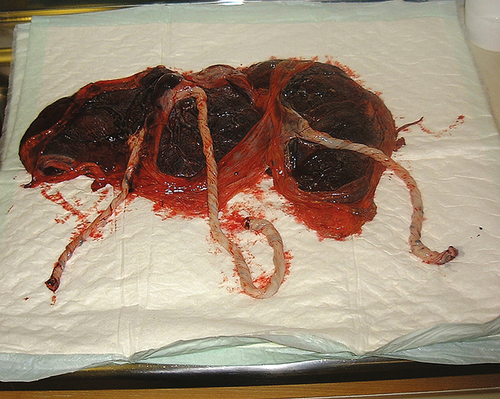
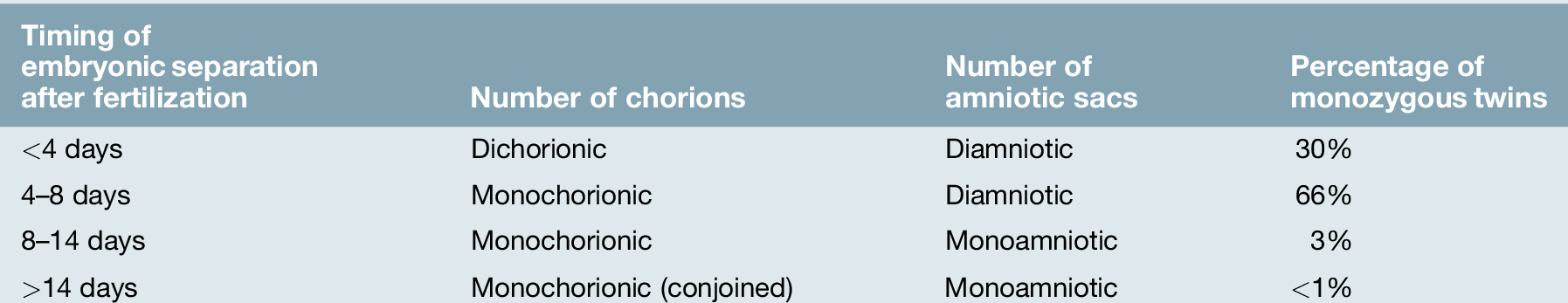
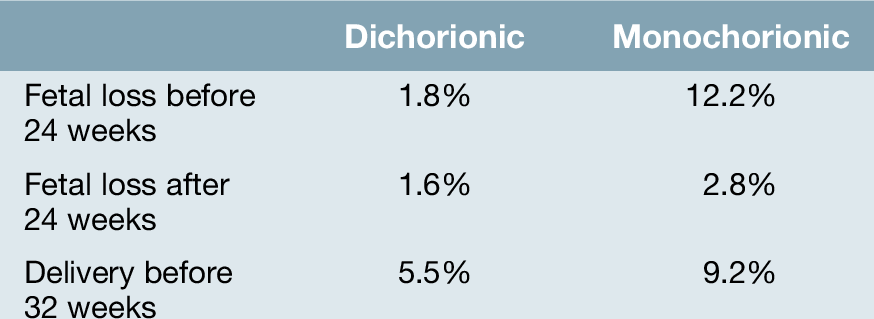
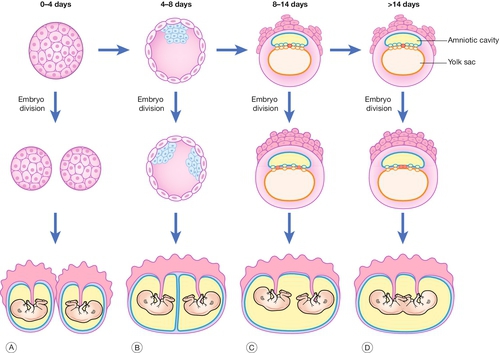
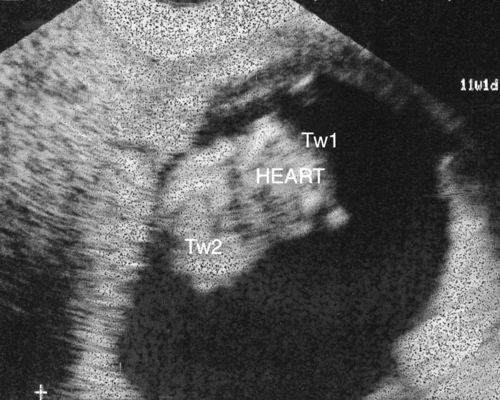
38 The nature of twinning and chorionicity Antenatal problems specific to monochorionic twin pregnancies The natural incidence of twinning has a large geographical variation, ranging from 54/1000 in Nigeria, 12/1000 in the UK, to 4/1000 in Japan. This difference is almost entirely due to variations in the rate of non-identical twins, while the incidence of identical twins remains remarkably constant at around 3/1000. In developed countries, the actual incidence of twin pregnancies is significantly greater than the natural incidence, due to in vitro fertilization and ovulation induction techniques. Around 25% of twin pregnancies, 50–60% of triplet pregnancies, and 75% of quadruplet pregnancies are a result of assisted reproduction techniques. One in 64 pregnancies in the UK is now a twin pregnancy. Overall, the perinatal mortality in twin pregnancies is four to five times higher than for singleton pregnancies, largely because of pre-term delivery, fetal growth restriction, twin-to-twin transfusion syndrome (TTTS), and a slightly increased incidence of congenital malformations. Perinatal mortality rates rise exponentially with fetal number in higher-order pregnancies. The outcome of any multiple pregnancy is also significantly affected by its chorionicity (whether each fetus has its own or shares a placenta) (Fig. 38.1). ‘Zygosity’ refers to whether the twins have developed from a single ovum or from different ova – in other words, whether they are identical or non-identical. ‘Chorionicity’ refers to the number of placentae (Fig. 38.2). Fig. 38.2Diagram of chorionicity. Monozygotic pregnancies may form any of the following combinations depending on the timing of embryo division: (A) dichorionic diamniotic; (B) monochorionic diamniotic; (C) monochorionic monoamniotic; (D) conjoined twins. Dizygotic twins account for approximately 70% of twins. This process occurs when two ova are fertilized and implant separately into the decidua. Each developing embryo will form its own outer chorion (chorionic membrane and placenta) and its own inner amniotic membrane. Dizygotic twin pregnancies are described as dichorionic and diamniotic. Monozygotic twins (30% of twins) are derived from the splitting of a single embryo and the exact configuration of placentation depends on the age of the embryo when the split occurs (Fig. 38.2). A split that occurs at or before the eight-cell stage (3 days post-fertilization) will occur before the outer chorion has differentiated and will therefore give rise to two separate embryos that will each proceed to form their own chorion. These twin pregnancies, like dizygotic twins, will therefore be diamniotic and dichorionic. Embryo splitting at the blastocyst stage (4–8 days post-fertilization) will occur after the chorion has started to differentiate and therefore the fetuses will share an outer chorion (placenta and outer chorionic membrane). This is the more common form of monozygotic twinning. Division of the embryo between 8 and 14 days will result in the inner amniotic cavity and membrane being shared (monochorionic monoamniotic twins). Splitting beyond 14 days following fertilization is extremely rare, giving rise to conjoined twins (Fig. 38.3); Table 38.1. Diagnosed at 12 weeks’ gestation. This is a cross-sectional view through the thoraces of both of the twins. In view of the shared cardiac structures, management includes the option of termination of pregnancy. In monochorionic twins, the shared placental mass inevitably contains a number of vascular anastomoses between the two fetal–placental circulations. The very presence of a shared vascular system dictates that the well-being of each twin is directly dependant on the well-being of the other. The number and nature of these vascular connections places monochorionic twins at risk of specific complications and an increased perinatal loss and morbidity rate. Chorionicity determination is therefore essential to allow risk stratification (Table 38.2), and has key implications for prenatal diagnosis and antenatal monitoring. It is most easily determined in the first or early second trimester by ultrasound: Fig. 38.4(A) Dichorionic twins – lambda sign. (B) Monochorionic twins – no lambda sign. The two amniotic membranes form a ‘T-sign’ as they join the placenta. The incidence of all maternal complications is increased in multiple pregnancy. The increased placental mass, and therefore increased maternal circulating human chorionic gonadotrophin (hCG) concentration, is associated with an increased and earlier incidence of hyperemesis. There is an increase in the incidence of anaemia associated with multiple pregnancy, which is not completely explained by a haemodilutional effect of the increased plasma volume. The need for iron and folate supplementation should be assessed early in the pregnancy with a full blood count performed at 20–24 weeks’ gestation, in addition to the usual antenatal anaemia screen performed at 28 weeks in all pregnancies.
Multiple pregnancy
Introduction
The nature of twinning and chorionicity
Dizygotic twinning (non-identical)
Monozygotic twinning (identical)
![]() widely separated first-trimester sacs or separate placentae are dichorionic
widely separated first-trimester sacs or separate placentae are dichorionic
![]() those with a ‘lambda’ or ‘twin-peak’ sign at the membrane insertion are dichorionic (Fig. 38.4A)
those with a ‘lambda’ or ‘twin-peak’ sign at the membrane insertion are dichorionic (Fig. 38.4A)
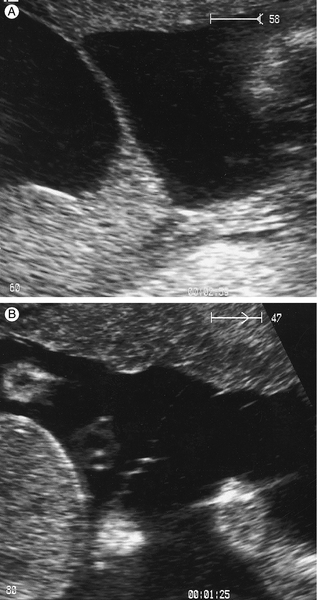
![]() those with a ‘T’ sign at the membrane insertion are monochorionic (Fig. 38.4B)
those with a ‘T’ sign at the membrane insertion are monochorionic (Fig. 38.4B)
![]() different-sex fetuses are always dichorionic (and dizygous).
different-sex fetuses are always dichorionic (and dizygous).
Maternal complications
Hyperemesis
Anaemia
Pre-eclampsia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree