Neonatal Arrhythmias
DEFINITION
Arrhythmias, alterations in the heartbeat rhythm, are a common problem in the newborn period. Many are now diagnosed in utero. We consider the tachycardias (rapid heart rhythms) first, then the bradycardias (slowed heart rhythms).
TACHYCARDIAS
The most commonly diagnosed fetal arrhythmias are premature atrial contractions (PACs), which often resolve soon after birth. The other tachycardias frequently seen in the fetus and the newborn period are atrial tachycardia, atrial flutter, and the more usual reentrant-type supraventricular tachycardia (SVT).1–3
Differential Diagnosis
It is often necessary to distinguish sinus tachycardia from a true tachyarrhythmia. The normal resting heart rate for infants varies with gestational age, with term infants at 130–150 beats per minute (bpm). Preterm infants have slightly faster rates, with an average resting heart rate of 160 bpm at 32 weeks. The average heart rate4 of a newborn is 145 with a range of 110–150 bpm.
It can be difficult to tell the difference between sinus tachycardia and an atrial tachycardia that originates close to the sinoatrial (SA) node based on the electrocardiographic appearance. If the clinical evidence is consistent with sepsis, dehydration, or blood loss, then it is likely that the rhythm is a reactive sinus tachycardia. Another helpful clue to sinus rhythm is the morphology of the P waves. With normal sinus rhythm, P waves are upright in leads I and aVF. In addition, one should see a biphasic P wave in V1. This is caused by the normal electrical depolarization of the atria that begins in the right atrium, spreads to the left atrium, then proceeds to the AV node.
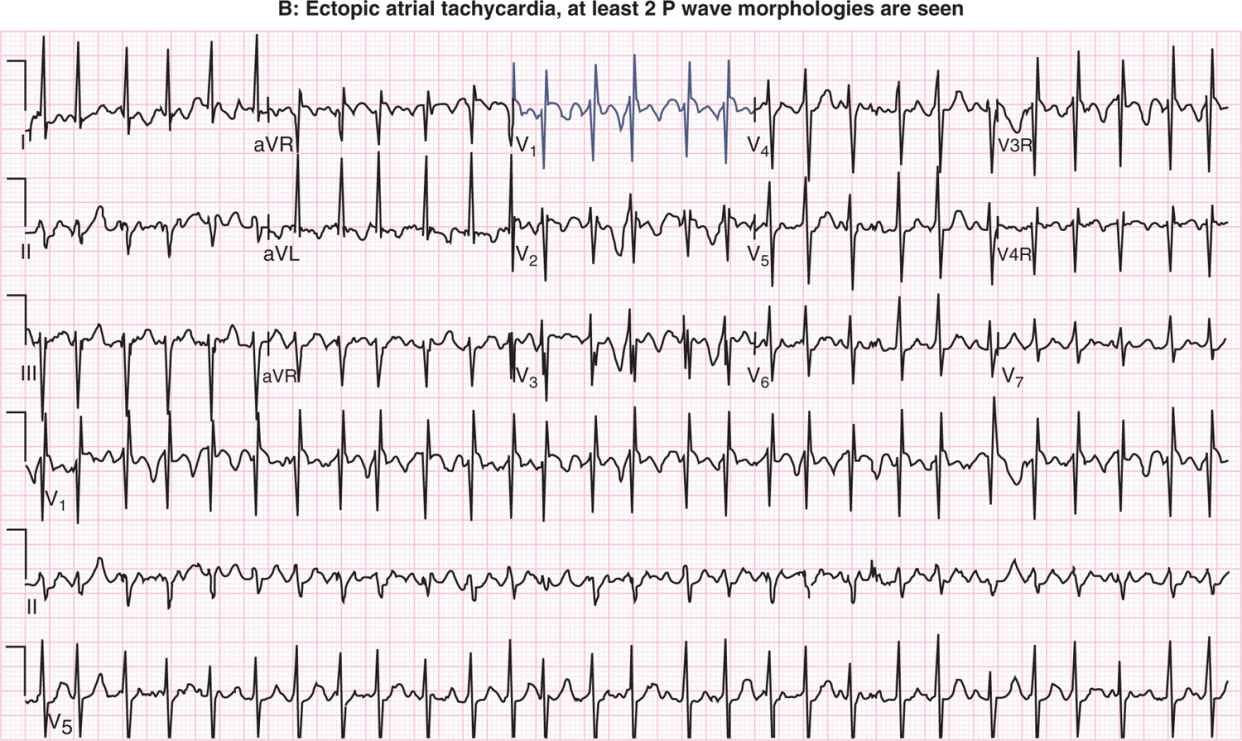
If the baby is being monitored on telemetry, there may be a clear change in P-wave morphology or axis that will suggest PACs or an ectopic atrial rhythm. The PR interval may also prolong.5 Figure 21-1 shows a comparison of sinus tachycardia and atrial tachycardia.
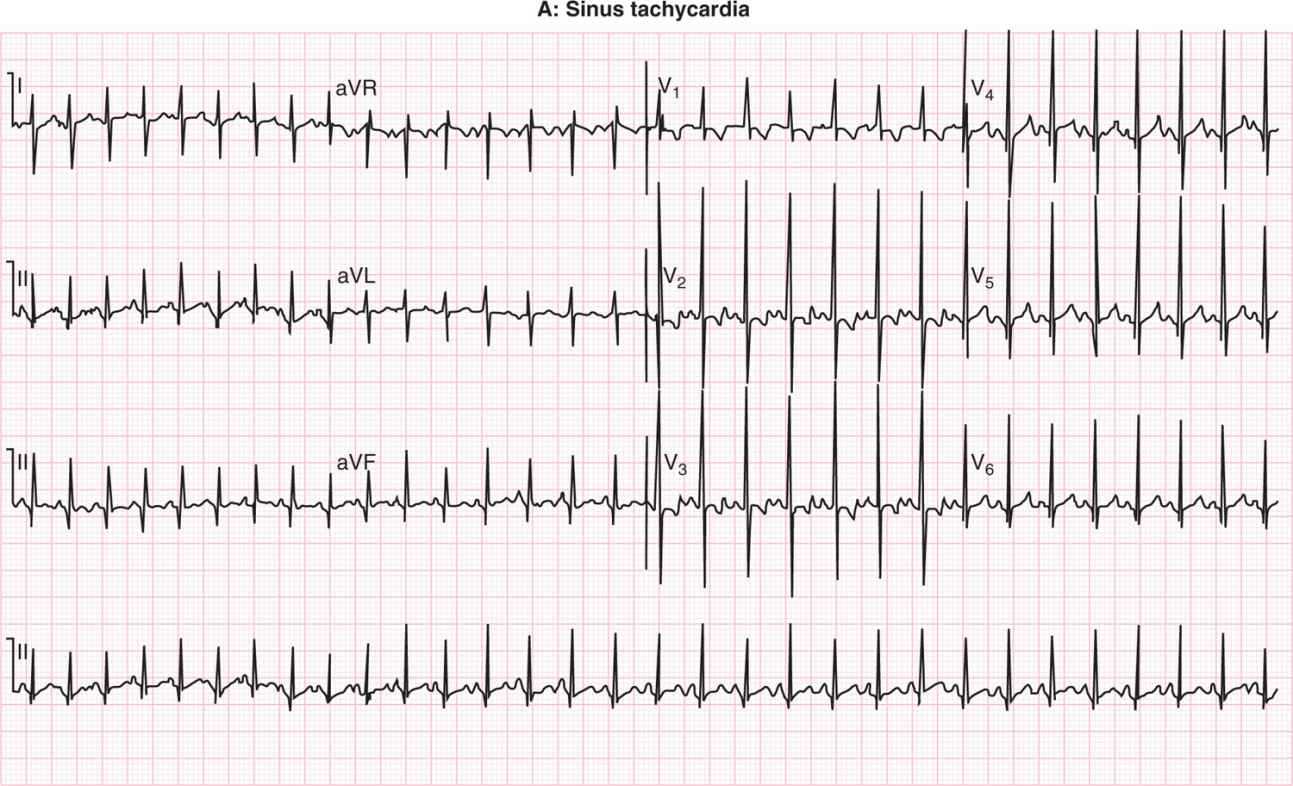
FIGURE 21-1 A, Sinus tachycardia vs B, ectopic atrial tachycardia (EAT). In sinus tachycardia, there is 1 P-wave morphology; in EAT there are at least 2 different P-wave morphologies.
The PACs look similar to sinus beats with a P wave preceding each QRS complex, but these occur earlier than expected. The P wave may be buried in the preceding T wave if the heart rate is increased. If they occur in a pattern of every other beat with sinus beats, they are called atrial bigeminy. Both of these rhythms are usually benign and self-limited but can occur if there is a central line within the right atrium or electrolyte disturbances.
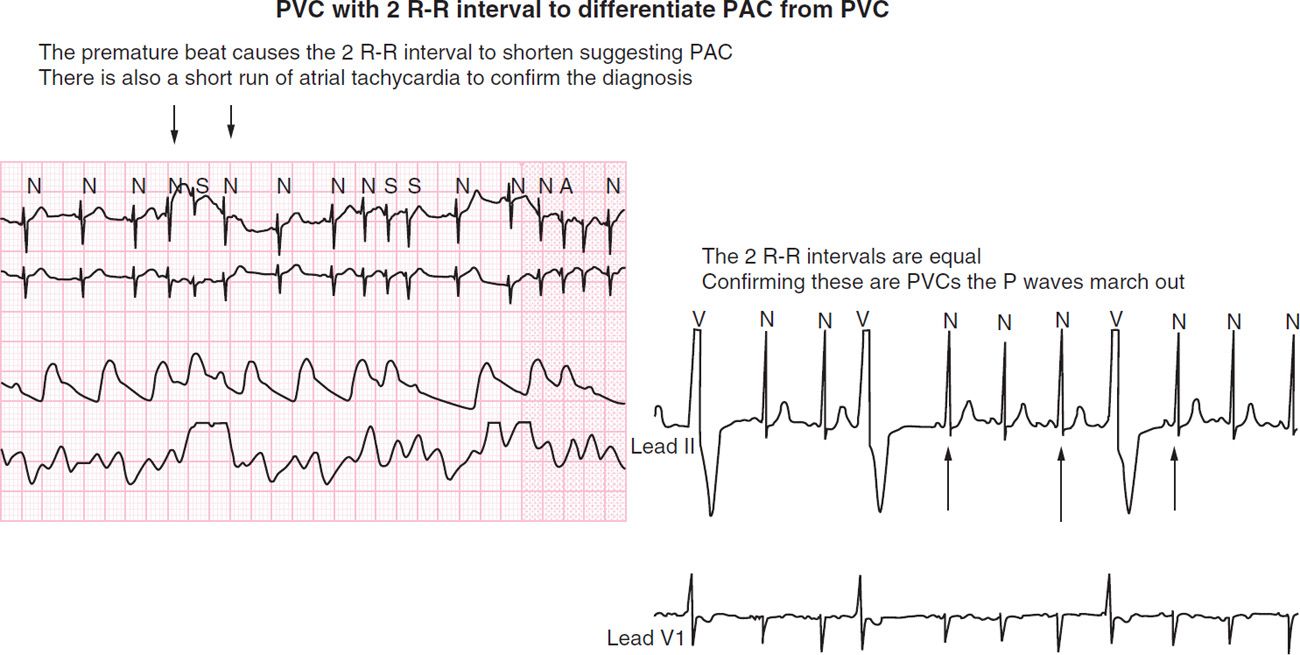
If the PAC is conducted aberrantly, there is often a question regarding whether it is a premature ventricular contraction (PVC) or PAC. It is helpful to invoke the 2 R-R rule to differentiate the origin of the premature beat. If the 2 R-R interval just prior to the premature beat is longer than the 2 R-R interval that contains the premature beat, that suggests a PAC. If the 2 R-R interval containing the premature beat is identical to the previous one, this is consistent with a PVC. This is because, typically, the atrium as unaffected by the early beat, continues its own timing, sends out the next P wave on time, and is then conducted normally. The atrium does not change its timing, and this creates what is called the “compensatory pause” for the QRS or ventricular complex. On the other hand, if the premature beat came from the atrium, it will penetrate the sinus node and reset the pacemaker, and the 2 R-R interval that includes the premature beat will be shorter than the preceding one (Figure 21-2).
FIGURE 21-2 Premature atrial contraction (PAC) vs premature ventricular contraction (PVC). On left, PACs with normal conduction will be narrow. On right, simultaneous tracing in leads II and V1. PVCs will have a wide complex. PVCs do not affect the next atrial beat and therefore cause a compensatory pause in the ventricular beat. PACs do affect the next atrial beat, making it come earlier (or advancing it); therefore, no compensatory pause is seen.
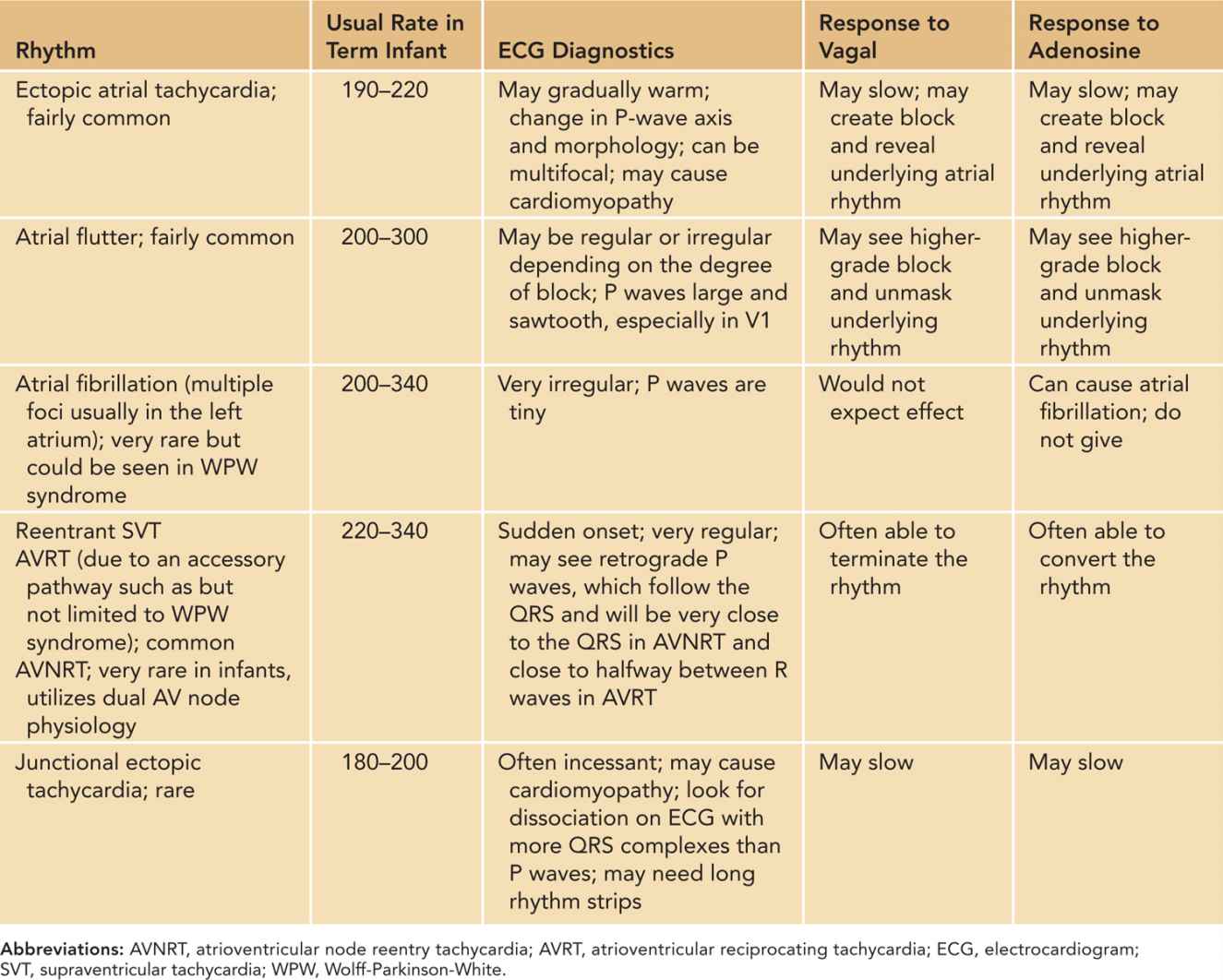
The pathophysiology of each tachycardia is different. Table 21-1 provides the differential diagnosis of SVT and response to adenosine. Ectopic atrial tachycardia comes from an area of atrial tissue that depolarizes and activates the atrium at a rate more rapid than the sinus node. The ectopic focus may be sensitive to catecholamines and inotropic medications.
Table 21-1 Differential Diagnosis of Supraventricular Tachycardia
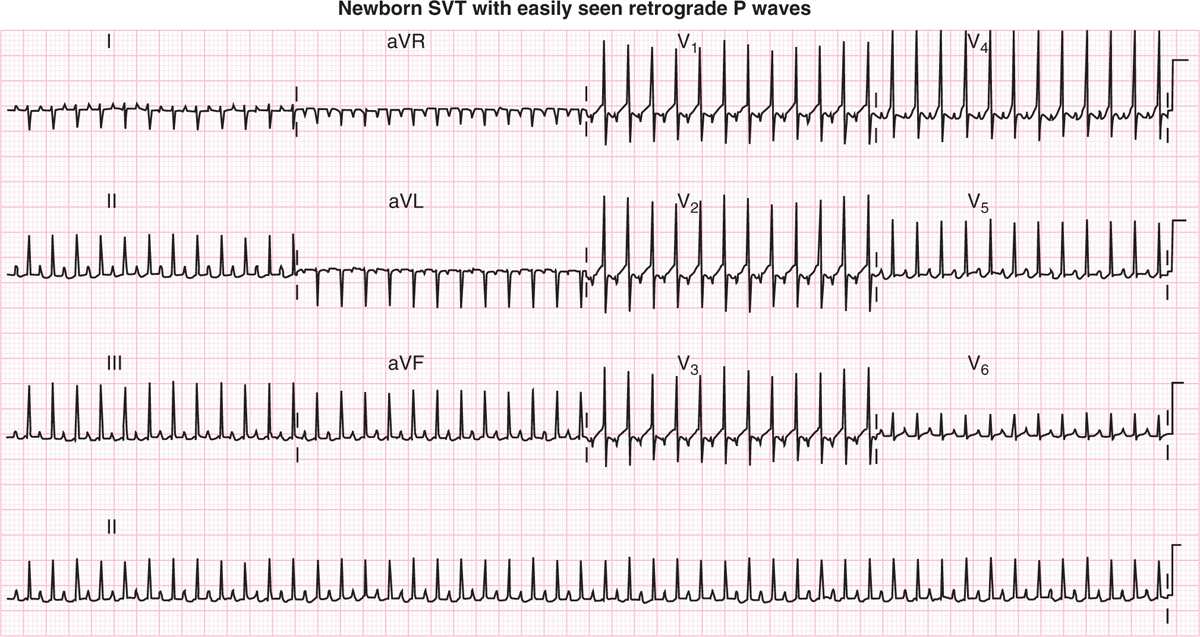
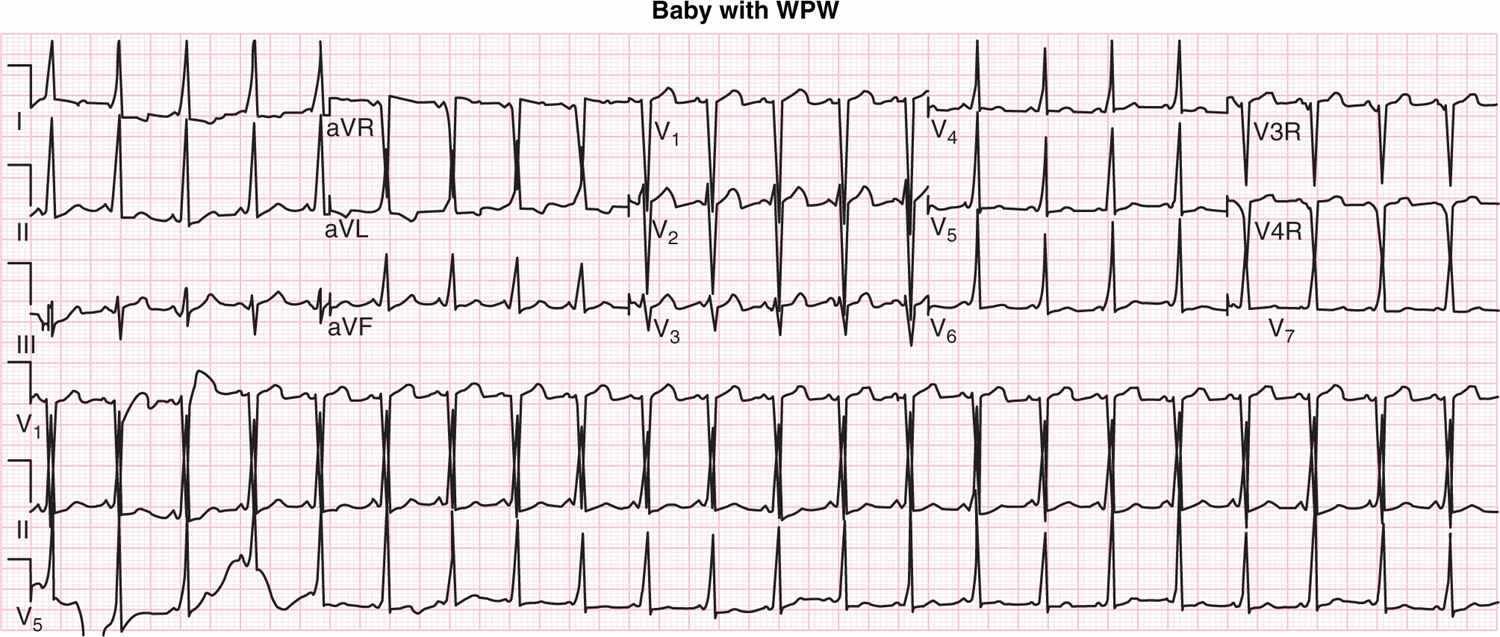
The more usual form of reentrant SVT is caused by an accessory pathway. In Wolff-Parkinson-White (WPW) syndrome, the pathway conducts in sinus rhythm and is therefore evident on the electrocardiogram (ECG). By depolarizing an area of ventricular myocardium earlier than would happen if conduction were only via the AV node, the accessory pathway causes the QRS complex to widen on the ECG in the pattern we refer to as preexcitation or a delta wave. Many patients do not have WPW syndrome or a delta wave, but do have SVT, which is caused by a concealed accessory pathway or one that does not conduct in sinus rhythm or show itself on an ECG. The most common ECG appearance of SVT will be a narrow complex at a rate of 240–300 bpm (Figure 21-3).
FIGURE 21-3 Narrow-complex supraventricular tachycardia (SVT). The mechanism for this rhythm is a reentrant circuit that uses the atrioventricular (AV) node as the antegrade limb and an accessory pathway as the retrograde limb. The P wave is almost equidistant between the R waves, which suggests the retrograde conduction time along the accessory pathway.
If the infant is in SVT, it is not possible to tell if there is WPW syndrome. Once in sinus rhythm, delta waves may become apparent (Figure 21-4).
FIGURE 21-4 Electrocardiogram (ECG) in sinus rhythm shows Wolff-Parkinson-White (WPW) syndrome. There is a pattern of preexcitation with delta waves.
Staying within the atrium, another common tachyarrhythmia in neonates is atrial flutter. This rhythm is a reentrant circuit, contained within the atrium in a stereotypic pattern. The circuit ascends the atrial septum, crosses over the superior portion of the atrium, and then descends along the lateral atrial wall, where it then traverses the isthmus between the inferior vena cava (IVC) and the tricuspid valve and then turns back up the atrial septum. This creates the classic “sawtooth” flutter waves seen best in V1. The rate of the atrial flutter is usually 240 to 300 bpm in older children and adults, but it is substantially faster in newborns (400–600 bpm). The flutter rate is determined by the physics of the atrium and the distance covered in each lap. This is also a common arrhythmia in fetal life.6 If the rhythm does not convert spontaneously at birth, it is easily treated with cardioversion and usually does not recur.
Fast Rhythms that Involve the Atrium, the AV Node, and the Ventricle
Fast rhythms that involve the atrium, AV node, and ventricle are otherwise known as typical reentrant SVTs. Many of these patients will have WPW syndrome, but not all; SVT and WPW syndrome are not synonymous. This is confounded by the phenomenon of a delay in the appearance of preexcitation or delta waves for several days after birth or conversion to sinus rhythm. ECGs done in tachycardia will usually show narrow-complex tachycardia in the range of 270–320 bpm. At that rate, P waves are almost impossible to see but may be appreciated on the upstroke of the T wave. If that is seen, it helps to envision the mechanism of tachycardia in these patients; the SVT circuit in these patients is usually down the AV node and then back up the accessory pathway. The circuit involves both atrium and ventricle, and conduction time from ventricle to atrium via the pathway is shorter than conduction time from atrium to ventricle over the AV node.
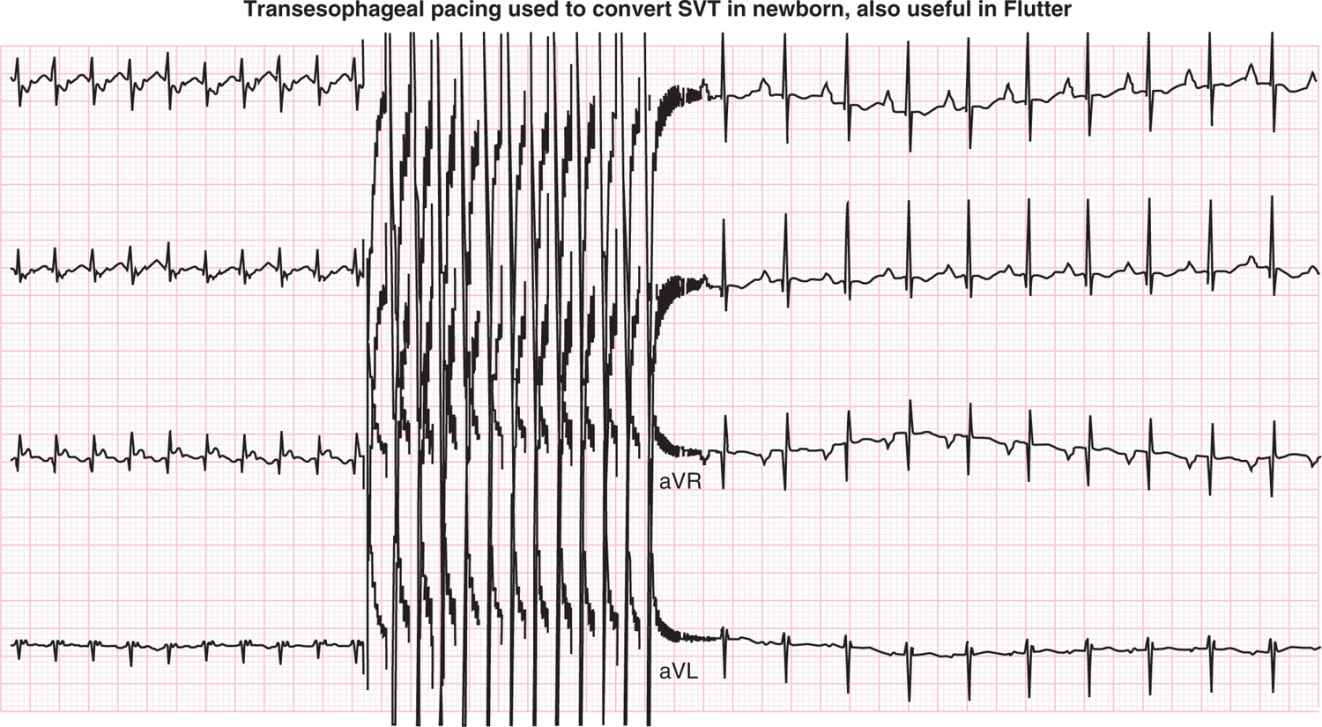
Figure 21-5 shows atrial flutter with variable block and transesophageal pacing used to convert reentrant SVT.7,8 This type of pacing may also be used for conversion of atrial flutter.
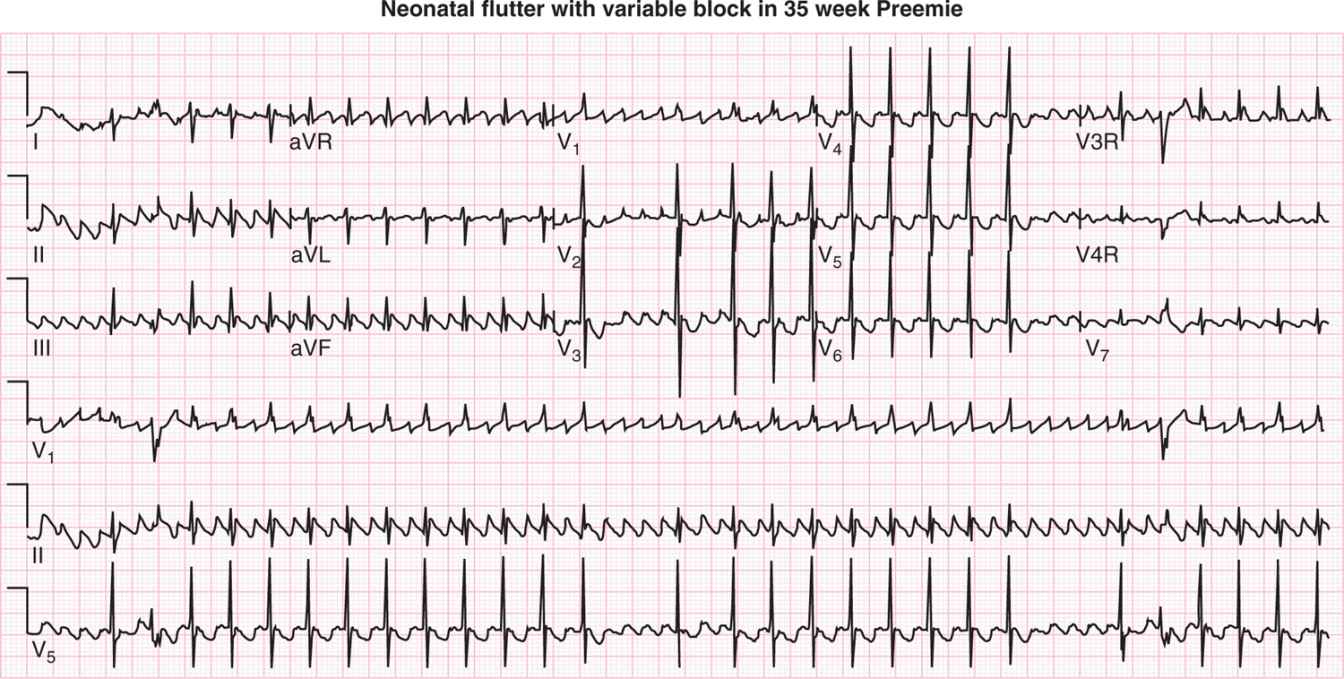
FIGURE 21-5 A, Atrial flutter: a macroreentrant rhythm confined to the atrium that produces large, sawtooth P waves. There is also variable atrioventricular (AV) block. B, Transesophageal pacing may be used to convert supraventricular tachycardia (SVT) as in this case or for atrial flutter.
Atrial fibrillation would be an unusual rhythm to see in a neonate with normal cardiac anatomy and function but might be seen in the setting of an inflammatory process such as myocarditis. It is recognizable by its irregularity and small, sometimes almost invisible, P waves. More often in infants, one may see chaotic atrial tachycardia, characterized by irregular discrete P waves of varying morphology.
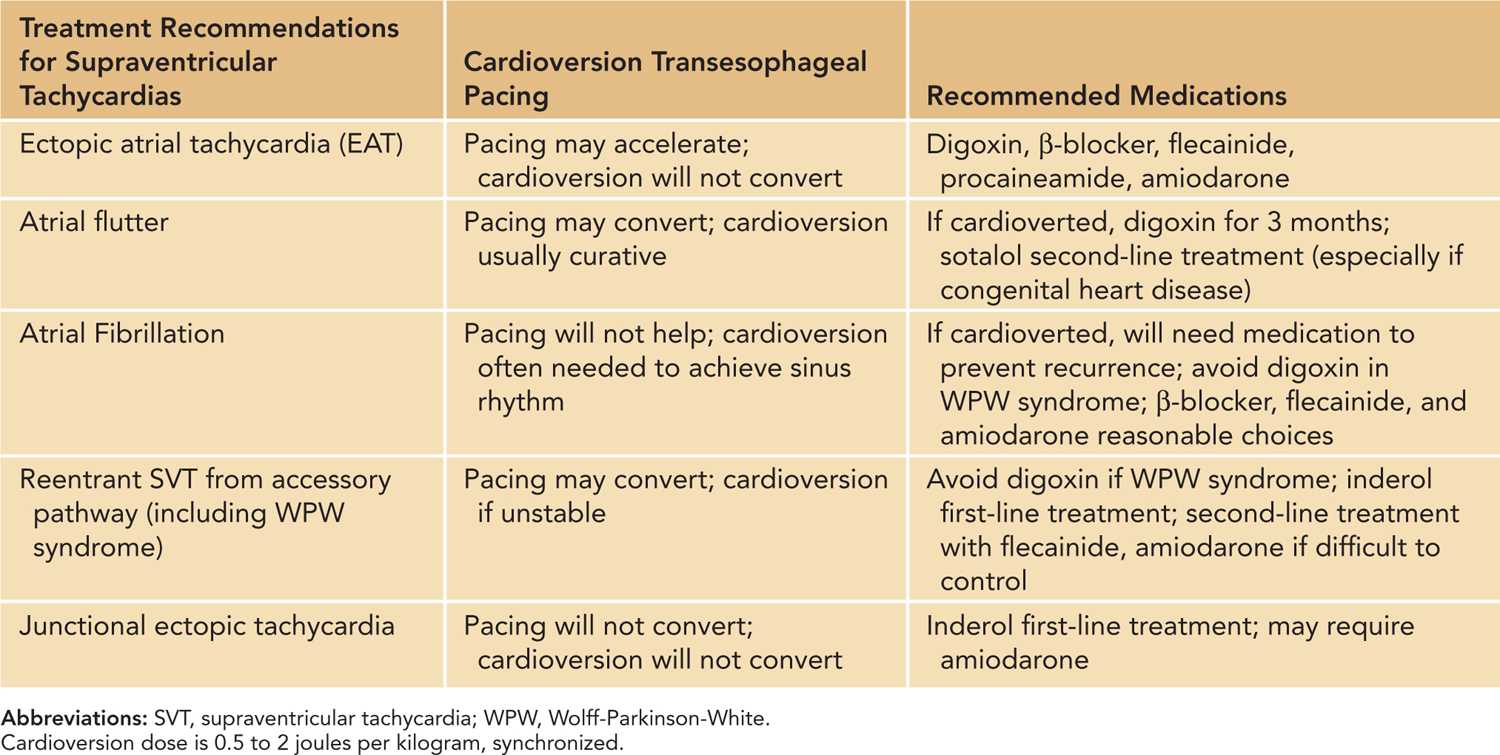
Table 21-2 indicates the treatment of SVT.9–12
Table 21-2 Treatment of Supraventricular Tachycardia
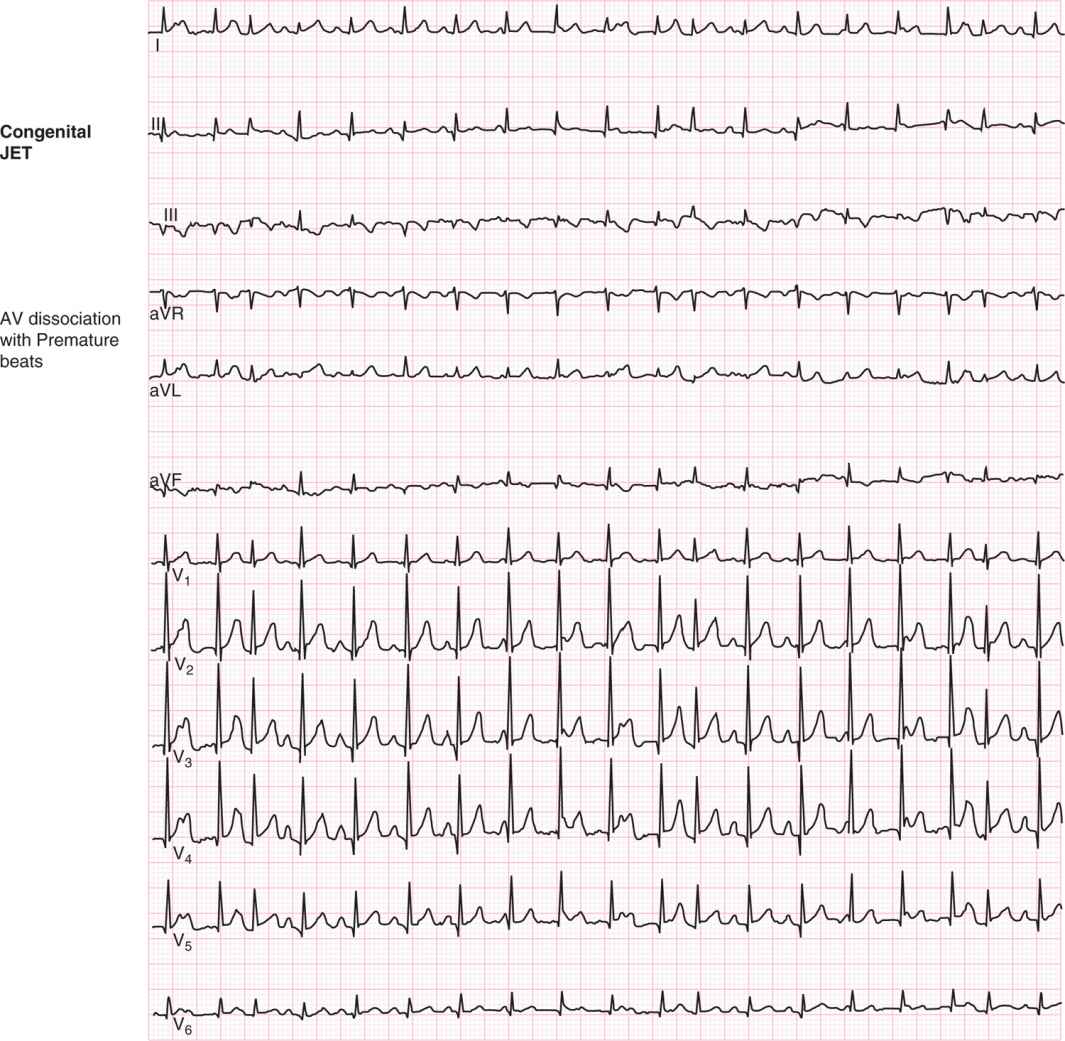
Moving lower in the heart and its conduction system, we come to the AV node or junction. This part of the heart is capable of becoming the auxiliary pacemaker if the sinus node fails; it may become inflamed and become an origin for ectopic tachycardia or cause too slow or blocked conduction if traumatized by surgery, inflammation, or intrauterine exposure to antibodies against itself. The ECG pattern in junctional tachycardia will characteristically show a narrow-complex rhythm and may or may not show P waves. If P waves are seen, they will typically be in a pattern of AV dissociation, with a slower atrial rate than ventricular rate and occasional sinus capture beats that advance the tachycardia.13 If there is, instead, 1:1 retrograde conduction from the focus to the atrium, P waves will be superimposed on the QRS complex and therefore not visible. Occasionally, they can be appreciated immediately after the QRS complex. In this case, one may appreciate the axis of the P waves as negative in II, III, and aVF as well, which suggests that the origin is from an area inferior to the sinus node.
Negative P waves seen before the QRS complex do not have the same significance; there may be an inferior atrial origin of the rhythm, but it is not junctional. Another feature of junctional rhythm, whether fast of slow, is that it is not driven by the atrial rate. If you are able to document dissociation, in that there are different atrial and junctional rates, with the junctional rate faster than the atrial and a regular rate for both, you have good evidence of junctional rhythm (Figure 21-6).
FIGURE 21-6 Junctional ectopic tachycardia (JET; after repair of tetralogy of Fallot) with atrioventricular (AV) dissociation. There are also premature atrial contractions (PACs), which conduct with a slightly wider QRS complex. This helps differentiate JET from ventricular tachycardia (VT), for which the QRS duration in the tachycardia would normally be wider or longer than the sinus capture beats.
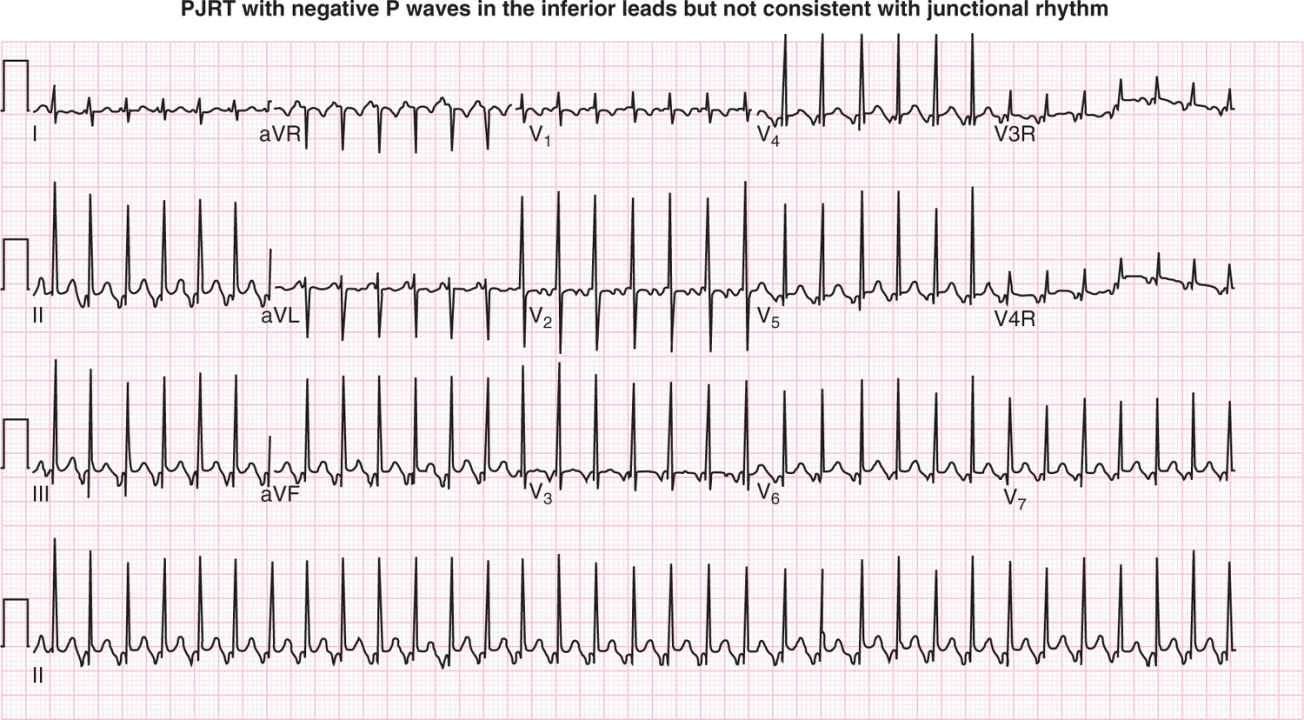
A rare rhythm that is confused with junctional rhythm is persistent (permanent form of) junctional reciprocating tachycardia (PJRT). This rhythm has inverted P waves, but they occur just prior to the QRS complex and are due to retrograde conduction along a slow-conducting accessory pathway. The negative P waves are seen in the inferior leads because the pathway comes near the posterior inferior portion of the right atrium near the coronary sinus os and the AV node. Because the tachycardia utilizes such a slow-conducting pathway, the patients tolerate it for much longer than the usual reentrant SVT. Eventually, it can cause a decrease in function and cardiomyopathy (Figure 21-7).
FIGURE 21-7 Persistent (permanent form of) junctional reciprocating tachycardia (PJRT) caused by a slow-conducting accessory pathway, which may cause incessant tachycardia. In this form of supraventricular tachycardia (SVT), the time taken to conduct retrograde from the ventricle to the atrium is reflected by the long V-to-A time (or R to P). The resultant P waves are also negative in the inferior leads, consistent with a right-sided posterior and inferior accessory pathway.
Fast Rhythms that Originate in the Ventricle
The epidemiology of ventricular tachycardia (VT) includes systemic problems, such as viral myocarditis, metabolic disease, electrolyte abnormalities, and genetic channelopathies, including long QT syndrome (LQTS). This rhythm, possibly more than any other, taxes clinicians in terms of the immediate response. The dilemma is to make the diagnosis and then to decide whether the patient is stable.
The differential diagnosis of wide-complex tachycardia includes benign ventricular accelerated rhythm of the newborn, sinus rhythm with a bundle branch block, SVT with aberrancy, SVT with antegrade conduction along the accessory pathway, and VT.
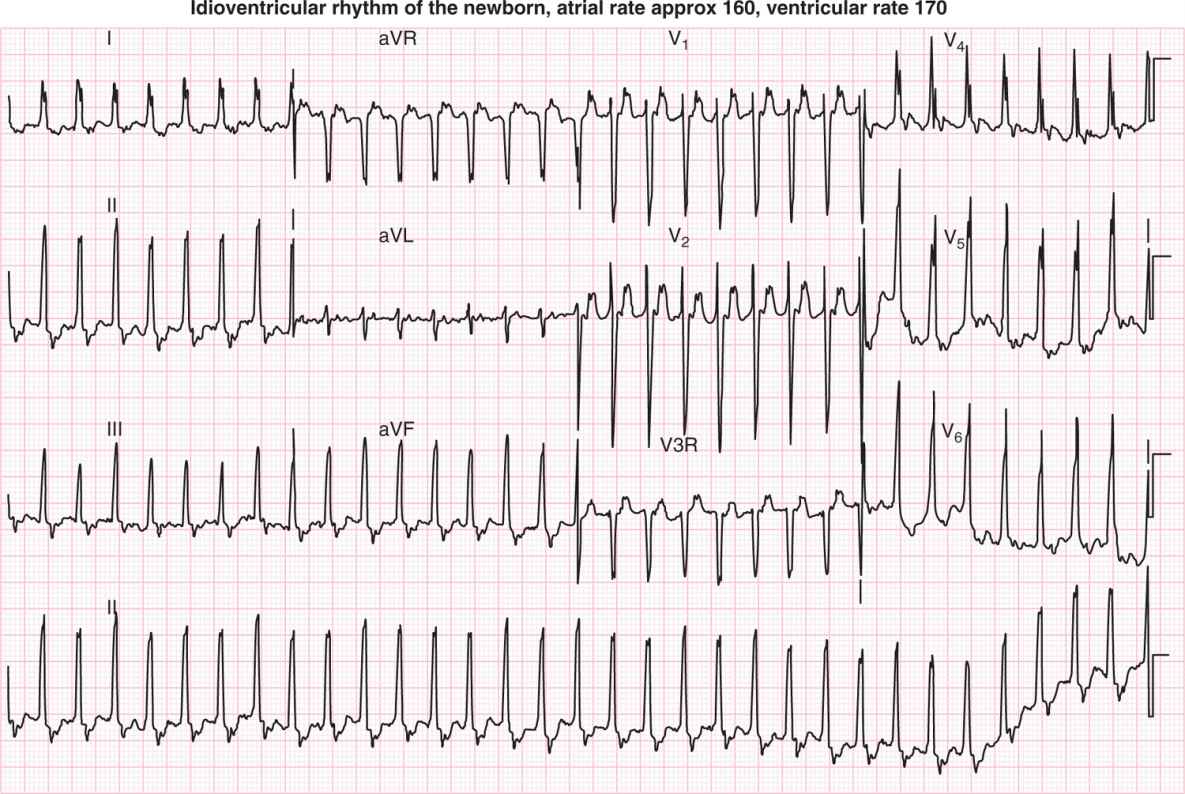
Benign ventricular rhythm of the newborn occurs when the ventricular pacemaker is slightly faster than the sinus pacemaker at a rate that is usually 140 to 170 bpm. It may require a long rhythm strip to demonstrate dissociation. It resolves spontaneously but can also be suppressed with beta blockers (Figure 21-8).
FIGURE 21-8 Idioventricular rhythm of the newborn. The ventricular rate is slightly faster than the atrial rate.
Pathophysiology
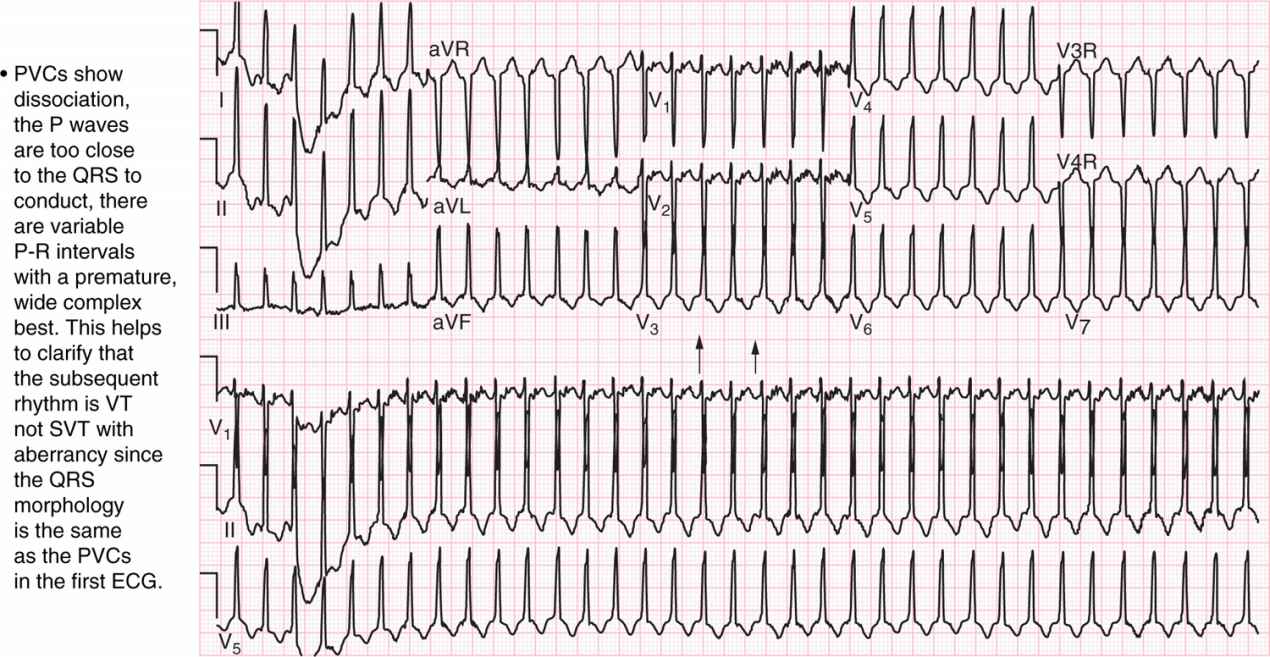
Rhythms coming from 1 of the ventricles will have a widened QRS duration for age. For a neonate, the normal QRS duration is 40 ms or 1 small box on the ECG paper at the usual recording speed of 25 mm/s. If the QRS duration is 80 ms, it is considered wide. This occurs because of the ventricle being activated gradually as the electrical depolarization makes its way across the myocardium without the aid of the usual conducting tissue. VT from the left ventricle will make the ECG look like there is a right bundle branch block. VT from the right ventricle will make the ECG look like there is a left bundle branch block. Just as with a junctional rhythm, there will be dissociation with 2 separate rhythms in progress, the atrial and the ventricular, without 1 affecting the other consistently. The AV node is capable of both antegrade (the usual pattern of conduction from the atrium to the ventricle) and retrograde (from the ventricle to the atrium) conduction, especially in the young. If that phenomenon is occurring, one may see retrograde (after the QRS) P waves in VT similar to that seen in junctional rhythm. Unlike junctional rhythm, in VT the QRS complex should be wide for age (Figure 21-9).
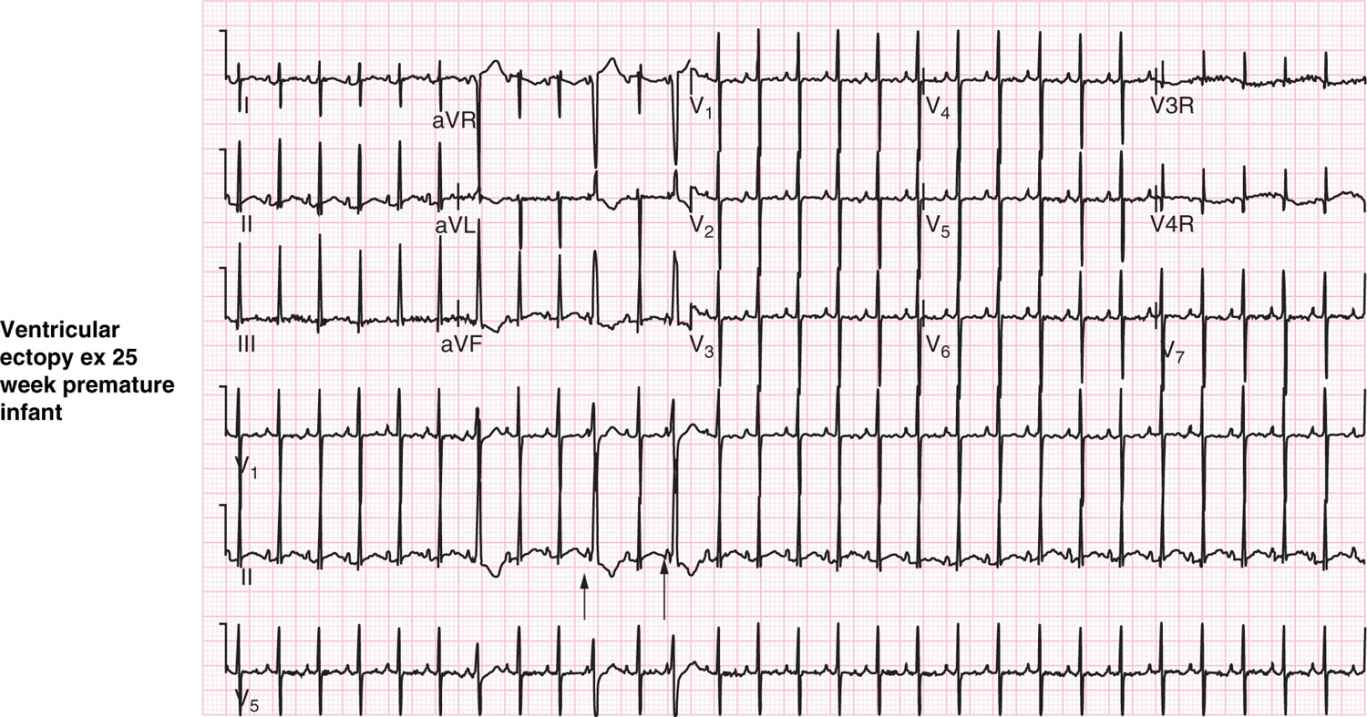
FIGURE 21-9 A, Premature ventricular contractions (PVCs) and B, ventricular tachycardia in an ex 25-week preemie. The PVCs show dissociation and widened QRS complex. This helps to clarify that the subsequent rhythm is ventricular tachycardia (VT) and not supraventricular tachycardia (SVT) with aberrancy. ECG, electrocardiogram.
Treatment
If there is sinus tachycardia, the baby needs to be treated for the underlying cause, such as dehydration. Medications or treatments to address a primary tachycardia in this setting may make the infant more ill. For example, if the baby has a heart rate above normal (210 bpm for an infant at 36 weeks’ gestation) and is hypotensive secondary to sepsis, drugs such as β-blockers can make the hemodynamic situation worse.
Treatment options for tachyarrhythmias above the ventricle depend on the exact rhythm. Table 21-3 presents a selected formulary.
Table 21-3 Drug Doses: Selected Formulary