FIGURE 30-1 Acute Monteggia fracture dislocation. A: Lateral radiograph of the forearm demonstrates a short oblique middiaphyseal ulna fracture. B: AP forearm radiograph including the elbow and wrist demonstrates an associated anterior radial head dislocation.
Unfortunately, despite the increased awareness and understanding of Monteggia fracture dislocations, the initial diagnosis is often missed, resulting in late presentation, challenging surgical reconstruction, and suboptimal outcomes. A number of published reports have documented a relatively high incidence of missed diagnoses.5,10,11 Therefore, a high index of suspicion is paramount, and the adjacent joints should be carefully inspected with any single bone fracture of the forearm.
Normally, the longitudinal axis of the radius should bisect the capitellar ossification center on all radiographic views.12,13 Cases of presumed “isolated” radial head dislocations must be scrutinized for abnormal ulnar bowing or plastic deformation; indeed >0.1-mm deviation from a straight ulnar border should alert the treating provider to a possible occult ulnar injury (Figure 30-2).14–18 There are some situations where plain radiographs are concerning but equivocal; in these cases, fluoroscopic imaging and/or advanced imaging in the form of magnetic resonance imaging (MRI) or ultrasound may be useful to confirm or rule out a congruent radiocapitellar and proximal radioulnar joint reduction.
While congenital radial head dislocations may occasionally present as acute injuries, the presence of a hypoplastic capitellum and convex radial head will usually confirm the diagnosis.19 Furthermore, it is important to note that statistically, most traumatic Monteggia lesions result in anterior radial head dislocation, whereas most (but not all) congenital radial head dislocations are posterior.20–22
An understanding of the pathoanatomy of Monteggia fracture dislocations is critical in providing appropriate treatment. In the majority of cases, the annular and quadrate ligaments are disrupted at the PRUJ; however, much of the interosseous membrane between the radius and ulna remains intact, as does the triangular fibrocartilage complex. Anatomic reduction of the ulna, therefore, will often restore PRUJ and radiocapitellar joint congruity. For this reason, treatment is predicated on the nature of the ulna fracture. In addition, the biceps, anconeus, and long forearm flexors exert deforming forces on the proximal radius and ulna, contributing to radial head dislocation, ulnar shortening, and apex radial angulation. Reversing or counteracting these forces is important during fracture manipulation and closed treatment.
Historically, the Bado classification, based upon the direction of the radial head dislocation and apex of the associated ulnar fracture, has been utilized to describe these injuries (Figure 30-3).2 This classification scheme may aid both in describing the pattern of injury and guiding closed fracture care.
Bado type I injuries refer to anterior dislocation and angulation and are the most common patterns, representing approximately 70% to 75% of all injuries. The mechanism of injury is thought to be due to a hyperextension injury combined with forearm pronation. Reduction, therefore, involves longitudinal traction, supination, posteriorly directed pressure over the radial head, and flexion of the elbow to 110 or 120 degrees to minimize the deforming effect of the biceps.
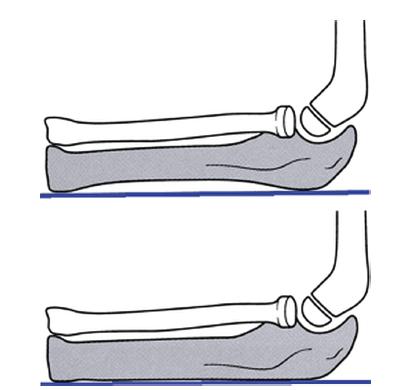
FIGURE 30-2 In cases of “isolated” radial head dislocation, the ulna should be evaluated for deviation from its normally straight dorsal border. Deviation from a straight line drawn along the ulnar border should alert the examiner of a prior ulnar fracture and Monteggia lesion. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
Bado type II injuries refer to posterior radial head dislocations with apex dorsal ulnar fractures. While common in adults, these injuries are relatively rare in children, accounting for 3% to 6% of pediatric Monteggia lesions. Thought to be caused by an axial load on a partially flexed elbow or direct blow to the proximal supinated forearm, the reduction maneuver involves longitudinal traction with the elbow flexed combined with an anteriorly directed force over the radial head.2,7,23,24 There is a propensity for instability with the elbow flexed.
Bado type III injuries refer to lateral dislocations and varus fractures of the proximal ulna. Representing the second most common pattern in children, these too result from hyperextension and pronation with varus stress.25,26 Among the various patterns, it is the Bado type III lesion that is most commonly associated with PIN palsies.27–29 Combined longitudinal traction, elbow extension, and valgus stress will serve to reduce the deformity. The need for open reduction is common.25–28,30,31
Bado type IV lesions refer to radial head dislocations with fractures of both the radius and ulna. The fractures are typically mid-diaphyseal, with the radial fracture more distal than the ulnar fracture.32 With similar mechanisms of injury as Bado type I injuries, these tend to be higher energy in nature and follow similar treatment principles.
Letts et al.33 have described an alternative classification scheme based upon the pattern of ulnar fracture (Figure 30-4). This classification is helpful in surgical decision making.
The clinical presentation of missed or chronic Monteggia fracture dislocations is quite varied. Many patients will present weeks after injury, when during the course of cast treatment for an “isolated” ulna fracture, the radial head dislocation is noticed (see Sidebar). While distressing, the opportunity to effectuate meaningful restoration of anatomy and functional potential remains great, as no secondary joint changes have occurred. Other patients will present months to years after injury, either with incidental radiographic diagnosis or for evaluation of new pain, noticeable loss of elbow flexion or forearm rotation, or with apparent deformity (e.g., a palpable radial head in the antecubital fossa or posterolateral elbow, progressive cubitus valgus). For many patients, there will be objective, but often minimally symptomatic, functional loss. Radiographs again confirm the diagnosis and guide treatment.
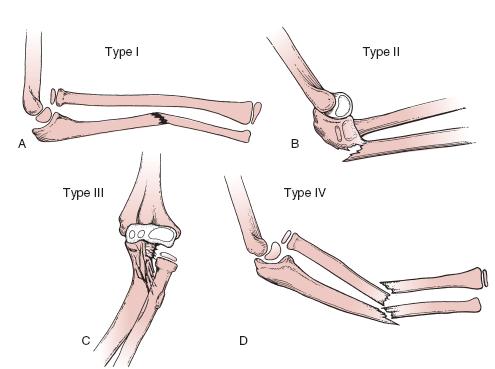
FIGURE 30-3 Schematic diagram of the Bado classification, based upon the direction of radial head dislocation and fracture angulation. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
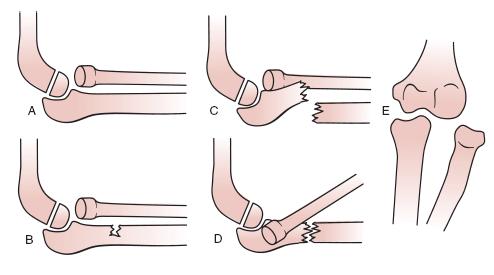
FIGURE 30-4 Letts classification of Monteggia lesions, based upon the ulna fracture pattern. (From Beaty JH, Kasser JR. Rockwood & Wilkins Fractures in Children. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
Surgical Indications
Set it and forget it.
—Ron Popeil
While all acute Monteggia fracture dislocations merit formal reduction, there are different methods by which this may be achieved. Closed reduction and cast immobilization alone has been advocated by many and is effective for plastic deformation and incomplete fractures, provided they are recognized acutely. However, simple closed reduction alone has a number of disadvantages. First, there is a high risk of recurrent instability due to loss of reduction with cast immobilization alone (Figure 30-5). This is further compounded by the challenges in serial radiographic evaluation of the quality of reduction while the limb is casted, particularly for Bado type III injuries, which require AP views to assess for lateral displacement of the radial head. Furthermore, effective immobilization of displaced Monteggia lesions often requires positioning the acutely injured, swollen limb in extreme positions. For the common Bado type I injuries, for example, hyperflexion is recommended, which may lead to issues with skin integrity and neurovascular compromise. For these reasons, among others, we advocate surgical reduction and stabilization of all acute Monteggia fracture dislocations with complete ulnar fractures.28,34
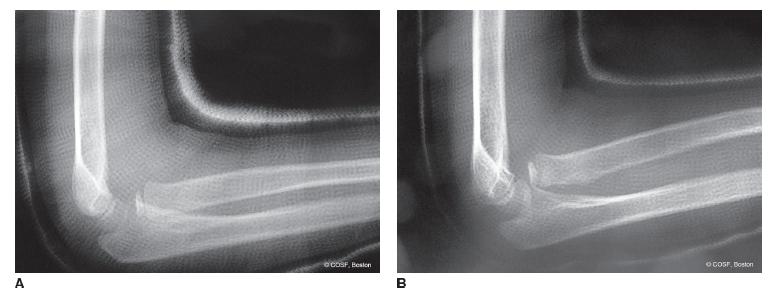
FIGURE 30-5 Loss of reduction with cast immobilization. A: Initial postreduction lateral radiograph of a Bado 1 Monteggia lesion. B: Loss of reduction is seen in cast. Notice the initial lateral was not perfectly reduced.
Chronic Monteggia lesions present a host of different challenges, due to the complexity of surgical steps needed to simultaneously reestablish a stable and mobile PRUJ and potential complications of operative treatment. This is further clouded by the paucity of long-term information regarding the natural history of unreduced Monteggia fracture dislocations.35–37 It is known, however, that some patients with missed Monteggia lesions will develop pain, functionally limited loss of elbow motion, cubitus valgus, ulnar or posterior interosseous neuropathy, and/or arthrosis.14,20,22,26,38–48 We believe that symptomatic patients with chronic Monteggia lesions are candidates for surgical reconstruction.
More important, perhaps, are the contraindications to chronic reconstruction. While some have discussed time from injury (<3 years) or patient age (<12 years of age) as discriminating factors, more important is the morphology of the radial head and capitellum.11,49–51 Patients with radial head enlargement, loss of capitellar convexity, loss of radial head concavity, and/or cartilage loss and arthrosis may not have reducible joints and are not candidates for reconstruction. These are similar to the principles that guide congenital radial head dislocations.
SURGICAL PROCEDURES
Adhering to the principle that restoration of ulnar length and alignment will help obtain and maintain radiocapitellar joint reduction, the choice of surgery will depend upon the chronicity and pattern of ulnar injury.
In acute fractures, incomplete ulnar fractures (plastic deformation and greenstick injuries) have some inherent stability and are length stable; therefore, closed reduction and appropriate cast immobilization are performed. In complete transverse or short oblique fractures, closed reduction and intramedullary (IM) fixation will maintain alignment and preserve length without the additional concerns of open surgery or retained implants. In patients with long oblique or comminuted fractures, IM fixation is often insufficient; open reduction and rigid internal fixation using plate and screw constructs, even in very young patients, are performed instead.
Chronic Monteggia fractures present different challenges. In addition to restoring ulnar length and alignment, the long-standing nature of the radial head dislocation adds further complexity, including scar and soft tissue interposition within the PRUJ, potential for secondary deformity of the capitellum and radial head, and an often deficient annular ligament.
Controversy persists regarding the optimal approach to reconstruction for chronic Monteggia lesions, and to date the “correct” answer is unknown. Areas of continued debate and discussion center around: (1) whether gradual or single-stage correction of the ulnar malunion should be performed; (2) the way in which the ulna should be osteotomized (oblique, transverse, opening wedge); and (3) whether the annular ligament should be discarded, repaired, or reconstructed.8,20,45,52–62 Clinical data exist to support various reconstructive strategies, and perhaps the most important decision-making factor is the experience and abilities of the treating surgeon. Experienced chronic Monteggia reconstruction surgeons throughout the world consistently feature ulnar osteotomy and thorough joint debridement as principal components of their treatment plans. Our preference is to perform an open ulnar osteotomy with plate and screw fixation, open reduction of the radiocapitellar joint with complete PRUJ debridement, and formal annular ligament repair or reconstruction.
 Closed Reduction Incomplete/Plastic Deformation
Closed Reduction Incomplete/Plastic Deformation
In acute lesions, the method of treatment is determined by the pattern of ulnar fracture. In patients with plastic deformation, proximal varus buckle, or greenstick fracture of the ulna, closed reduction under general anesthesia is recommended. In these situations, closed reduction of the ulna is typically performed with a combination of longitudinal traction, forearm rotation, and direct pressure applied to the apex of the fracture. The radiocapitellar joint usually reduces spontaneously with this maneuver. The need for significant force applied to the radial head should raise suspicion for interposed soft tissue blocking radiocapitellar joint reduction. In the most common type I lesions, for example, the radial head is anteriorly dislocated, and the ulna has apexvolar angulation. Correction of the ulnar deformity followed by posteriorly directed pressure on the radial head, elbow flexion, and forearm supination is usually performed. Typically, the ulna fracture and radiocapitellar joint are stable after reduction of plastic deformation or incomplete fractures. This is tested manually and under fluoroscopy. A wellmolded, bivalved above-elbow cast is then applied for 4 to 6 weeks. After radiographic and clinical healing is confirmed, supervised range-of-motion exercises may be initiated.
 IM Fixation of Short Oblique or Transverse Ulna Fractures
IM Fixation of Short Oblique or Transverse Ulna Fractures
In patients with complete transverse or short oblique fractures of the ulna, closed reduction alone can result in loss of reduction in a cast. Therefore, closed reduction and IM fixation of the ulna are recommended to facilitate maintenance of ulnar alignment and radiocapitellar reduction (Figure 30-6). In these cases, an age- and size-appropriate stainless steel K-wire or flexible titanium nail (Synthes, West Chester, PA) is selected. K-wires have the advantage of being inexpensive, universally available, and, due to their stainless steel composition and straight tip, allow for easy removal in the office without need for analgesia or anesthesia. K-wires, however, can be too short to provide adequate fixation in older children with longer forearms.
Via a small longitudinal split in the triceps tendon overlying the olecranon process, the K-wire or flexible titanium nail is inserted into the IM canal of the ulna and advanced in an antegrade fashion to the fracture site. The ulnar fracture is closed reduced, and the nail is subsequently advanced into the IM canal of the distal fracture fragment, allowing for restoration of both ulnar length and alignment. During ulnar reduction and fixation, closed reduction is performed of the radiocapitellar dislocation. Intraoperative fluoroscopy is utilized to confirm appropriate ulnar and radiocapitellar reduction, as well as intraosseous placement of the IM device. Given the rapid healing of the ulnar fracture, particularly with closed reduction, our preference is to bend and cut the IM nail outside the skin to facilitate subsequent removal. An above-elbow, bivalved cast is then applied with the elbow in 90 degrees flexion and the forearm in supination, which confers additional stability to the radiocapitellar articulation.
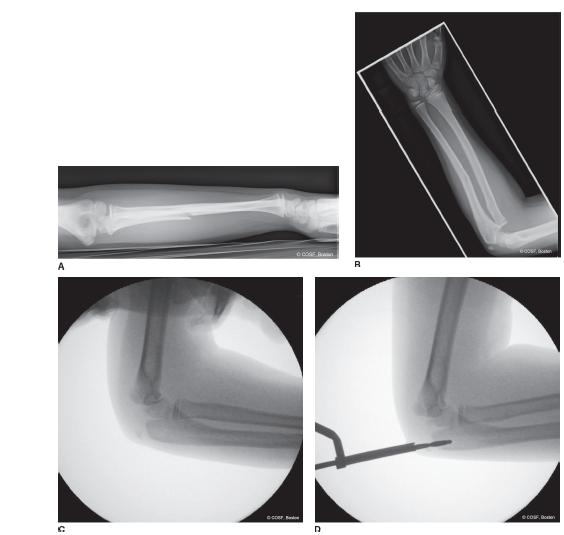
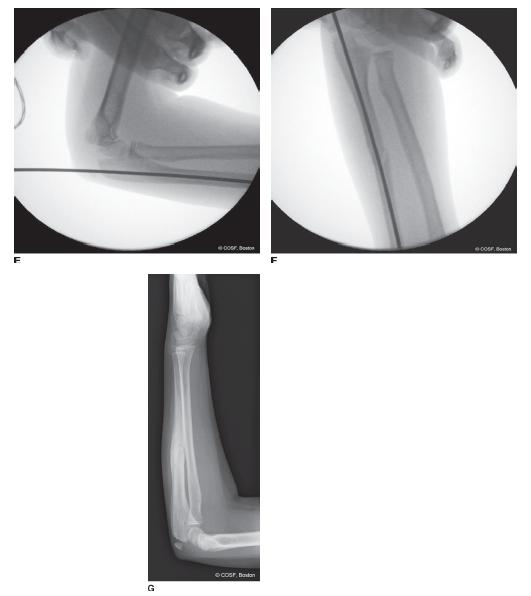
FIGURE 30-6 IM fixation of an acute Bado 1 Monteggia fracture dislocation in a 7-year-old female. A, B: The injury radiographs demonstrate a short oblique ulna fracture with an anteriorly dislocated radial head. C: Intraoperatively, closed reduction is performed. D: A cortical entry site is created in the olecranon. E: A smooth K-wire is passed down the ulnar canal, stabilizing the fracture and joint reduction. F: Reduction is stable with elbow extension. G: Radiograph taken 3 months post-operatively demonstrates bony healing and anatomic joint reduction.
 Open Reduction and Internal Fixation (ORIF)of Long Oblique or Comminuted Ulnar Fractures
Open Reduction and Internal Fixation (ORIF)of Long Oblique or Comminuted Ulnar Fractures
Long oblique or comminuted ulnar fractures cannot be adequately stabilized with IM techniques. While passage of the IM rod is straightforward, the fracture pattern does not allow for adequate maintenance of alignment or length. In these cases, open reduction and internal fixation utilizing plate and screw constructs are necessary (Figure 30-7). Through a longitudinal incision based on the subcutaneous border of the ulna and centered on the fracture site, reduction is performed, and double-stacked one-third tubular or small-fragment dynamic compression plates (Synthes, West Chester, PA) are applied in the standard fashion. In our experience, four to six cortices of fixation proximal and distal to the fracture provide adequate stability in pediatric patients. Radiocapitellar joint congruity is again achieved during reduction and fixation of the ulna fracture, typically with closed manipulation alone. If closed reduction of the radiocapitellar joint is unattainable, an open reduction may be facilitated by extending the ulnar incision proximally over the posterolateral aspect of the elbow. After stable reduction of the radial head (closed or less commonly open), the periosteum is repaired over the fracture site and implant. Limited prophylactic dorsal and volar forearm fasciotomies are performed to lessen the risk of postoperative compartment syndrome. A bivalved long-arm cast in forearm supination is applied.

FIGURE 30-7 ORIF of Monteggia lesion in a 4-year-old male associated with a comminuted ulna fracture. A, B: Injury radiographs demonstrating the dislocated radial head and ulnar fracture pattern. C, D: Radiographs taken 3 months postoperatively, demonstrating a healed fracture and stable joint alignment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


