Risk factors such as family history and younger age at first dislocation have been associated with recurrent instability. As expected, abnormal anatomy including patellofemoral malalignment as measured by increased Q angle, trochlear dysplasia, and abnormal patellar configuration are also associated with recurrent dislocations or instability.20,21,24
The patellofemoral joint is stabilized against lateral instability by both osseous and soft tissue structures. In patients with normal trochlea anatomy, the patella enters the osseous confines of the trochlea at 30 degrees of knee flexion which provides static stability, whereas in extension, the medial patellofemoral ligament (MPFL) is the most important stabilizer of the patellofemoral joint. As opposed to the cruciate ligaments, the MPFL has relatively low tension throughout flexion and extension, between 2 N and 10 N.1 Furthermore, the MPFL remains isometric throughout flexion from 0 to 110 degrees and then becomes slack past 110 degrees of flexion.2 This biomechanical data suggests that the MPFL acts as a “checkrein” for the patella in that it is a main stabilizer against lateral patellar dislocation when an outside force is exerted on the knee in extension. When put to the test in this action of forced lateral subluxation, the native MPFL can withstand a tension of approximately 200 N.3 Studies have shown that when the patella dislocates from trauma, the MPFL is torn in approximately 90% of patients.4 The zone of injury of the MPFL tear, whether it tears off of the patella or its femoral insertion, has been the topic of a number of radiographic studies.4–10 The studies isolated to adolescent patients5–7 have found that the MPFL more commonly is torn near its patellar insertion. In a study of 43 children with acute patellar dislocation, as confirmed by magnetic resonance imaging (MRI), 61% had tears isolated to the patellar insertion.7
The MPFL lies in the second layer of the knee as described by Warren and Marshall.11 The patellar attachment is a fan-like attachment at the junction between the proximal and middle thirds of the superomedial border of the patella.12 A recent anatomic study investigated the patellar insertion of the MPFL in eight cadavers and found the proximal fibers of the MPFL were mainly attached to the vastus intermedius tendon, whereas its distal fibers were inserted partially on the medial retinaculum.13 The authors proposed that this anatomic relationship allows the MPFL to pull both the patella and the patellar tendon, albeit indirectly, medially to keep the patella engaged in the trochlea throughout flexion and extension. The femoral attachment of the MPFL is bounded by the adductor tubercle proximally and the femoral attachment of the medial collateral ligament (MCL) distally.12 In the anterior to posterior dimension, it lies approximately 1.3 mm anterior to a line drawn along the posterior cortex of the femoral diaphysis.14
Surgically addressing the MPFL has become a mainstay of treating PFI given both the biomechanical importance of the MPFL as a restraint to lateral dislocation as well as the high frequency of MPFL injury following traumatic patellar dislocation. Similar to the experience with anterior cruciate ligament repair, repairing the remaining ends of a torn MPFL has not been a successful surgical option.15,16 Dozens of different techniques of MPFL reconstruction have been reported in the literature, and there is still no consensus supporting one technique over another.17 Although MPFL reconstruction in the skeletally mature patient is well described in the literature, there are fewer studies that focus on patients with open growth plates.17,18
A recent patellar dislocation can be confirmed with MRI. Transchondral fracture and bone marrow edema pattern, increased signal intensity in the lateral femoral condyle on fluid-sensitive imaging, and short T1 inversion recovery (STIR) sequencing are indicative of an acute dislocation.7 In addition, cartilage-sensitive magnetic resonance (MR) sequencing is useful in identifying an MPFL tear as well as the zone of injury of such a tear. Finally, MRI also can identify an osteochondral lesion or a loose body that needs to be addressed surgically. Guerrero et al.26 found that 49% of patellar dislocations were associated with an osteochondral lesion and 13% incurred a loose body in the joint.
First-time dislocators are treated with a trial of nonoperative management that includes quadriceps and core strengthening. If this treatment fails and the patient experiences recurrent instability or recurrent episodes of patellar dislocation, then MPFL reconstruction is recommended. Patients with additional risk factors, younger age or family history, as well as those with osteochondral lesions or loose bodies for surgery may be indicated for surgery after their first dislocation event.
Generally, distal realignment procedures are reserved for skeletally mature patients with pathologic patellofemoral anatomy that predisposes to PFI, such as patients with large Q angle (>20 degrees), large J signs, or increase tibial tubercle–trochlear groove distances (TT-TG). A TT-TG distance of over 20 mm is typically used to indicate adults for a tibial tubercle osteotomy (TTO) or other distal realignment procedure. However, recently published literature reported that TT-TG in children increases with age, and an increase in TT-TG should be expected as a child matures.27
If a patient has underlying anatomic pathology, it is important to address this surgically in addition to MPFL reconstruction to achieve a good outcome. For instance, in cases of fixed or obligatory dislocation, part of the etiology is a tight quadriceps mechanism. This must be addressed surgically with a quadriceps release in order to prevent recurrence.
TECHNIQUES DESCRIBED IN LITERATURE
Although over 100 different techniques for reconstructing the MPFL have been described, this section focuses on the six common types of MPFL reconstruction. One such technique, the diversion of a portion of the quadriceps tendon, has been described in the previous chapter. Hemiquad tendon transfer was first described by Steensen et al.28 They harvested the medial and anterior one-third of the quadriceps tendon and redirect this detached tendon to the femur, securing it there with a tenodesis screw (Fig. 17.1A). Similar to the quadriceps diversion technique, various other pedicled graft techniques have been described in the literature. Steiner et al.29 describe isolating the distal adductor group and redirecting it to the patella to reconstruct the MPFL. Furthermore, surgeons can also redirect a portion of the patellar tendon from the tibial tubercle to medial femoral condyle to recreate the path of the MPFL (Fig. 17.1B).

A free hamstring graft can also be used to reconstruct the MPFL, and there are a variety of methods to secure the graft currently used in practice. Although some surgeons prefer to use either the MCL of the knee or the adductor group as a pulley or site of fixation,30,31 many prefer to create sockets or tunnels within the medial femoral condyle and patella to secure the free graft32,33 (Fig. 17.1C,D). Hamstring autograft using the MCL as a pulley was described by Deie et al.31 The authors detach the semitendinosus proximally and leave the distal insertion intact, then use a slit in the MCL as a pulley, finally attaching the graft to the patella to recreate the MPFL.31 Similarly, Gomes30 described a technique that takes advantage of the adductor’s proximity to the native MPFL insertion on the femur and uses this attachment as a pulley for a gracilis or semitendinosus graft (Fig. 17.1E).
Graft Harvest
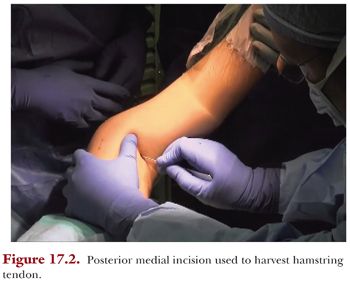
The semitendinosus is our preferred autograft choice. In some of the larger patients, the gracilis is of adequate size. In an isolated MPFL reconstruction, when not combined with a TTO, the semitendinosus is harvested from a transverse posteromedial incision, as it is cosmetically preferable to the anteromedial harvest (Fig. 17.2).
Once the tendon is identified, the open tendon harvester is placed around the tendon and sent proximally (Fig. 17.3). The tendon is isolated at the musculotendinous junction. Then, a closed tendon harvester is inserted distally, crosses the tibial crest to the tendon’s insertion, and then harvested. Approximately 200 mm of tendon length is needed for this technique in most pediatric patients. The final length of this incision is seen in Figure 17.4.




