Restoring the native anatomy of the anterior and posterior horn attachment sites, while providing sufficient fixation, is central to the success of meniscal transplantation. A small stump of remaining meniscal tissue can frequently be used to identify the horn insertion sites. Attachment options include suture-only fixation through transosseous tunnels, bone plugs with horn attachments, or the bone slot technique containing both the anterior and posterior horns. There is still debate in the literature regarding which should be considered the gold standard of fixation. Some authors44,63 advocate suture-only fixation without attached bone; however, most cadaveric studies demonstrate superior results with meniscal horn bone plug fixation.32,35,36,64 This is further supported in the clinical setting, as Rodeo8 found an 88% success rate with bone plug fixation compared to a 47% success rate using the suture-only technique.
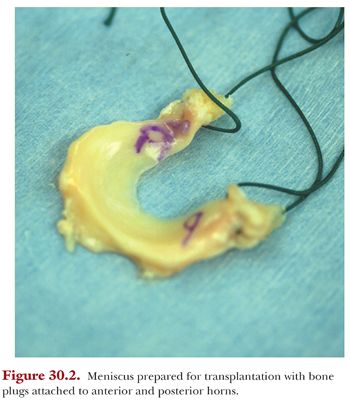
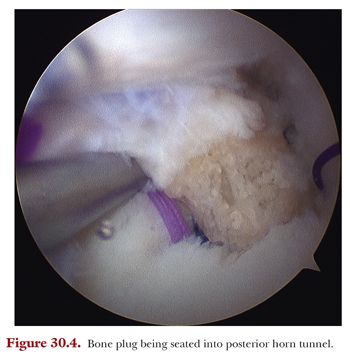
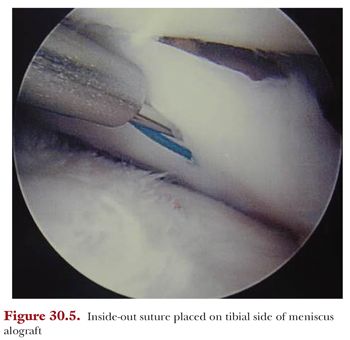
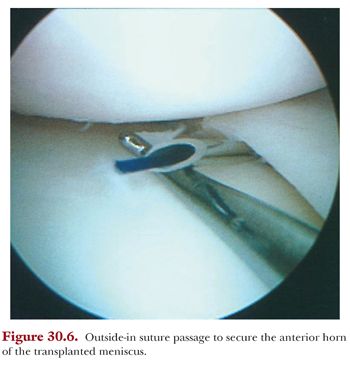
For a medial MAT, we recommend using 9-mm diameter bone plugs for both the anterior and posterior horns (Fig. 30.2). The tunnel for the posterior horn bone plug can be drilled using an ACL or posterior cruciate ligament (PCL) guide, whereas the anterior horn bone plug can be drilled antegrade using an enlarged arthroscopic portal (Fig. 30.3). The meniscal allograft can then be shuttled through the same small medial arthrotomy (enlarged anterior portal). In order to facilitate passage, a small amount of bone should be shaved from the medial tibial spine and medial femoral condyle. An arthroscopic probe can be used to temporarily retract the PCL so the graft can be placed posteriorly (Fig. 30.4). A long meniscal repair needle with attached suture should be passed through the posterior horn, then the posteromedial capsule, and retrieved out an accessory posteromedial incision. This suture is used to pull the graft into the joint and can be later employed for meniscal suturing. In the rare instance where the medial compartment is excessively tight and there is still difficulty with graft insertion, a partial release of the deep medial collateral ligament (MCL) can be performed. Once the bone plugs are appropriately docked in their tunnels, the sutures attached to the bone plugs are tied together over a bone bridge on the anterior tibia. Vertical mattress sutures are then used for circumferential repair of the meniscal allograft to the surrounding capsule, as this has shown superior repair strength compared to absorbable meniscal fixation devices (Fig. 30.5).65,66 An inside-out technique with nonabsorbable suture is used for the posterior horn around to the mid-body, whereas the anterior portion can be repaired using an outside-in approach or under direct visualization using the small anterior incision (Fig. 30.6).

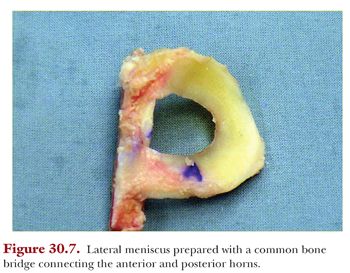
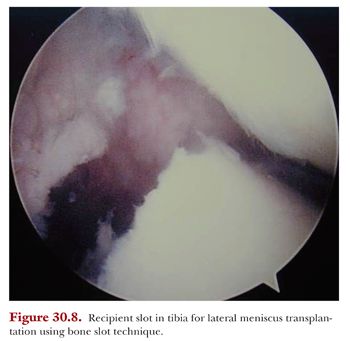
When performing a lateral MAT, we recommend using either individual bone plugs or the bone slot technique (Fig. 30.7). If the latter is employed, a trough in the recipient tibia is made before the graft is shuttled through a small lateral arthrotomy (Fig. 30.8). Generally, arthroscopic burrs are used to create the trough, and care must be taken to remain central while not causing damage to the ACL. Supplemental suture fixation through drill holes in the bone slot can be used to augment attachment, but typically, the graft is stable with an appropriate interference fit. The meniscus is then circumferentially repaired to the capsule as described earlier for the medial side.
Certain considerations must be taken into account when performing concomitant procedures in association with MAT. If ACL reconstruction is performed with medial meniscal transplantation, the starting point for the ACL tibial tunnel is moved medially to accommodate the central placement of the two smaller tunnels for the meniscal horn bone plugs. Proper spacing must be used to prevent tunnel confluence. For combined ACL reconstruction with lateral meniscal transplantation, the bone slot is implanted first, followed by creation of the ACL tibial tunnel. There is a small chance the ACL tunnel could partially violate the bone slot; however, the overall integrity and fixation of the graft should not be compromised. If both medial and lateral MATs are performed simultaneously, a common bone bridge containing the attachments of both menisci is used for fixation. Finally, in conjunction with either cartilage resurfacing or osteotomy, meniscal transplantation is always completed first. This ensures the cartilage graft is not damaged during the passage of meniscal needles, and excessive stress is not placed on the osteotomy during knee positioning for meniscal suturing.
RESULTS OF MENISCAL TRANSPLANTATION
Recent mid- and long-term follow-up studies have produced more conclusive results for meniscal allograft procedures; however, there is still a need for additional long-term studies that limit variability in protocol and/or provide isolated MAT results. Although MAT is one of the most effective alternative treatments for meniscectomized knees and may delay articular cartilage degeneration, restore the chondroprotective function of the meniscus to some degree, and provide pain relief and functional improvement, there are several unfavorable outcomes from the procedure that may result. These include degeneration, deformation, tearing, and structural changes of the transplant during the graft remodeling process.67 Factors that affect graft remodeling include graft type and size, degree of arthrosis, meniscocapsular healing, and extrusion.8,67 Thorough evaluation of outcomes requires analysis of both clinical and objective parameters. Objectively, graft condition and joint preservation are evaluated using MRI or second-look arthroscopy.8,67,68 Validated patient-reported outcome scales are used to assess subjective symptoms and overall knee function.
The method of graft preparation and storage used in MAT is a significant factor as well. The two types of graft that are currently preferred over lyophilized (freeze-dried) grafts are fresh and fresh frozen size-matched allografts.67,69 In a clinical outcome study, Wirth et al.61 reported that lyophilized graft recipients had comparable results to the meniscus-deficient group, whereas fresh frozen graft recipients experienced better clinical outcomes that were similar to the intact meniscus control group. On MRI and second-look arthroscopy, the lyophilized grafts showed greater shrinkage compared to fresh frozen grafts. Long-term clinical results were variable, with Lysholm scores ranging from 21 to 97 points at the 20-year postoperative milestone; however, there was clear radiographic evidence of degenerative change. Due to expanding literature corroborating this data, lyophilized grafts are not recommended due to shrinkage and significant changes in the tissue properties of the transplant.61,67
Cryopreserved grafts have more extensive follow-up in the literature. Van Arkel et al.37 reported on a minimum 2-year follow-up of meniscal allografts using cryopreserved transplants with arthroscopic evaluation. Of 23 meniscal transplants, there was partial detachment in 5, and degenerative changes in 5. Cameron and Saha42 examined clinical outcomes, reporting good to excellent results in 19 of 21 (90%) patients who had an isolated meniscal transplant. The midterm failure rate of cryopreserved grafts, defined by reoperation, has been reported to be between 30% and 35%. Failure rates associated with persistent pain and meniscal tear produced cumulative survival rates of the lateral, medial, and bilateral allografts of 76%, 50%, and 67%, respectively.67,70 Long-term follow-up studies have evaluated clinical and objective results, producing a survival rate of 45% at 10 years.67,70 Radiographs and MRI show joint space narrowing and meniscal shrinkage.67 Van der Wal and colleagues71 reported an overall failure rate of 29% at a mean follow-up of 13.8 years postoperatively in cryopreserved MATs. Although Lysholm scores decreased to as low as 61 points, the authors concluded that MAT is a good salvage option for meniscectomized knees. Proposed reasons for cryopreserved graft failure include chondrocyte apoptosis and failure of revascularization.37,60,69
Irradiation of the graft may be detrimental to the success of MAT due to the change in material properties of the meniscal transplant. Yahia and Zukor72 reported that frozen irradiated allograft transplants were less viscous in rabbits when compared to allograft transplants that were nonirradiated fresh or frozen. Noyes and Barber-Westin62 reported high failure rates of fresh frozen allografts that were irradiated with 2.5 mrad. They suggest that irradiation of the meniscus may weaken and denature the tissue, leading to poor results. Of 96 fresh frozen, irradiated transplants, MRI showed that 9 (9%) of the transplants healed, 30 (31%) partially healed, 56 (58%) failed, and 1 (2%) was unknown.
Several studies suggest improved healing rates in patients who have a meniscal transplant with attached bone plugs. Healing of the bone plugs in a bone tunnel is thought to be more secure and reproducible than that of the meniscus to bone, allowing for improved load transmission.8,32,36 Rodeo and Johnson73 reported on 33 meniscus transplants at 2-year follow-up evaluated with MRI and arthroscopy. Arthroscopic inspection in a subset of the patients showed normal appearance, consistency, and position in the knee joint. There was minimal articular cartilage degeneration, although some degenerative changes were commonly noted in the posterior horn on MRI. Based on objective findings, 8 of 33 transplants were rated as good; 14, moderate; 4, poor; and 7, failed. Outcome measures including the International Knee Documentation Committee (IKDC) and Lysholm scales as well as pain and function scores showed clinical improvements. Transplantation with attached bone plugs yielded significantly better results than those without bone plugs: 88% of menisci transplanted with bone plugs were rated as good or moderate in comparison to 47% transplanted with no bone plugs.
Extrusion of the transplant from the tibiofemoral compartment has also been shown on MRI. The greatest amount of extrusion was present in patients with more advanced articular degeneration.73 Using MRI, Potter et al.48 confirmed that extrusion is seen in patients who have flattening of the femoral condyle or advanced degenerative changes in the articular cartilage or posterior horn of the meniscus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


