KEY POINTS
• Prematurity is the greatest risk factor for multiple-gestation pregnancies.
• Monochorionic placentation creates additional risk for either fetus and requires careful surveillance.
• Higher-order multiple gestations also pose significant medical risks for maternal morbidity.
BACKGROUND
Definition
• Incidence with spontaneous ovulation
• Twin gestation occurs in 15 out of 1000 pregnancies.
 Monozygotic twin gestation is constant at 3 to 5 in 1000 births.
Monozygotic twin gestation is constant at 3 to 5 in 1000 births.
 Dizygotic twin incidence varies by population group.
Dizygotic twin incidence varies by population group.
• Triplet gestation occurs in 3.7 out of 10,000 pregnancies.
• The frequency of triplets is influenced by the same factors as is that of twins.
• Higher-order multiple gestation:
 Incidence is less than 5 out of 1,000,000 pregnancies.
Incidence is less than 5 out of 1,000,000 pregnancies.
 Live birth rate is significantly lower.
Live birth rate is significantly lower.
• Incidence in United States
• Vital statistics data often do accurately differentiate spontaneous conceptions from assisted reproductive technology (ART).
• Twin gestation:
 Thirty-three out of 1000 births are twins (1).
Thirty-three out of 1000 births are twins (1).
 There has been a 76% increase in incidence since 1980 (1,2).
There has been a 76% increase in incidence since 1980 (1,2).
 Thirty-three percent of twins result from fertility therapies (2,3).
Thirty-three percent of twins result from fertility therapies (2,3).
• Triplet gestation and higher-order multiples (triplets/+):
 Triplets and higher-order multiples accounted for 13.8 out of 10,000 pregnancies in 2010.
Triplets and higher-order multiples accounted for 13.8 out of 10,000 pregnancies in 2010.
 During the 1980s, the incidence rose greater than 400%. However, since 1995, the incidence has dropped nearly 30% (1,4).
During the 1980s, the incidence rose greater than 400%. However, since 1995, the incidence has dropped nearly 30% (1,4).
 Only 7% to 18% of triplets occur spontaneously.
Only 7% to 18% of triplets occur spontaneously.
 Less than 7% of higher-order multiples result from spontaneous ovulation (5).
Less than 7% of higher-order multiples result from spontaneous ovulation (5).
• The gradual increase in maternal age over the past 20 years also has had some minor effect on the frequency of multiple-gestation birth.
Pathophysiology
• Zygosity and placentation
• The outcome of multiple gestations, especially twins, correlates well with placentation and, to a lesser extent, zygosity.
• The outcome for triplets and higher-order multiples is more influenced by the degree of prematurity.
• Patterns of placental relationships remain important to siblings in triplets and higher-order multiples due to the possible combinations of zygosity.
• Zygosity
• Monozygotic twins
 There is a fixed incidence of 30% of monozygosity in spontaneous twins.
There is a fixed incidence of 30% of monozygosity in spontaneous twins.
 Monozygosity can occur in ART twins, especially after intracytoplasmic sperm injection.
Monozygosity can occur in ART twins, especially after intracytoplasmic sperm injection.
• Dizygotic twins
 The rate of dizygotic twins is influenced by
The rate of dizygotic twins is influenced by
– Maternal age
– Parity
– Race and ethnicity
 There is a 70% incidence of dizygosity in spontaneous twins.
There is a 70% incidence of dizygosity in spontaneous twins.
 There is a greater than 95% incidence of dizygosity in ART twins and higher-order multiples.
There is a greater than 95% incidence of dizygosity in ART twins and higher-order multiples.
• Placentation
• Monochorionic placenta
 Derived from single embryo, identical
Derived from single embryo, identical
 Monochorionic/diamniotic
Monochorionic/diamniotic
– There is a 68% incidence of monochorionic/diamniotic placentation in monozygotic twins.
– Excess preterm birth and perinatal mortality are observed with a single placenta.
– The perinatal fetal death rate is as high as 25% (6).
 Monochorionic/monoamniotic
Monochorionic/monoamniotic
– In monozygotic twins, the incidence of monochorionic/monoamniotic placentation is less than 2%.
– Up to 50% perinatal mortality is reported due to cord entanglement.
• Dichorionic/diamniotic placenta
 Dichorionic placentation may occur in either monozygotic or dizygotic twins and higher-order multiples.
Dichorionic placentation may occur in either monozygotic or dizygotic twins and higher-order multiples.
 Dichorionic placentation occurs in monozygotic twins that divide earlier than 3 days after fertilization.
Dichorionic placentation occurs in monozygotic twins that divide earlier than 3 days after fertilization.
 There is lower perinatal risk than with monochorionic placentation.
There is lower perinatal risk than with monochorionic placentation.
• Evaluation of the placenta may help determine if same-sex twins are identical.
 Placentation should always be documented
Placentation should always be documented
– During ultrasound studies
– In the delivery room
– In the lab, if necessary
 Same-sex twins with separate placentas have a monozygotic/dizygotic risk of 1:5 (Table 34-1).
Same-sex twins with separate placentas have a monozygotic/dizygotic risk of 1:5 (Table 34-1).
Table 34-1 The Frequency of Placentation in Twin Pregnancies
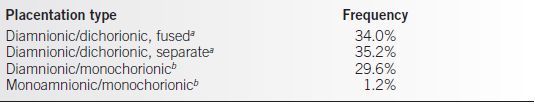
aMay be mono- or dizygotic.
bMonozygotic only.
Source: Hollenbach KA, Hickok DE. Epidemiology and diagnosis of twin gestation.
Clin Obstet Gynecol. 1990;33:3–9.
Table 34-2 Perinatal Outcome for Multiple-Gestation Pregnancy
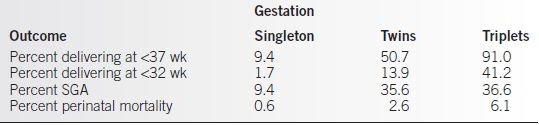
SGA, small for gestational age.
Source: Keith LG, Cervantes A, Mazela J, et al. Multiple births and preterm delivery. Prenat Neonat Med. 1998;3:125–129; Mathews MS, MacDorman MF. Infant mortality statistics from the 2009 period linked birth/infant death data set. National Vital Statistics Reports. 2013;61(8).
Epidemiology
• Of all live births, 3.3% are from multiple gestations.
• Just more than 58% of multiples are also low birth weight.
• Thirteen percent of all preterm births are multiples.
• Over 5% of all infants less than 1500 g are multiples (1).
• The average cost for twin pregnancy and delivery is almost $40,000.
• The average cost for triplets and higher-order multiple pregnancy and delivery exceeds $100,000 per pregnancy (4,7).
• Prematurity is the greatest risk for multiple-gestation pregnancies (Table 34-2). There is a significant increase (vs. singletons) in
• Neonatal intensive care unit admissions
• Low birth weight deliveries (8)
• Perinatal deaths (8)
EVALUATION
Ultrasound Surveillance
Chorionicity
• Chorionicity is best determined by ultrasound in the first trimester or early second trimester (Fig. 34-1).
Monochorionicity
• Single placental bed
• Thin amniotic membrane
• At insertion of amnion into chorion, no increase in thickness
Dichorionicity
• Two separate placental beds or fused placentas with thickened amnion.
• Chorion separates leaves of amnion at insertion in placental bed (twin peak sign).
Fetal Growth
• Multiple-gestation fetuses have a high rate of growth restriction.
• Serial sonographic estimated fetal weights (EFW) are the only method to assure that fetal growth is within normal limits. Ultrasound references for expected twin growth are available.
• Ultrasound studies should be done every 3 to 6 weeks.
• EFW with less than 25% differences are concordant.
• EFW with greater than 25% difference are discordant and warrant more careful attention.
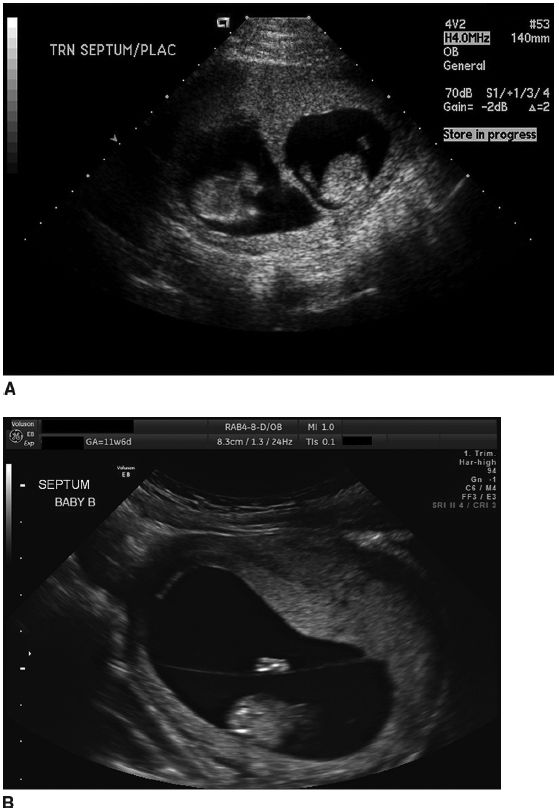
Figure 34-1. A: Dichorionic, diamniotic placenta. Note chorion present between leaves of amnion at placenta insertion. B: Monochorionic, diamniotic placenta. Note amnion appears thin at insertion without chorion present.
Cervical Length
• Endovaginal ultrasound measurement of the cervix at 22 to 28 weeks may aid in selecting patients at high risk of preterm delivery (9–11).
• Normal cervix with length greater than 3.5 cm is very reassuring.
• Cervical length less than 2.5 cm in an asymptomatic patient may indicate increased risk of spontaneous preterm birth and warrant careful surveillance.
• Cervical length less than 2.5 cm and abnormal examination or symptoms of preterm labor mandate immediate evaluation.
Amniotic Fluid Volume
• The amniotic fluid index (AFI) is the standard method of measuring amniotic fluid volume in singleton pregnancies.
• Reduced AFI may represent chronic placental dysfunction.
• The amniotic fluid volume in twins may be assessed by two different methods:
• General assessment can be done using the same method as a singleton pregnancy (12).
• A subjective assessment of fluid volume of each pregnancy can be made with a minimal objective measurement of a 2-cm vertical pocket in each gestational sac beyond 20 weeks’ gestational age.
• Amniotic fluid volume assessment should be performed at every ultrasound study and is recommended every 2 weeks beyond 32 weeks’ gestational age.
DIAGNOSIS
Antepartum Surveillance
• In at-risk singleton gestations, antepartum surveillance reduces the risk of stillbirth (13).
• Some centers routinely perform antepartum testing in all multiple gestations.
• An alternative option is to perform antepartum testing in twins only if discordance or other risk factors exist.
• All higher-order multiples require some form of fetal surveillance.
Methods of Surveillance for Fetal Well-Being
• Nonstress tests (NSTs) are most the common tests used. NST is usually recommended twice weekly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


