Capute documented the average gestational age at which tone and reflexes develop19 (Figure 17-3). For example, all premature infants initially had a positive scarf sign and slip through on vertical suspension. It was not until 35 to 38 weeks’ gestational age that these signs remitted.
FIGURE 17-3 Neurological signs during development. The mean postmenstrual age of appearance of neurological signs relevant to muscle tone and strength are shown. The range of mean appearance or presence of each sign is shown as a thick, colored bar or a diamond, with the thin error bars before and after representing 1 standard deviation. (Data from Allen and Capute.19)
It is useful to divide peripheral hypotonia into its 3 functional units: the motor nerve unit, the neuromuscular junction, and the muscle itself. Some general comments can be made with regard to the clinical presentation of a dysfunction for each functional unit.
Motor Nerve Unit Dysfunction
The prototypic motor neuron unit disorder is SMA.20 In the neonatal form of this disorder, the α-motor neurons’ ability to survive is affected, resulting in a clinical picture consisting of profound hypotonia and absent deep-tendon reflexes. Although the neck muscles are weak, bulbar function is usually preserved, and the CNS is unaffected, resulting in infants with a normal level of alertness that often contrasts markedly to the observed profound hypotonia and weakness.
Neuromuscular Junction Dysfunction
While SMA presents with profound hypotonia but usually preserved bulbar function, congenital myasthenic syndromes, in addition to hypotonia, usually present with cranial nerve dysfunction, including ophthalmoparesis.21 Congenital myasthenias are frequently accompanied by fatigue, although this feature can be difficult to elicit in infants.
Muscle Dysfunction
Congenital muscle diseases include 2 broad categories based on their pathological appearance: the congenital myopathies22 and the congenital muscular dystrophies.23 These 2 categories encompass many disorders with phenotypes ranging the gamut from mild to severe. As a general rule, the muscular dystrophies present with markedly elevated serum creatine kinase (CK), while the congenital myopathies have normal-to-slightly-elevated CK levels. Most of these disorders, when present at birth, involve the bulbar muscles. Muscular dystrophies tend to affect more proximal muscles first.
ETIOLOGY OF HYPOTONIA BASED ON ANATOMICAL LOCALIZATION
In this section, we examine in more detail the most common etiologies of congenital hypotonia. Whereas the previous section described typical presentations by anatomical location, this section focuses on clinical presentations by etiology. It is important to keep in mind that we do not intend this section as a systematic review of each condition or intend to cover every possible etiology of congenital hypotonia. Either proposition is well beyond the scope of this chapter. Nevertheless, we offer a tool we hope can be used as a reference in the evaluation of the hypotonic infant, a tool that will cover the most common causes of hypotonia and will offer a good start in the evaluation of the more unusual disorders.
As described previously, a careful history and physical examination should allow the clinician to classify the hypotonia as central vs peripheral and it is hoped further localize the pathology. Based on this information, the clinician can now proceed to further refine the differential diagnosis. This section is designed to help in this second step. It is divided in etiologies by localization: systemic, cerebral, spinal cord, motor nerve unit, and finally muscle.
Systemic Hypotonia
Systemic hypotonia defines a group of disorders in which a systemic disorder, either directly or indirectly, has an impact on cerebral function with a resultant clinical hypotonia. Systemic hypotonias can be subdivided in 3 groups: acquired or congenital systemic illnesses indirectly causing a cerebral energy crisis, congenital metabolic syndromes, and acquired metabolic illnesses.
Acute Congenital or Acquired Illnesses Resulting in a Cerebral Energy Crisis
It is well established that hypotonia is a common presentation of systemic illnesses in the newborn. Although the pathophysiology of the hypotonia is not well defined, it is useful to think of it in the context of a cerebral energy crisis. In other words, the metabolic demand on the rest of the body is such that the brain enters a deficient state with resultant encephalopathy and hypotonia. Two good examples of systemic acquired and congenital illnesses with hypotonia as one of the prominent features are septicemia and congenital heart defects. In a retrospective study of 83 newborn infants with septicemia,24 only 6% of the infants had evidence of hypotonia before the onset of the infection, while the numbers rose to 54% at onset and 91% at the peak of the illness. In fact, it was one of the most consistent findings in septic infants (along with skin color and microcirculation). A similar result was reported in a study of infants with congenital heart defects.25 In this study, 28 of 50 patients examined demonstrated abnormalities on neurological examination, and 20 of these 28 presented with diffuse hypotonia and 5 with weakness in the upper extremities. Most of the time, these illnesses will be evident from the clinical context. However, occasionally hypotonia will be the first clinical clue that the child is ill and the etiology should be investigated aggressively.
Congenital Metabolic Syndromes
As a group, congenital metabolic syndromes are daunting to the clinician. They are relatively rare, they often have complicated metabolic pathways, and their clinical presentations vary widely even within a single disorder due to variable residual activity of the enzymes affected. Saudubray et al presented a useful approach to inherited metabolic disorders.26 They suggested classifying the disorders in 3 groups: disorders that give rise to intoxication, disorders of energy metabolism, and disorders involving complex molecules (Table 17-3). This classification has the merit of grouping the metabolic disorders in 3 groups with roughly distinguishable clinical presentations and with very different clinical managements. While the disorders that give rise to intoxication are mostly amenable to intervention, often urgently, the disorders in the other 2 groups are, as a general rule, poorly or not at all responsive to treatment.
Table 17-3 Metabolic Disorders Presenting With Congenital Hypotonia
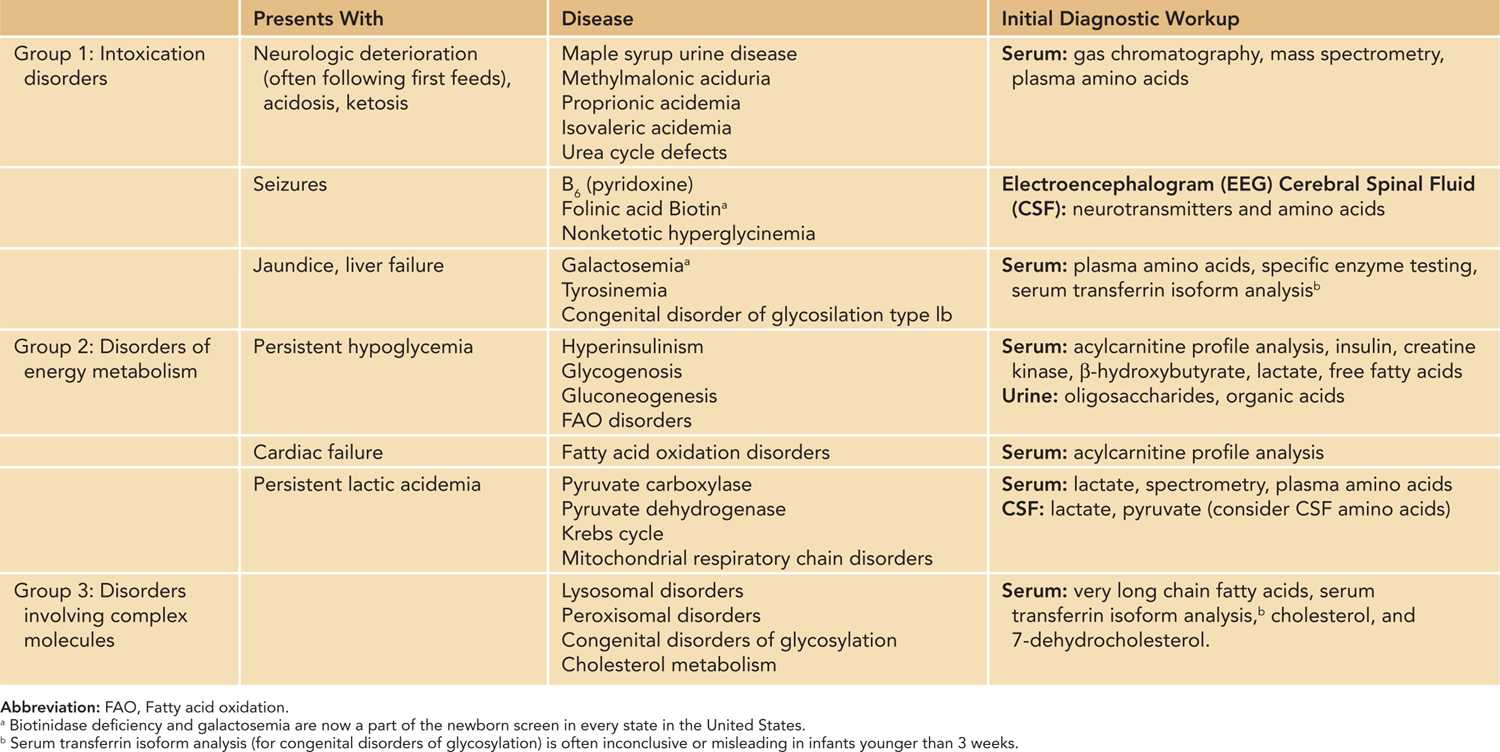
Disorders that give rise to intoxication: This group of disorders includes the aminoacidemias, organic acidurias, abnormalities of galactose and fructose metabolism, and congenital urea cycle defects. Infants with these disorders typically present with progressive deterioration over the first week of life, often with onset of symptoms following the first feeding. Many of these disorders are treatable and require early intervention.
Disorders of energy metabolism: These disorders include the glycogen storage diseases (glucose deficiency), fatty acid oxidation disorders (carnitine metabolism defects; small-, medium-, and long-chain acyl-coenzyme A deficiency) and congenital lactic acidemias (pyruvate metabolism disorders, Krebs cycle and mitochondrial disorders). This group of disorders typically presents with severe hypoglycemia, hyperlactic acidemia, hypotonia, organomegaly, and myopathy. While the congenital lactic acidemias are not amenable to treatment, the rest of these disorders respond at least partially to clinical intervention. Mitochondrial myopathies presenting in the neonatal period are rare and are briefly discussed in a separate section.
Disorders involving complex molecules: This group of disorders includes all of the lysosomal storage disorders, peroxisomal disorders, congenital disorders of glycosylation, and inborn errors of cholesterol synthesis (see Table 17-3). With few exceptions, none of these disorders are treatable.
Acquired Metabolic Illnesses
A number of entities can be classified in this group of acquired metabolic illnesses. They all present with neonatal hypotonia as a prominent feature. By definition, they are transient and acquired and caused by toxicity transmitted to the infant by the mother. Examples of such illnesses include lithium toxicity,27 magnesium toxicity,28 and transient neonatal myasthenia.29
Lithium toxicity: Prenatal exposure to lithium used to treat maternal bipolar illness may pose an increased risk of teratogenesis. Infants without malformations may have transiently depressed neurological function, including hypotonia, respiratory distress syndrome, cyanosis, lethargy, weak suck and Moro, apnea, and bradycardia.27 Lithium crosses the placenta freely, but the half-life in the fetus is increased. Most of these symptoms resolve as lithium is excreted, which may take up to 14 days. Transient nephrogenic diabetes insipidus, cardiac disorders, and thyroid goiters have been reported as well as cardiac anomalies, especially the Ebstein anomaly.
Magnesium toxicity: Magnesium sulfate is the most commonly used tocolytic and is now used for prevention of cerebral palsy.30 In a recent retrospective cohort analysis, 6% of infants born to 6654 women with preeclampsia treated with intravenous magnesium sulfate were diagnosed with hypotonia.28 Other clinical findings included significantly lower 1-minute Apgar scores and Apgar scores of 3 or less at 1 and 5 minutes. The probability of hypotonia increased with increasing magnesium concentration (13% when maternal magnesium levels were 7 mEq/L or greater).
Transient neonatal myasthenia: Transient neonatal myasthenia is a rare complication occurring in infants of mothers with acquired myasthenia gravis.29 The pathophysiology is felt to be secondary to passive transfer of maternal acetylcholine receptor (AChR) antibodies across the placental blood barrier. However, this mechanism is clearly not sufficient since all infants born to mothers with positive AChR antibody myasthenia are found to have elevated AChR titer, yet only a small proportion develop symptoms. In a retrospective cohort study of 127 births to mothers with acquired myasthenia, 5 (4%) infants were diagnosed with neonatal myasthenia.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree