Multiple Births
James M. Greenberg
Since antiquity, multiple births have fascinated mankind. Twins, triplets, and higher order births attract public attention and bemusement that often belies appreciation of specific management challenges not associated with singleton pregnancies. In addition, certain complications of pregnancy, such as preterm birth, occur more frequently with higher order gestations. Optimal management requires knowledge of issues associated with multifetal gestation during pregnancy, at delivery, and into the neonatal period.
Multifetal gestations are classified on the basis of zygosity and chorionicity.1Dizygotic twins arise from independent fertilization of separate ova. Typically, two placentas form with distinct chorionic and amniotic membranes separating each fetus. Monozygotic twins develop from a single fertilized ovum that subsequently divides at or before the blastocyst stage of embryogenesis. The factors promoting fission of the conceptus are poorly understood. The timing of embryonic division determines whether the monozygotic twins will be separated by amnion and chorion (dichorionic, diamniotic), amnion only (monochorionic, diamniotic), or not separated (monoamniotic, monochorionic). Dizygotic twins account for about two thirds of spontaneous twin births and are almost always dichorionic, diamniotic. Monochorionic twins share a single placenta with a shared circulation. This developmental phenomenon carries a significant mortality risk and may lead to complications such as twin-twin transfusion syndrome (discussed under “Complications” in this chapter).2 Higher order multiples can be a combination of monozygotic and dizygotic gestations. Monozygotic triplets arising from a single fertilized ovum are extremely rare.
EPIDEMIOLOGY
The twin birth rate in 2005 was 32.2 per 1000 births, a 42% increase from 1990, and up 70% since 1980.3 The incidence in 2005 was unchanged from 2004. It is not clear whether this represents a true stabilization of a persistent upward trend over the previous 25 years. The triplet+ birth rate (the number of triplet, quadruplet, and higher order multiple births) increased dramatically during the 1990s, peaking at 193.5 per 100,000 births in 1998. Since then, the rate has slowly declined to 161.8 per 100,000 births in 2005. However, this rate is still more than fourfold higher than in 1981.
The increase in twin and higher order multiple births has occurred in conjunction with increases in maternal age and the use of assisted reproductive technologies, ovulation-inducing agents, and artificial insemination. It is noteworthy to consider that nearly half of very-low-birth-weight multiples hospitalized in newborn intensive care units may involve pregnancies assisted by infertility treatments.4 In the late 1990s, the American Society of Reproductive Medicine recommended reducing the number of embryos transferred per cycle. This may explain the decline in triplet+ births since that time.5 The remarkable increase in multiple births is recognized as a significant public health concern because of the associated mortality and morbidity risks discussed next.
COMPLICATIONS
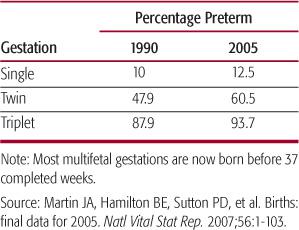
Multifetal gestations exhibit certain complications also encountered during a singleton gestation. Of these, the single most significant is preterm delivery (see Table 46-1). Once delivered, the preterm product of a multifetal gestation is at risk of experiencing any or all known complications of prematurity, including respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, growth failure, and developmental delay. Prior to delivery, multiples are more likely to have delayed growth, especially during the third trimester. Breech or other abnormal presentations are more likely and account for a higher potential for cesarean delivery. Other described complications include polyhydramnios, birth depression, and congenital anomalies, including those related to compression or constraint in utero.6
Additional, unique complications can occur in monochorionic twinning. These gestations share a common, fused placenta that typically includes vascular connections between each fetus. When an artery from one twin is drained by a direct venous connection from the other, twin-twin transfusion syndrome may develop. Although intertwin vascular connections in monochorionic twins are nearly universal, the incidence of symptomatic twin-twin transfusion syndrome is much lower, with estimates ranging from 4% to 35% of monochorionic twin gestations.7 The typical presentation includes size discordance, with blood transfusing from the high-pressure arterial circulation of the “donor” twin to the low-pressure venous circulation of the “recipient” twin. The natural history of twin-twin transfusion syndrome includes progressive heart failure in each twin, hydrops, and intrauterine fetal demise. The donor twin may develop significant oligohydramnios and constraint of movement within the amnion: the so-called stuck twin phenomenon. The recipient twin usually develops polyhydramnios.8 Treatments for twin-twin transfusion syndrome include repetitive amniocentesis to reduce the volume of amniotic fluid surrounding the recipient twin. In utero laser ablation of intertwin arteriovenous connections has also been performed with some success9 (see Chapter 40). Even in the absence of twin-twin transfusion syndrome, disproportionate placental circulation may cause discordant growth. Cord entanglement in monoamniotic, monochorionic twins represents an additional risk for fetal compromise or demise. Conjoined twinning occurs as a consequence of incomplete fission in monoamniotic, monochorionic twins approximately 14 days after fertilization.10 They are classified according to the site of attachment. Congenital malformation of major organs is typical. Long-term survival is a function of potential for surgical separation.
Table 46-1. Preterm Birth Rates Increased during the Period from 1990 to 2005
MANAGEMENT
The cornerstone of delivery room management for multiple births is anticipation. Most multifetal gestation pregnancies are identified long before delivery, providing time to ensure that qualified personnel and equipment are available to manage each newborn. Historical information such as discordancy may alert delivery room attendants to the potential for clinical instability after delivery. An easy vertex delivery does not necessarily predict uneventful delivery of subsequent infants. Malpresentation, placental abruption, or unexpected cord prolapse or compression may require emergency cesarean delivery and resuscitation. After delivery, multiples should be carefully screened for congenital malformations. Many parents inquire about zygosity. Twins of different gender or with distinct placentas and associated membranes are dizygotic. Same-sex multiples with fused placentas are more challenging. Pathologic examination of the fused placenta and blood testing can be useful. Absolute verification of zygosity requires analysis of DNA derived from somatic tissue.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


