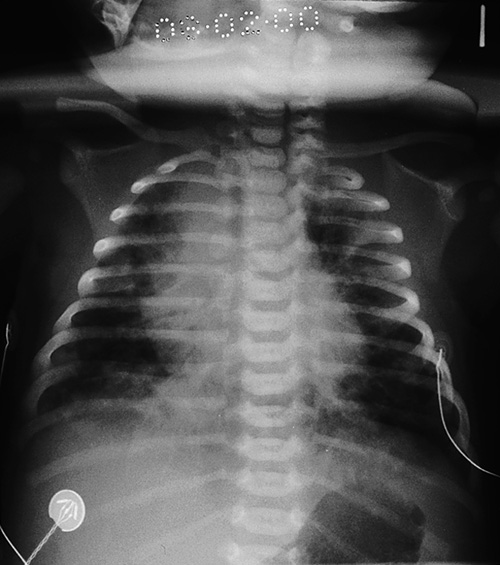
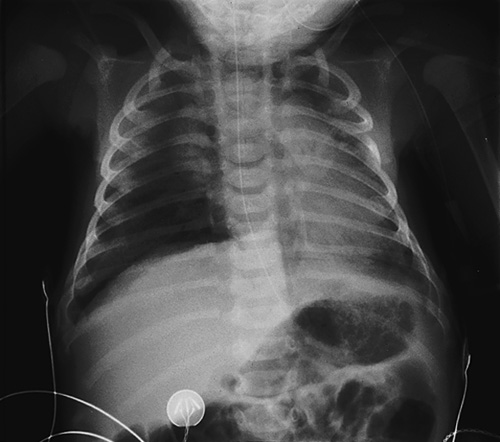
50 Good-quality neonatal care is extremely important, and may have key implications for the rest of a baby’s life. Those born prematurely need skilled intensive support, and those born with presumed hypoxia need resuscitation, prompt assessment and appropriate subsequent care. The early neonatal period is often the time when congenital abnormalities become apparent and precise diagnosis and management can make a difference to the quality of life, or even influence whether the baby will live or die. The aim of this chapter is not to provide a comprehensive guide to neonatal care, but rather to highlight some of the more common neonatal problems which can occur. It is essential that the obstetrician, midwife, paediatrician, neonatologist and neonatal nurse collaborate closely as a team. High-quality communication is essential if decision-making is to be optimized. The apparent ease with which most babies make the transition from fetal to neonatal life conceals a host of complex physiological changes in virtually every system. Several relatively common neonatal disorders are related to difficulties with this transition. The fetal lung at term contains about 100 mL of liquid. This equals the functional residual capacity and in a sense, the fetal lung can be said to form around a liquid cast of the future air spaces. Lung fluid is formed by alveolar cells, and fluid is essential for normal lung growth and development. The fluid must be cleared at birth to make way for air, and failure to do so leads to breathlessness. This is known as transient tachypnoea of the newborn (TTN). It may last for a day or two, and is commoner after elective caesarean section. Respiratory distress syndrome (RDS) is caused by a deficiency of surfactant and is commoner in pre-term infants (0.1% at term vs 30% at 28 weeks). Surfactant, a complex lipoprotein consisting largely of phosphatidyl choline, is synthesized by type II pneumocytes within the alveoli and is important in reducing surface tension, allowing the alveolus to expand. Hypoxia, acidosis and hypothermia reduce surfactant production; antenatal steroids increase production and thereby reduce the incidence of RDS. Clinically there is tachypnoea, grunting and intercostal recession commencing within the first 4 h of life, low oxygen saturations requiring oxygen and the chest X-ray demonstrates a generalized reticulogranular appearance referred to as like ‘ground glass’ (Fig. 50.1). Some babies improve with supplemental oxygen or continuous positive airways pressure (CPAP), but increasing respiratory distress and oxygen requirements are indications for intubation and administration of artificial surfactant via an endotracheal tube. Fig. 50.1Respiratory distress syndrome following emergency caesarean section. The mother had diabetes, which predisposes to respiratory distress syndrome. Note the ground-glass appearance of the lungs. Meconium aspiration syndrome is also a potentially serious respiratory complication. In utero, meconium is usually retained within the colon. Although it may be passed through the sphincter under physiological conditions, particularly after 40 weeks, it also has an association with fetal hypoxic stress. Meconium is irritative to the neonatal lungs and may lead to a pneumonitis, the meconium aspiration syndrome (Fig. 50.2). Clinical features range from mild neonatal tachypnoea to severe respiratory compromise. The incidence is probably unrelated to fetal pH (and indeed the majority of babies with meconium aspiration syndrome are not acidotic at delivery) but the syndrome is more likely to be severe if there is associated acidosis. It is also more severe when the meconium is thick. Treatment is with oxygen, mechanical ventilation, surfactant therapy (as meconium can displace or inactivate endogenous surfactant) and, if very severe, extracorporeal membrane oxygenation ± pulmonary lavage. The switch from fetal to neonatal circulation is normally made rapidly after birth. The key event is relaxation of the smooth muscle in the pulmonary blood vessels, which is triggered by the entry of oxygen into the lung with the first breath (note this paradoxical response to oxygen, which is the opposite to that of all other blood vessels). In some babies, especially when there has been prolonged fetal hypoxia, this circulatory switch does not occur and may itself lead to further hypoxia. This condition is known as persistent fetal circulation and is difficult to distinguish clinically from congenital cyanotic heart disease. Although the fetal kidney is important in maintaining the amniotic fluid volume, it has a negligible role in the excretion of waste products. After birth, the kidney must excrete all the body’s waste, as well as conserve fluid. In a baby born at term, the kidney is just able to manage this role, although there is always an initial rise in the blood urea and creatinine concentrations. The maximum urine osmolality, which the newborn can attain is about 600 mmol/L (compared with 1800 mmol/L in the adult) and it is therefore not surprising that dehydration and electrolyte disturbances are common complications of neonatal illness. The fetus swallows amniotic fluid at about the same rate as it is produced, and deficiencies in fetal swallowing result in polyhydramnios. If there has been polyhydramnios, the baby should be examined for swallowing problems and should have an orogastric tube passed in order to exclude complete oesophageal atresia. The term fetus has a high haemoglobin concentration, at around 18 g/dL. This is a response to the low arterial oxygen tension (3–4 kPa) which characterizes the latter part of intrauterine life. Once the oxygen tension rises after birth, this high haemoglobin is no longer needed, and falls to around 10 g/dL by about 8 weeks of age. The white cell count at birth is high (12–20 × 109/L) and polymorphs predominate. By 4 days of age, it is usually in the range 7–12 × 109/L and is mainly lymphocytic. There are several routine observations and procedures to perform on the newborn shortly after birth, but, providing the baby does not need to be resuscitated, none of them should be allowed to prevent the mother from seeing and holding her baby as soon as possible. The baby’s condition at 1 and 5 min of age is assessed by means of the Apgar score (see Table 49.1). The purpose of this is to have a reasonably objective record of how the baby initially responded to the challenge of extrauterine life. It serves as a guide to the need for resuscitation, but, unless the score fails to improve with resuscitation, it has very little predictive value for later disability. A low Apgar score is not synonymous with birth asphyxia. It could, for example, be a reflection of a pre-existing fetal problem or of sedation caused by the maternal drug administration. Newborn babies can lose heat faster than they can generate it (Box 50.1). Hypothermia is dangerous and must be prevented. The delivery room must be warm and draughts kept to a minimum. The baby should be immediately dried and wrapped in dry towels or blankets, with a hat put on to prevent heat loss from the head. If resuscitation is required, it should be performed under a radiant heater. Pre-term babies are routinely delivered into polythene bags to minimize evaporative losses and improve temperature control. Providing all appears well, all that is needed in the labour ward is a brief examination for any obvious external abnormalities. A full routine examination should be deferred until later. Weight, length, and head circumference measurements provide an assessment of how well the baby has grown in utero and are a baseline against which to judge subsequent growth. Table 50.1 gives some normative term data and such data are also available for neonates born at earlier gestations. Table 50.1 Some dimensions of an average male* infant at 40 weeks * Females are about 10% smaller. The cord should be checked to see whether it contains the usual two arteries and one vein. A single artery has a 20% association with congenital abnormalities, mainly of the genitourinary system. A plastic cord clamp should be fixed so as to leave about 2 cm of cord proximally. Subsequent care of the cord involves ensuring it is kept clean and dry. If the baby is likely to need intensive care, the cord should be left longer as it provides an accessible route for arterial and central venous cannulation. Vitamin K does not cross the placenta well and newborn babies have low serum concentrations and poor stores. They do not have gut bacteria to synthesize it for them, and human milk is a relatively poor source of the vitamin. Lack of vitamin K leads to shortage of clotting factors II, VII, IX and X, and about 1 in 1000 breast-fed babies will experience serious bleeding, a condition known as haemorrhagic disease of the newborn. The classical form occurs between days 1–7, although an early form occurs in infants born to mothers taking anticonvulsants and a late (and sometimes more serious form) may also occur, even up to 12 weeks after delivery. Bottle-fed babies are at less risk because formulae are supplemented with vitamins. Almost complete protection is provided by the administration of vitamin K 1 mg i.m. at the time of birth, and possibly less-complete protection is provided by giving vitamin K 2 mg orally twice in the first week (with a further oral dose at 1 month). Some epidemiological studies have found an association between i.m. vitamin K (as opposed to oral vitamin K) and childhood leukaemias, resulting in a swing away from treatment. Many large subsequent studies have failed to prove the connection. Evolution has equipped the fetus with a remarkable ability to tolerate asphyxia without adverse consequences, to the extent that sometimes 10 or 15 min of absolute anoxia can be compatible with normal survival. In practice, absolute anoxia only occurs with rare events such as massive placental abruption or cord prolapse. Asphyxia may lead to cerebral palsy, essentially a motor disorder affecting posture and movement which is variably accompanied by mental impairment, epilepsy or sensory defects. Despite popular belief, it is likely that less than 10% of cerebral palsy is caused primarily by perinatal asphyxia. Neonatologists are wary of making a diagnosis of perinatal asphyxia, unless there is a good antenatal history (e.g. abruption) together with neonatal ‘depression’ (e.g. poor Apgar scores) and evidence of subsequent multi-organ failure. Such multi-organ failure may present with seizures, cerebral oedema, oliguria, haematuria, coagulopathy, jaundice or occasionally pulmonary haemorrhage. The question of predicting the likelihood of neurological injury following a specific birth and the question of whether a subsequent developmental abnormality was caused by a specific intrapartum insult is seldom straightforward. Current evidence suggests that therapeutic induced hypothermia (‘cooling’) to a rectal temperature of 33–34°C for 72 h improves both survival and neurological outcome at 18 months of age in infants with moderate or severe perinatal asphyxial encephalopathy. Therapeutic hypothermia is considered in infants of > 36 weeks completed gestation, admitted to a neonatal unit with one or more of the following: Infants who fulfil one or more of the above criteria then require close observation for signs of seizures or moderate to severe encephalopathy evidenced by an:
Neonatal care
Introduction
The transition at birth
Respiratory system
Cardiovascular system
Genitourinary system
Gastrointestinal system
Haematological system
Routine care at birth
Assessment
Preventing hypothermia
Examination
Weighing and measuring
Weight
3500 g
Length
50 cm
Head circumference
35 cm
Brain weight
400 g (12% of body weight)
Blood volume
280 mL (80 mL/kg)
The umbilical cord
Preventing haemorrhagic disease of the newborn
Perinatal asphyxia
![]() Apgar ≤ 5 at 10 min of age
Apgar ≤ 5 at 10 min of age
![]() continued need for resuscitation, including endotracheal or mask ventilation, at 10 min after birth
continued need for resuscitation, including endotracheal or mask ventilation, at 10 min after birth
![]() acidosis within 60 min of birth (defined as any occurrence of umbilical cord, arterial or capillary pH < 7.00)
acidosis within 60 min of birth (defined as any occurrence of umbilical cord, arterial or capillary pH < 7.00)
![]() base deficit ≥ 16 mmol/L in umbilical cord or any blood sample (arterial, venous or capillary) within 60 min of birth.
base deficit ≥ 16 mmol/L in umbilical cord or any blood sample (arterial, venous or capillary) within 60 min of birth.
![]() altered state of consciousness (reduced or absent response to stimulation) and
altered state of consciousness (reduced or absent response to stimulation) and
![]() abnormal tone (focal or general hypotonia, or flaccid) and
abnormal tone (focal or general hypotonia, or flaccid) and
![]() abnormal primitive reflexes (weak or absent suck or Moro response).
abnormal primitive reflexes (weak or absent suck or Moro response).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree