FIGURE 29-1 A, B: AP, oblique radiographs and lateral radiographs of a displaced medial epicondyle fracture.
Many of life’s failures are people who did not realize how close to success they were when they gave up.
—Thomas Edison
Patients will typically present with medial elbow pain, swelling, and varying degrees of limited elbow motion after acute fractures. History should be taken regarding hand dominance, functional demands including sports participation, prodromal symptoms consistent with overuse apophysitis, and chronicity of symptoms if present. Physical examination will usually elicit tenderness over the (displaced) medial epicondylar fracture fragment, with or without associated swelling, ecchymosis, and limited elbow flexion-extension. A thorough neurovascular examination is critical to rule out evidence of peripheral neuropathy, particularly involving the ulnar nerve.
In patients with acute elbow dislocations, the clinical presentation is less subtle. Patients will present acutely with pain, obvious deformity, and fixed elbow position after a fall or high-energy injury. Neurovascular examination is important to identify primary nerve palsies due to the injury and establish a baseline against which post treatment examinations may be compared. Careful assessment of median and ulnar nerve function is critical. Vascular insufficiency is quite uncommon.
Radiographic evaluation will confirm the diagnosis. Standard anteroposterior (AP) and lateral radiographs will identify the medial epicondylar avulsion fracture and characterize displacement. Oblique radiographs, including the external rotation oblique, will assist in radiographic assessment of fracture displacement as it brings the normally posteromedial medial epicondyle into profile. It is important to recognize that the flexor-pronator mass acts to displace the medial epicondylar apophysis distally and often anteriorly, not laterally, and therefore the magnitude of fracture displacement cannot be quantified on AP radiographs. Indeed, recent information suggests that plain radiographs do not allow for accurate measurement of displacement, and that intra and interobserver reliability of medial epicondylar fracture displacement is low.11,12

FIGURE 29-2 AP and lateral radiographs of a posterolateral elbow dislocation in a 9-year-old female gymnast.
Medial epicondylar fracture fragments can be entrapped in the elbow joint. The trochlear ossification is usually irregular, often fragmented. The medial epicondyle is ovoid and regular. At times, the entrapped medial epicondyle can be mistaken for a trochlea and the diagnosis of an entrapped medial epicondyle missed. Look for the medial epicondyle in or near its anatomic posteromedial location. If it is not there, look for it in the joint. If necessary, compare elbow films of the affected and unaffected side. An entrapped medial epicondyle is a diagnosis not to be missed.
In cases of displaced medial epicondylar apophyseal fractures, joint stability may be assessed using gravity valgus stress views (Figure 29-3). This radiographic technique involves placing the patient in the supine position with the shoulder abducted 90 degrees, elbow extended, and the forearm maximally supinated (the thumb points to the ground). An AP view of the elbow is taken, and the medial joint space is assessed. Medial joint widening of >3 mm is suggestive of valgus instability.
Plain radiographs, including obliques, will also clearly diagnose simple and complex elbow dislocations and characterize the direction of displacement. Elbow dislocations in general are described anatomically according to the position of the forearm in relationship with the distal humerus (e.g., posterolateral, posteromedial, anterior, medial, lateral). “Simple” dislocations denote pure joint dislocations, whereas “complex” dislocations are used to describe joint instability with associated bony or chondral fractures.
Advanced three-dimensional imaging is rarely required in acute cases of medial epicondylar fractures but may provide important additional information in cases of chronic injuries or elbow dislocations with suspected chondral or osteochondral shear fractures (Figure 29-4). Imaging with magnetic resonance imaging (MRI) is particularly useful in these latter situations, especially when nonoperative management is being considered.
Surgical Indications
There are only two options regarding commitment. You’re either in or out. There’s no such thing as a life in-between.
—Pat Riley
The indications for surgical treatment of medial epicondylar avulsion fractures are controversial and continue to evolve. Historically, almost all displaced fractures of the medial epicondyle were treated nonoperatively with reportedly acceptable results. Farsetti et al.13 previously reported on 42 children and adolescents with displaced medial epicondyle fractures followed to an average age of 45 years. Patients treated nonoperatively had similarly good long-term results as those treated with open reduction internal fixation (ORIF). Based upon this information, the authors and others suggest that displaced medial epicondylar fractures may be successfully treated nonoperatively.14 This and other similar reports have established the dogma by some that medial epicondylar avulsion fractures are nonsurgical injuries.
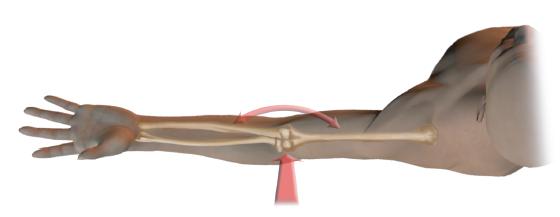
FIGURE 29-3 Schematic representation of the valgus gravity stress radiograph. With the patient supine, the shoulder abducted 90 degrees, elbow extended, and the forearm maximally supinated (the thumb points to the ground). An AP view of the elbow is taken by directing the beam indentllel to the ground, and the medial joint space is assessed.

FIGURE 29-4 Complex elbow dislocation with chondral shear fracture. A: AP and lateral radiographs demonstrate a mildly angulated radial neck fracture and subluxation and incongruity of the ulnohumeral joint. B: Sagittal MRI images depicting an intra-articular loose body (small arrow) from a chondral shear injury to the trochlea (arrowhead) with a dislocated ulnohumeral articulation.
It is clear that patients with medial epicondyle fracture dislocations in whom the fracture fragment is incarcerated within the elbow joint should be treated with expeditious ORIF. Relative indications include displaced fractures with associated ulnar neuritis/neuropathy or fractures affecting the dominant limb in throwing or overhead athletes. We tend to be surgically aggressive for displaced medial epicondyle fractures, given the safety and efficacy of acute surgical treatment and the functional limitations and surgical challenges of symptomatic nonunions or malunions.15–17 We prefer anatomic alignment of the fracture, rigid fixation with elbow joint stability restored, and early motion rehabilitation to avoid a flexion contracture.
Occasionally patients will present for first consultation to the pediatric hand and upper extremity surgeon after closed reduction of an elbow fracture dislocation by a referring caregiver. The previous care can cloud the decision-making process. If the elbow joint is unstable and/or the fracture is still displaced, we tend to proceed with ORIF to provide stability for early range of motion and avoid late complications. Clearly chronically entrapped medial epicondylar fracture fragments require extraction and ORIF no matter how late those patients present for evaluation and care.
In cases of elbow dislocations, it is clear that acute simple elbow dislocations should be treated with prompt closed reduction, either under conscious sedation or under general anesthesia. Surgical indications include complex elbow dislocations with associated nerve injury or entrapment, associated osteochondral fractures, or joint instability precluding appropriate postinjury rehabilitation. Surgical repair of the collateral ligaments and/or muscles is not necessary following successful closed reductions of simple dislocations.18–20
 Closed Treatment of Medial Epicondyle Fractures and Elbow Dislocations
Closed Treatment of Medial Epicondyle Fractures and Elbow Dislocations
As cited above, nonoperative treatment is appropriate for nondisplaced or minimally displaced medial epicondylar fractures without ulnar neuropathy in patients without high functional demands of the affected elbow (e.g., baseball pitchers, gymnasts, cheerleaders) (Figure 29-5). Nonoperative care consists of a brief period of splint or cast immobilization (no longer than 2 weeks), followed by hinged elbow brace protection and advancement of elbow range of motion in brace until 6 weeks postinjury Physical therapy may be initiated at 6 weeks, if needed, to regain the remaining elbow motion and strength. Sports participation is limited until elbow motion and strength normalizes, usually at 2 to 3 months.
One error in nonoperative treatment of medial epicondylar fractures lies in excessive immobilization. The amount of soft tissue and capsular injury cannot be accurately assessed on initial clinical evaluation or radiographs. Stiffness is a risk, even with seemingly innocuous fractures. If nonoperative treatment is chosen—and therefore no intent to achieve anatomic fracture reduction—early protected range-of-motion exercises are critical to avoid functionally limiting stiffness.
The other problem with nonoperative treatment of displaced fractures is symptomatic nonunions or malunions. If the medial epicondylar fragment heals in a displaced distal and anterior position, it will limit motion (especially extension) and function. Some nonunions cause symptomatic valgus instability, especially in gymnasts and throwing athletes.
Closed reduction of simple elbow dislocations follows principles similar to adults. Conscious sedation or general anesthesia is preferred to mitigate the effects of muscle spasm, avoid excessive force, which imparts risk of producing iatrogenic osteochondral shear fractures, and provide maximum patient comfort. In general, for the most common posterior dislocations, closed reduction maneuvers may be divided into “pull” or “push” tech-niques.21–29 With the brachium stabilized and the patient either in the supine or in the prone position, the elbow is flexed and forearm supinated to unlock the radial head and reduce tension on the biceps. Longitudinal traction is then provided distally along the axis of the humerus, with simultaneous anteriorly directed force. Hyperextension is avoided, as it further tensions the anterior capsule and flexor muscles and may lead to iatrogenic shear fractures of the radial head, coronoid process, trochlea, or capitellum. Reduction with extension also increases the risk of entrapment of the median nerve in the joint. Alternatively, distally directed pressure may be applied to the prominent olecranon process and radial head with the elbow flexed and forearm supinated to “push” the forearm back into position. Following reduction, careful radiographic evaluation is performed to confirm a congruent joint reduction and rule out associated fractures, which may not be apparent on initial injury films. The stable arc of motion is assessed and the limb immobilized in a long-arm bivalved cast or posterior splint with the forearm in pronation. The postreduction immobilization needs to be quite bulky as elbow dislocations will have considerable soft tissue swelling in the first week postinjury.
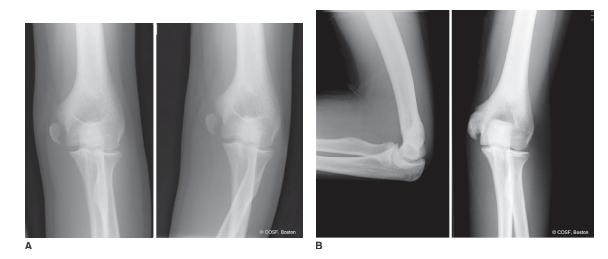
FIGURE 29-5 Nonoperative treatment of a displaced medial epicondyle fracture involving the nondominant limb of a 14-year-old male. A: Initial AP and lateral radiographs demonstrate a displaced medial epicondyle apophyseal avulsion. B: Follow-up radiographs 3 months postinjury demonstrate evidence of bony union with exostosis. At times this can lead to ulnar nerve compression.
 ORIF of Medial Epicondylar Fractures
ORIF of Medial Epicondylar Fractures
An ORIF of displaced medial epicondylar apophyseal fracture fragments is performed under general anesthesia and tourniquet control (Figure 29-6). In cases of fracture dislocations with the fracture fragment incarcerated in the elbow joint, initial attempts at closed manipulation may be performed under general anesthesia before proceeding to open repair.30,31 With valgus stress imparted on the elbow and forearm supinated, the wrist and digits are maximally extended. Tension on the extrinsic flexors and pronators, in theory, will allow for fragment extraction. Fluoroscopy will confirm success or failure of closed manipulation.
A medial longitudinal incision is created along the distal humerus, centered on the fracture site. It is easy to make this incision too anteriorly, which will in turn cause greater difficulty in reducing the displaced fracture to the normal posteromedial apophyseal location. Skin flaps are raised and blunt dissection performed down to the level of the fracture; in acute settings, this subcutaneous dissection often involves only a sweep of the surgeon’s finger, as the injury itself has developed the appropriate planes of dissection. Protect the crossing cutaneous nerves. The medial epicondyle fragment is identified, preserving its distally attached flexor-pronator muscles, and the fracture site and joint are entered from above the fragment while maintaining the soft tissue integrity. A heavy nonabsorbable suture (No. 1 Ethibond, Ethicon, Inc., Somerville, NJ) is passed in a figure-of-eight fashion through the proximal aspect of the fracture fragment and periosteal sleeve, which is used for traction as well as subsequent soft tissue repair. Careful dissection is performed proximally and posteriorly to the origin of the medial epicondylar apophysis, and the ulnar nerve should be retracted and protected at all times during the course of the procedure. The elbow joint is inspected for associated osteochondral injuries, and the intra-articular hematoma is debrided with saline, suction, and fine-tipped forceps. The fracture is then mobilized, and confirmation is made that an anatomic reduction can be achieved (Sidebar).
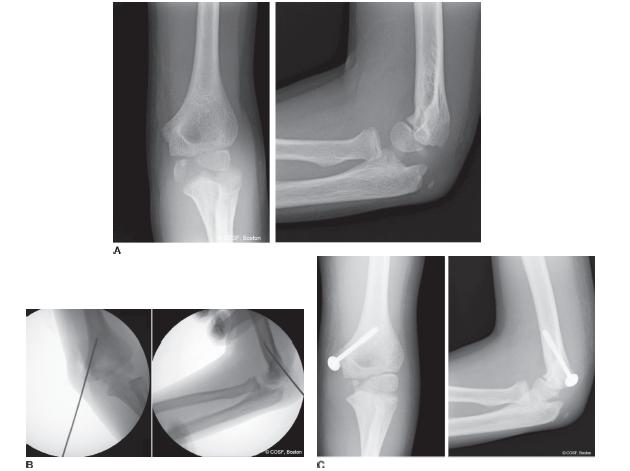
FIGURE 29-6 Open reduction and cannulated screw fixation of a displaced incarcerated medial epicondyle fracture in an 11-year-old male. A: Injury AP and lateral radiographs depict an incarcerated medial epicondyle within the ulnohumeral joint. B: Intraoperatively, after fragment extraction and reduction, a guide pin is used for provisional fixation and subsequent cannulated screw placement. C: Following postoperative radiographs demonstrating reduction and fixation with a partially threaded cannulated screw with washer. Note is made of the appropriate posterior-to-anterior trajectory of the screw on the lateral projection.
With the fracture reduced, a threaded guide pin from a cannulated screw set is placed in the center of the fracture fragment and then driven across the fracture into the medial column of the distal humerus. In general, a 3.5-or 4.5- mm screw is used. Often, the bony piece available for fixation is much smaller than the size of the apophysis that is palpated, as much of the avulsed fragment is comprised of cartilage surrounded by soft tissue. Care must be taken to place the guide pin through the center of the bone without fragmenting it. At times, the medial epicondylar fracture fragment is predrilled before reduction, and the drill is used to aid in anatomic reduction. Another useful method is to suture the medial epicondyle in place before pin placement. Intraoperative fluoroscopy is then used to confirm adequacy of the reduction and guide pin trajectory (which is posterior to anterior in the lateral projection). A second guide pin may then be placed in a indentllel fashion for provisional rotational control. Measurements are taken, the central guide pin overdrilled, and a partially threaded 3.5- or 4.5- mm cannulated screw is inserted with a washer. With the use of a partially threaded screw, purchase of the far cortex is not needed, and a 40- to 50- mm length screw is typically used. If a fully threaded cortical screw is used, the screw should engage the far anterolateral cortex to achieve fracture compression and stability Following fixation, fluoroscopy is again used to confirm fracture reduction, joint stability including valgus stress, and implant placement. The ulnar nerve is again checked to ascertain that no kinking or compression has occurred during screw fixation. Range of motion is checked to be certain there are no limits to the flexion-extension arc and the ulnar nerve does not impinge on the screw. The wound is closed in layers. Patients are immobilized in a hinged elbow brace, posterior elbow splint, or a long-arm cast that is bivalved widely to allow for postoperative swelling.
 ORIF of Osteochondral Fracture
ORIF of Osteochondral Fracture
As stated above, osteochondral fractures are associated in up to half of all elbow dislocations in pediatric patients.32–35 For this reason, careful radiographic evaluation after closed reduction to look for apophyseal avulsion or osteochondral fractures is imperative (Figure 29-7). While fractures of the medial epicondyle and radial neck, for example, are quite obvious, osteochondral injuries may only be manifest by subtle, thin radiopacities or soft tissue shadows on plain radiographs. Advanced imaging is appropriate in any suspected case of osteochondral injury, particularly if there is suspicion of intra-articular loose bodies. This is particularly true of elbow dislocations due to high-energy trauma in patients <10 years of age, in whom the articulating surfaces of the humerus, radius, and ulna are predominantly cartilaginous.
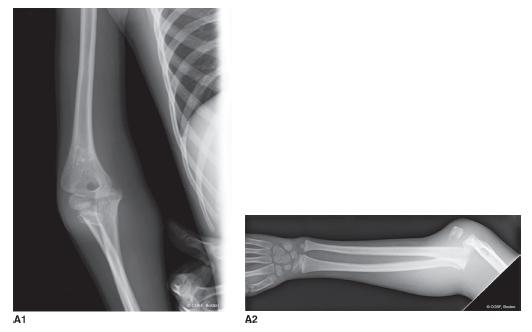
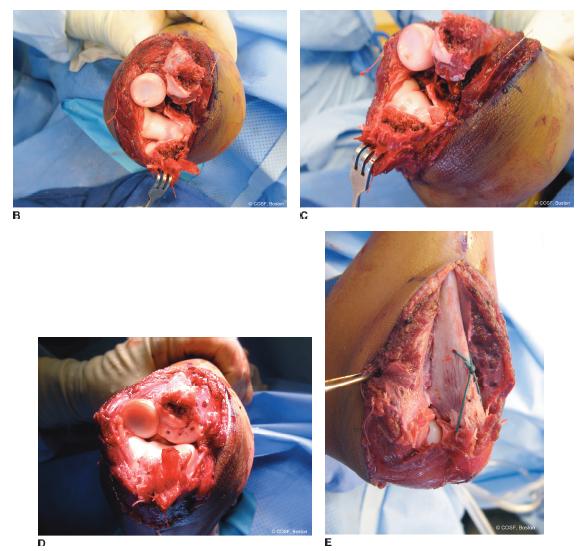
FIGURE 29-7 Osteochondral injuries associated with an elbow fracture dislocation in a 7-year-old male following a fall down stairs. A: Injury AP and lateral radiographs demonstrate an anterior elbow dislocation with olecranon fracture. Note is made of the extensive soft tissue swelling. B, C: Intraoperative photographs of the elbow joint, exposed through the olecranon fracture, demonstrate multiple osteochondral fractures of the ulna with loose bodies. D: Initial restoration of the articular surface is performed with reduction and fixation of the osteochondral fragments using bioabsorbable implants. E: Final reconstruction demonstrating restoration of the articular surfaces and tension band fixation of the ulna
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


