Skeletally immature patients with patellar dislocations require a thorough evaluation to understand the role that various factors play in their presentation. Medial patellar tendon transfer has been generally used in females younger than 11 years of age or male patients younger than 12 years of age. However, most patients undergoing the procedure are 10 years of age or younger. Patients generally present with a history of chronic patellar dislocations and subluxations and are often able to demonstrate a dislocatable patella on clinical exam. Significant patellofemoral crepitus is extremely rare in this population due to the degree of soft tissue laxity present. Clinical assessment of the patient’s Q angle is generally abnormal. Additionally, assessment of standing lower extremity alignment (mechanical axis) and femoral/tibial rotational profile is important in this population.
Radiographic evaluation with anteroposterior (AP), lateral, notch, and Merchant views is used to assess for patellofemoral tracking as well as any other pathology. The Merchant view commonly demonstrates significant lateral subluxation (or even dislocation) of the patella in these patients. Additionally, some degree of trochlear dysplasia is commonly noted on Merchant and lateral radiographic projections. Patella alta is commonly noted as well. Three-dimensional imaging can be useful to characterize the underlying anatomy including measurement of the tibial tubercle–trochlear groove (TT-TG) distance.
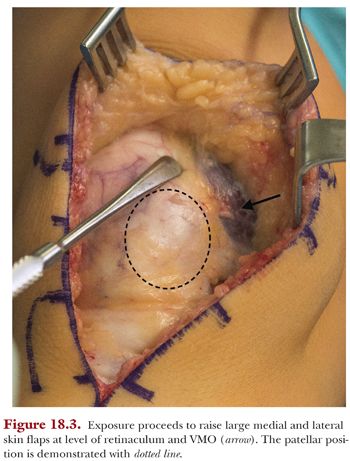
Surgery is performed supine with a bump under the ipsilateral hip. A nonsterile tourniquet is placed prior to sterile prep of the surgical limb. Standard preoperative antibiotic prophylaxis is used. After exsanguination of the leg, the tourniquet is inflated. A midline incision from the level of the superior pole of the patella to 3 cm below the tibial tubercle is used (Fig. 18.2). Circumferential skin flaps are raised at the level of the retinaculum (Fig. 18.3). We have not routinely used arthroscopy in this young patient population, unless clinical evaluation suggests underlying chondromalacia or loose body. We have found intra-articular pathology to be relatively uncommon in this patient population.

Proximal Realignment
Initial dissection for the proximal realignment is performed next. The lateral retinacular release is performed 1 cm lateral to the patella. Care is taken to identify the extrasynovial plane at the beginning of this dissection. This plane can then be followed proximally to the level of the superolateral patella and distally through the fat pad to the level of the tibial tubercle to complete the release. Care should be taken to avoid injury to the periosteum and physis in the distal aspect of the release. The lateral release is initially carried to the superior aspect of the patella, but frequently, an anomalous contracted band of vastus lateralis insertion on the patella is present deep to the initial dissection (Fig. 18.4). Failure to identify this band will result in persistent lateral maltracking.

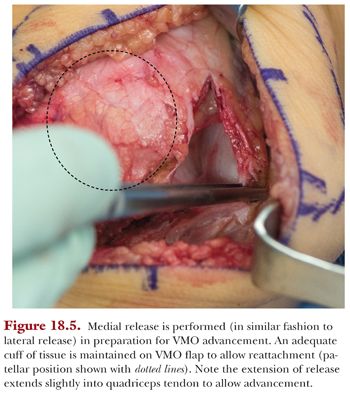
Attention is then turned to the medial retinacular incision performed in preparation for vastus medialis obliquus (VMO) advancement. Similar to the lateral release, the extrasynovial plane is identified. The incision is performed approximately 1 cm medial to the distal half of the patella and extended along the medial border of the tendon. Above the midpoint of the patella, the release is taken across the VMO insertion, with care taken to leave a 5- to 7-mm cuff of tissue for subsequent repair. The release is extended approximately 2 cm into the quadriceps tendon to allow for adequate mobility for the VMO advancement (Fig. 18.5). The plane deep to the VMO is bluntly dissected to allow good mobility of the VMO for lateral advancement. The VMO advancement is not performed at this point but instead as the final step in the procedure after medial patellar tendon transfer.