Natural Family Planning: Periodic Abstinence and Withdrawal
Periodic abstinence as a method of contraception (also called fertility awareness) is keyed to the observation of naturally occurring signs and symptoms of the fertile phase of the menstrual cycle. This method must take into account the viability of sperm in the female reproductive tract (2 to 7 days) and the lifespan of the ovum (1 to 3 days). The variability in the timing of ovulation is the reason why the period of abstinence must be relatively lengthy unless barrier methods are used during the fertile days.
The period of maximal fertility begins 5 days before the day of ovulation and ends on the day of ovulation.1,2 The probability of conception plummets the day after ovulation; however, conception occasionally occurs more than 6 days before ovulation or immediately following ovulation.3 The likelihood of pregnancy steadily increases during this period of fertility and is highest the day of ovulation and the preceding 2 days.1,3,4 Ovulation occurs at the following median times (note the relatively wide ranges)5:
16 hours after the LH peak (range: 8 to 40 hours).
24 hours after the estradiol peak (range: 17 to 32 hours).
8 hours after the rise in progesterone (range: 12.5 hours before to 16 hours after).
12 to 16 days before the onset of menses, depending on cycle length.
Implantation occurs from 6 to 12 days after ovulation.6 In the great majority of instances, hormonal evidence of implantation can be detected 8 to 10 days after ovulation. The chance of early miscarriage increases when implantation occurs later than day 10 after ovulation.
In 2002, about 1.6% of reproductive age contracepting women in the United States utilized some method of fertility timing compared with 2.3% in 1995.7,8 This represented a dramatic decline since the 1960s.9 Worldwide, it is estimated that 3.6% of reproductive age women use a method of periodic abstinence, with a high prevalence that reaches nearly 20% in parts of South America.10 Adherence to this method requires commitment from both partners; it is a way of life. Unsuccessful use can be predicted in couples who are unable to part with sexual spontaneity, women with irregular menses, disorganized people who cannot keep good records, and women with chronic problems of vaginitis or cervicitis. The advantage of periodic abstinence as a method of contraception is the availability of this method regardless of
economic status or the accessibility of other methods. Users of this method also avoid religious proscription and the need to use “unnatural” substances.
economic status or the accessibility of other methods. Users of this method also avoid religious proscription and the need to use “unnatural” substances.
Methods of Periodic Abstinence
There are several specific methods, and most teachers of periodic abstinence advocate the incorporation of features from more than one method.11 Printed forms facilitate the careful record keeping required to accurately estimate the fertile days each month. The sophistication of these methods was made possible by the tremendous increase in the scientific knowledge of the events in the human menstrual cycle. The time of ovulation (the fertile period) was identified in the 1930s, but it was not until the 1960s with the advent of the radioimmunoassay that relatively precise timing of the various events became possible.
The Rhythm or Calendar Method
This method of periodic abstinence was based on the assumption that menstrual cycles were relatively constant, and therefore, the fertile period of the subsequent month could be predicted by the timing of the past cycle.
The general rule is to record the length of six cycles, then estimate the beginning of the fertile period by subtracting 18 days from the length of the shortest cycle, and to estimate the end of the fertile period by subtracting 11 days from the length of the longest cycle. Thus, a woman with cycles varying from 26 to 32 days will practice periodic abstinence from the eighth day until the 21st day, a formidable requirement of 14 days of abstinence per cycle. Indeed, because of the normal variation in menstrual cycles, the average couple would practice periodic abstinence 16 days each month.
This method is useful only for women who have relatively regular and consistent menstrual cycles. This method has a pregnancy rate of about 40 per 100 woman-years, and therefore, it is not advocated without combining it with other techniques. However, the utilization of programmed electronic devices to record temperatures, keep track of cycles, and provide a signal to the patient during the fertile period can reduce pregnancy rates to 5 to 10 per 100 woman-years.12,13
The Cervical Mucus Method
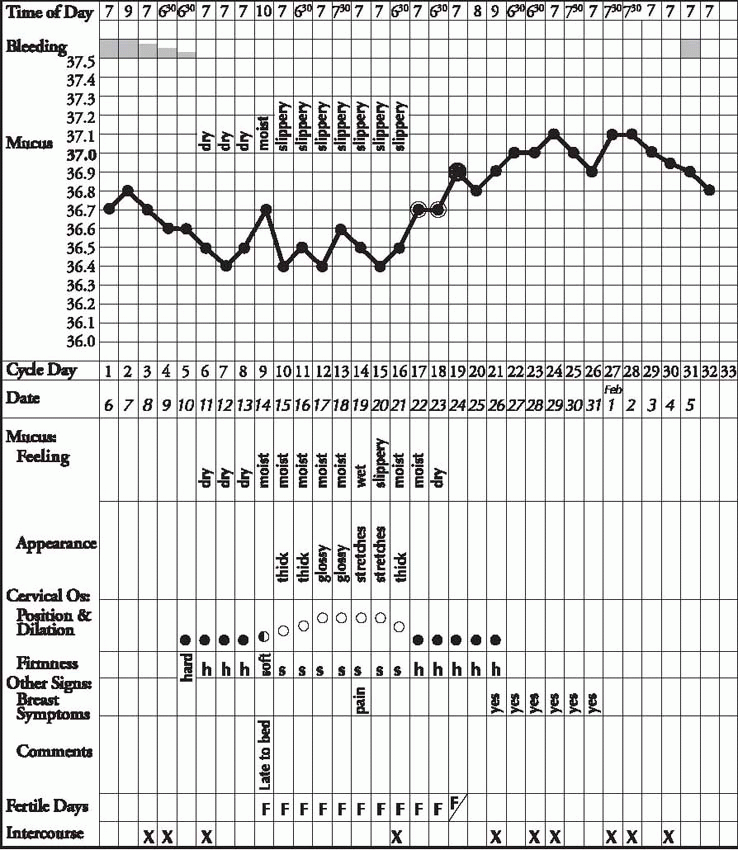
The effectiveness of periodic abstinence has been improved by the development of methods that allow decisions to be made within each cycle. The cervical mucus method is also called the ovulation method, the Billings method, the Creighton Model Fertility Care System, or the TwoDay method.14,15,16 This method requires sensing or observing the cervical mucus changes over time.17 A woman successfully practicing this method must become aware
of the estrogen-induced changes in cervical mucus that occur at midcycle: an increase in the amount of clear, thin, stringy mucus. Practitioners of this method describe these changes as wet and sticky (but slippery). The day of ovulation corresponds closely to the day of peak mucus.18 This method requires the maintenance of a daily record, at least in the beginning. Some recommend the addition of cervical palpation: firm and closed when infertile, soft, open, and moist when fertile.
of the estrogen-induced changes in cervical mucus that occur at midcycle: an increase in the amount of clear, thin, stringy mucus. Practitioners of this method describe these changes as wet and sticky (but slippery). The day of ovulation corresponds closely to the day of peak mucus.18 This method requires the maintenance of a daily record, at least in the beginning. Some recommend the addition of cervical palpation: firm and closed when infertile, soft, open, and moist when fertile.
The rules for intercourse are as follows:
1. Not on consecutive days during the postmenstrual preovulatory period so that seminal fluid will not obscure observation of cervical mucus changes, although assessment in the evening after intercourse that morning or the previous night should be reliable.
2. Abstinence when the mucus becomes sticky and moist.
3. Intercourse is permitted beginning on the fourth day after the last day of sticky, wet mucus. Most women (95%) will have 4 to 12 days of observable secretions; thus, the method requires a lengthy period of abstinence for many women.19
The Symptothermal Method
This method utilizes at least two indicators to identify the fertile period, usually combining the cervical mucus method with the basal body temperature (BBT). The BBT is recorded with any thermometer in the morning before getting out of bed. Prior to ovulation, the temperature is usually below the normal body temperature. It rises about 0.2°C to 0.4°C or 0.4°F to 0.8°F in response to the increasing levels of progesterone after ovulation. The BBT method is so variable that, if practiced alone, it requires abstinence until the night of the third day of a shift in temperature.
Combining the BBT with the mucus method, abstinence begins when the mucus becomes sticky and moist. Intercourse resumes the night of either the third day of a temperature shift or the fourth day after the last day of sticky, wet mucus, whichever is later. Although this method is more complicated, the efficacy is slightly better, about 2 to 3 failures per 100 woman-years when practiced by experienced couples who follow all the rules.20,21,22 The performance of this method was superior in a comparison of the symptothermal method with various hormone-monitoring devices.23 Similarly, the typical use of this method was better than methods that relied on handheld devices to evaluate ferning in saliva or mucus.23 The failure rate is higher when the method uses only measurement of the BBT, about 8.5%.21
Individual women can be taught to incorporate other signals into their periodic abstinence method. For many women, these additional signs and symptoms can add accuracy. These signals include mittleschmerz, breast tenderness, and changes in cervical position and texture.
 |
Hormone Monitoring
Urinary concentrations of estrone-3-glucuronide and luteinizing hormone (LH) can be measured with disposable test sticks and a handheld monitor. The Persona Monitor indicates fertile days (the first rise in estroneglucuronide) by displaying a red light after the insertion of the test stick, and the light changes to green at the end of the fertile period (4 days after the rise in LH). With a 6-day fertile period, this method was 93.8% effective (a 6.2% pregnancy rate over 1 year), although a criticism of this study concluded that the pregnancy rate is higher.24,25 In an Italian evaluation of several methods (salivary ferning, BBT, salivary glucuronidase, and urinary LH), self-measurement of urinary LH levels was the best method to accurately minimize the number of days of abstinence.26 The Clearplan Easy Fertility
Monitor is an electronic device that also measures urinary LH and estrone-3-glucuronide.27 It is marketed as an aid to achieve pregnancy, not as a method of family planning, and it should be emphasized that it underestimates the window of fertility; the device would have to be used in conjunction with one of the other measures of the fertile period. A study that compared the cervical mucus method with and without this device found a 2% failure rate with the monitor compared with a 12% rate without the monitor.28 The cervical mucus method combined with the Clearplan Monitor is known as the Marquette Method of natural family planning.29
Monitor is an electronic device that also measures urinary LH and estrone-3-glucuronide.27 It is marketed as an aid to achieve pregnancy, not as a method of family planning, and it should be emphasized that it underestimates the window of fertility; the device would have to be used in conjunction with one of the other measures of the fertile period. A study that compared the cervical mucus method with and without this device found a 2% failure rate with the monitor compared with a 12% rate without the monitor.28 The cervical mucus method combined with the Clearplan Monitor is known as the Marquette Method of natural family planning.29
The Standard Days Method
The Standard Days Method was developed by the Institute for Reproductive Health of Georgetown University in Washington, DC.30 This method simply incorporates the avoidance of unprotected intercourse on days 8 through 19 of menstrual cycles that last between 26 and 32 days. CycleBeads, also developed by the Institute for Reproductive Health of Georgetown University, are a string of color-coded beads used with the Standard Days method to monitor cycle days and lengths. Users of this method are advised that efficacy will be reduced even if only one menstrual cycle is out of the 26- to 32-day range, and to abandon the method if two cycles are out of the range.30 The first-year failure rate in worldwide use was 14.1 per 100 woman-years.31 Condom use is recommended during the fertile period, days 8 to 19.



