Chapter 40
Maternal Mortality
Jill M. Mhyre MD
Chapter Outline
Global Maternal Mortality
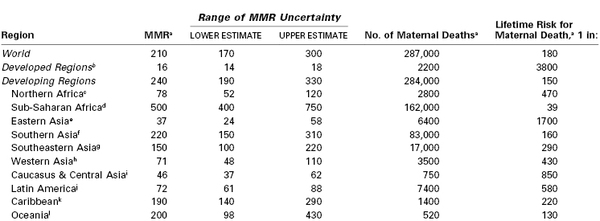
Globally in 2010, 287,000 women died while pregnant or within 42 days of the end of pregnancy.1 This number corresponds to a ratio of 210 maternal deaths per 100,000 live births and to a 1-in-180 lifetime risk for maternal death for each girl entering her childbearing years (Table 40-1).1 According to the World Health Organization (WHO), “No issue is more central to global well-being than maternal and perinatal health. Every individual, every family and every community is at some point intimately involved in pregnancy and the success of childbirth.”2
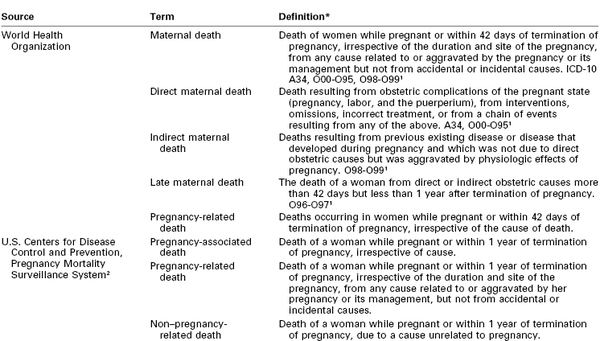
Definitions for maternal death are listed in Table 40-2, and measures of maternal mortality are listed in Table 40-3. More than 99% of maternal deaths occur in developing countries, with 85% in either sub-Saharan Africa or South Asia (see Table 40-1). As part of the Millennium Development Goals,1 the international community committed to reduce the maternal mortality ratio (MMR) by 75% between 1990 and 2015,1 from 400 to less than 100 per 100,000 live births. Between 1990 and 2010, the global MMR fell by 47%, with the greatest reductions demonstrated in East Asia (69%), North Africa (66%), and South Asia (64%).1 Although the MMR declined 41% in sub-Saharan Africa, the lifetime risk for maternal death remains unacceptably high, at 1 in 39.1 There is considerable regional variation. Within sub-Saharan Africa, the highest MMRs are in Chad (1100) and Somalia (1000) and represent rates that are 10-fold higher than the lowest ratios in the region.1
TABLE 40-3
Measures of Maternal Mortality
| Maternal Mortality Measure | Definitions | Reports Using the Measure |
| Maternal mortality ratio (MMR) | Direct and indirect maternal deaths, but not late maternal deaths, per 100,000 live births | WHO1 |
| Maternal mortality rate | Direct and indirect maternal deaths, but not late maternal deaths, per 100,000 maternities (pregnancies resulting in a live birth or stillbirth ≥ 20 weeks gestational age) | UK CEMD63 |
| Pregnancy-related mortality ratio (PRMR) | Pregnancy-related deaths per 100,000 live births | US CDC PMSS75 |
| Lifetime risk for maternal death | The lifetime risk for maternal death takes into account both the probability of becoming pregnant and the probability of dying as a result of that pregnancy cumulated across a woman’s reproductive years | WHO1 |
UK CEMD, The United Kingdom Confidential Enquiry into Maternal Death; US CDC PMSS, U.S. Centers for Disease Control and Prevention Pregnancy Mortality Surveillance System; WHO, World Health Organization.
Leading Causes
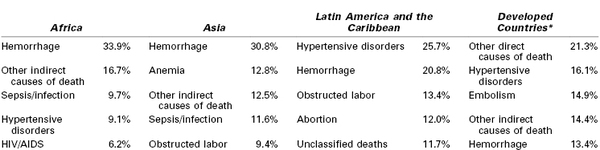
Hemorrhage, hypertensive disorders of pregnancy, and sepsis account for more than half of global maternal deaths and for slightly more than a third of deaths in the developed world.3 Hemorrhage is the leading cause of maternal death in both Africa and Asia (Table 40-4). Hypertensive disorders represent the leading cause in Latin America and the Caribbean.3 Infection and sepsis may be substantially underestimated in regions where laboratory diagnostic tests are unavailable.4 In one Malawi hospital with full laboratory capabilities, infection played a primary role in almost three fourths of all maternal deaths.5
Anemia and obstructed labor each cause approximately one tenth of maternal deaths in Asia.3 Anemia is associated with (1) iron and other micronutrient deficiencies, (2) pregnancy intervals of less than 1 year, (3) adolescent pregnancy, (4) hemoglobinopathy, (5) urinary tract infection, (6) human immunodeficiency virus (HIV) infection, (7) parasitic infections including malaria, and (8) recurrent antepartum hemorrhage.6–8 Anemia can cause lethal congestive heart failure in pregnancy7 and also increases the risk for maternal death from other complications, particularly hemorrhage and infection.6
Obstructed labor is an important cause of maternal death in communities in which early adolescent pregnancy is common, childhood malnutrition leads to small maternal pelves, and operative delivery is unavailable.9 Maternal mortality from obstructed labor is largely the result of uterine rupture or ascending genital tract infection.9,10 Prolonged pressure on the pelvic outlet can lead to tissue necrosis and obstetric fistula, which is thought to affect between 2 and 3.5 million women worldwide.11,12
HIV/acquired immune deficiency syndrome (AIDS) increases vulnerability to both nonobstetric infection (e.g., tuberculosis, malaria) and obstetric complications (e.g., hemorrhage, pregnancy-related sepsis, septic abortion).13,14 The WHO attributed 6.5% of maternal deaths in 2010 to HIV/AIDS.1 In contrast, the Institute of Health Metrics and Evaluation estimated that one in five maternal deaths in 2011 would not have occurred in the absence of the HIV epidemic, based on statistical models that account for the prevalence of HIV within a population.15,16 In countries most severely affected, including Botswana, Malawi, Namibia, South Africa, Swaziland, and Zimbabwe, MMRs increased between 1990 and 2000, but they have since begun to decline as antiretroviral therapy becomes increasingly available.1,15,16
Maternal deaths attributed to unsafe abortion account for 13% of maternal deaths worldwide (47,000 in 2008).17 The WHO defines unsafe abortion as “a procedure for terminating an unintended pregnancy either by individuals without the necessary skills or in an environment that does not conform to minimum medical standards, or both.”17,18 Worldwide, 49% of abortions were unsafe in 2008, compared with 44% in 1995.19 The case-fatality rate (460 maternal deaths per 100,000 unsafe abortions) and the absolute number of maternal deaths per year (28,500) are highest in sub-Saharan Africa.17,20
Early marriage (before age 18 years) has been identified as a major health risk for girls, increasing their exposure to domestic violence, coercion, pregnancy, and sexually transmitted diseases such as HIV/AIDS.21–23 Girls younger than 15 years are five times more likely to die in childbirth than women in their 20s,24 and pregnancy is among the leading causes of death worldwide for girls ages 15 to 19.25 Early childbearing also increases the likelihood of high parity birth (≥ 5) later in life. With a threefold increase in the MMR, high parity is the most important demographic risk for maternal death because it remains so common, accounting for 29% of births globally between 1990 and 2005.26 Advanced maternal age is less common globally but increases individual risk for maternal death as much as fourfold for women aged 35 years or older and as much as eightfold after age 40.27
Anesthesia providers working in the developing world must contend with profound limitations in staffing, equipment, and other resources.14,28–33 In addition, patients who labor at home may face a variety of social and environmental obstacles to reach a facility with the capacity to provide comprehensive emergency obstetric care,34–36 and many arrive at these facilities in septic or hemorrhagic shock.37,38 Cesarean delivery is the most common major surgical procedure in Africa,39 and perioperative maternal mortality is estimated to be between 1.2% and 2%.40–42 As many as one third of deaths that occur within 24 hours of surgery have been attributed to anesthesia, mainly because of airway problems with general anesthesia or hemodynamic collapse with neuraxial anesthesia.14,28,29,43 Peripartum deaths have also been attributed to limited availability or affordability of blood products.32,40,43,44 The number of maternal perioperative deaths likely pales in comparison with maternal deaths that result from the unmet need for lifesaving obstetric procedures, including cesarean delivery.45
Strategies to reduce global maternal mortality include (1) improvement in family planning services and a reduction in the performance of unsafe abortion46,47; (2) community-based education focused on safe birth practices and indications for transfer to a higher level of care48–51; and (3) development of the infrastructure needed to provide timely emergency obstetric care, including the performance of indicated cesarean delivery (and safe administration of anesthesia) by trained care providers, who can also provide resuscitation of women in whom shock develops secondary to hemorrhage or infection.52–57 Limited human, political, and economic capital mandate ongoing rigorous evaluation of the effectiveness of future programmatic efforts.58,59 Cluster randomized trials to evaluate these strategies are beginning to appear48,49,51 and suggest that certain interventions succeed only when deployed as part of an integrated, context-specific and culturally sensitive program.55 For example, training traditional birth attendants to identify and manage complications may only improve maternal and perinatal outcomes if accompanied by ongoing training, resource support, and effective referral pathways to emergency obstetric care.60
Maternal Mortality in the Developed World
In developed regions of the world, the reported MMR has traditionally fluctuated around 10 per 100,000 live births.61 As of 2010, the WHO has reported an MMR of 16 (95% confidence interval [CI], 14 to 18). This apparent increase reflects increases documented primarily in the United States, as well as expansion of the developed world to include Cyprus, Israel, the Republic of Moldova, Belarus, the Russian Federation, and Ukraine.1
The most comprehensive maternal surveillance system in the world is the Confidential Enquiry into Maternal Deaths (CEMD) in the United Kingdom.* Triennial reports of CEMD in England and Wales extend back to 1952 and have covered the entire United Kingdom since the 1985 to 1987 report. By government mandate, all maternal deaths are subject to this enquiry, and health professionals have a duty to provide all requested information.62,63 Once a case is identified, practitioners are asked to provide (1) a full account of the circumstances leading up to the woman’s death, (2) all supporting records, (3) any clinical or other lessons that have been learned, and (4) details of any actions that may have been taken as a result.62,63 Regional assessors review the files to ensure completeness before removing identifying information. Central assessors compile the cases and produce the triennial reports. The reports focus on both medical and nonmedical recommendations for action to improve safety for future pregnant women.
The CEMD reports include both the internationally defined MMR and the U.K.-defined maternal mortality rate (see Table 40-3). The numerator for the U.K.-defined maternal mortality rate includes all deaths that in the opinion of the central assessors are related to pregnancy, including some causes that are not internationally coded as maternity related (e.g., suicide attributed to postpartum depression). The denominator includes all pregnancies that resulted in a live birth or stillbirth after 20 weeks’ gestation. The international MMR is calculated strictly from data coded on death certificates; the U.K. maternal mortality rate includes all deaths identified through active surveillance. As a result, the 2006 to 2008 internationally defined MMR for the United Kingdom (6.69 per 100,000 live births) is significantly lower than the 2006 through 2008 maternal mortality rate (11.39 per 100,000 maternities).63,64
National confidential enquiry reports are now published by many other countries, including Australia,65 France,66 the Netherlands,67 New Zealand,68 and South Africa.14
In the United States, the National Center for Health Statistics (NCHS) has provided maternal death counts since 1900 and MMRs since 1915.69 Accuracy is limited because (1) the system relies on death certificates rather than active surveillance, (2) the certification of death is the legal responsibility of individual states, and (3) the process of maternal death ascertainment varies by state.
The U.S. MMR reported by the NCHS declined from more than 600 deaths per 100,000 live births in 1915 to fewer than 10 deaths per 100,000 live births by 1980 (Figure 40-1).69 Throughout the 1980s and 1990s, the MMR oscillated between 6.6 and 9.2. Then in 1999, the MMR began to increase, reaching 16.6 in 2009 (Figure 40-2).70 Improvements in ascertainment explain some of the increase. In 1999, the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) replaced the ICD-9 as the coding system for U.S. death certificates and liberalized the criteria by which pregnancy could be linked with death. Growing numbers of states perform electronic matches among women’s death certificates, live birth certificates, and fetal death files. In addition, increasing numbers of states have adopted the 2003 revision of the U.S. Standard Certificate of Death, which introduced questions about pregnancy status at the time of death (Box 40-1). By 2005, 19 states had adopted the standard pregnancy questions; the MMR calculated from vital records in these states was 17.3, compared with 10.7 from states without any questions about pregnancy on the state death certificate.71
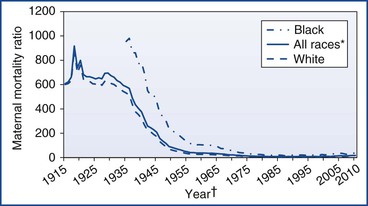
FIGURE 40-1 U.S. maternal mortality ratios by race, 1915 to 2010.69,70,155–158 *Includes races other than white and black. †For 1915 to 1934, data on black race not available.
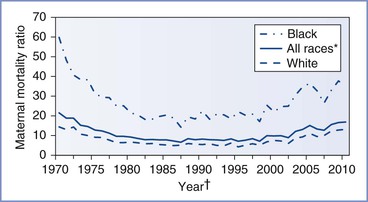
FIGURE 40-2 U.S. maternal mortality ratios by race, 1970 to 2010.69,70,155–158 *Includes races other than white and black. †Beginning in 1989, race for live births tabulated according to race of mother, not child.
In 1987, the Centers for Disease Control and Prevention (CDC) partnered with state health departments and the American College of Obstetricians and Gynecologists (ACOG) to form the Pregnancy Mortality Surveillance System (PMSS).72 To capture maternal deaths more completely, the PMSS recommended that states develop an active surveillance system and collect death certificates and matching live birth or fetal death certificates for all pregnancy-associated deaths (defined in Table 40-2). These certificates are forwarded to the CDC, where clinically experienced epidemiologists manually review the certificates to identify all pregnancy-related deaths (defined in Table 40-2). Similar surveillance enhancement procedures have been estimated to improve case ascertainment by between 22% and 93%.73 The pregnancy-related mortality ratio (PRMR) includes deaths that took place up to a year after the end of pregnancy and, according to the PMSS, increased from 10.3 in 1991 to 16.8 in 2003 before returning to 15.4 in 2005.74,75 Documentation of pregnancy on the death certificate increases ascertainment further. In 2005, among the 19 states with death certificates that include the standard pregnancy questions, the combination of data from the NCHS and the PMSS suggests an MMR of 19.7 and a PRMR of 22.3.71
Leading Causes
According to a 2006 systematic review of data from Europe, North America, Australia, New Zealand, and Japan, hypertensive disorders of pregnancy, embolic disorders, and hemorrhage together account for slightly less than half of maternal deaths in the developed world (see Table 40-4).3 Indirect deaths account for another 14%.3
Indirect deaths have exceeded direct deaths in the United Kingdom since 1997, with cardiac disease being the most common category of death. Similar patterns are seen in the United States, where the combination of cardiovascular conditions and cardiomyopathy comprised 23% of all pregnancy-related deaths between 1998 and 2005 and cerebrovascular accidents and noncardiovascular medical conditions represented another 20%.75 Cause-specific mortality ratios are shown in Table 40-e1 (available online at expertconsult.com). Cardiomyopathy, including both peripartum and other types of cardiomyopathy, is the leading diagnosis underlying maternal cardiac death in both the United States and the United Kingdom.63,75
TABLE 40-e1
Ratios of Leading Causes of Maternal Death in the United States (1987-2007) and United Kingdom (1988-2008)
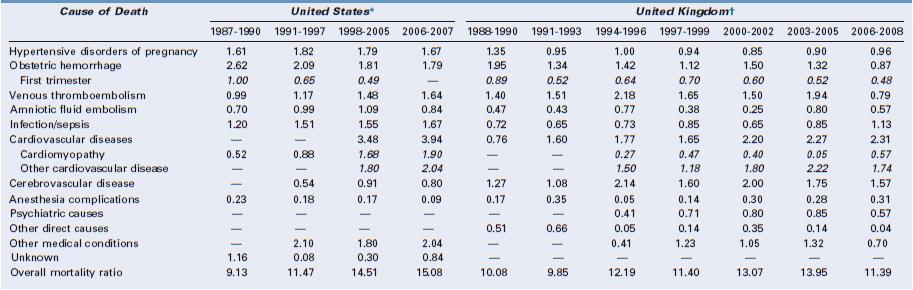
* United States: Cause-specific mortality ratio includes death during pregnancy and up to 1 year after the end of pregnancy per 100,000 live births. Data from references 1 to 4 below.
† United Kingdom: Cause-specific mortality ratio includes deaths during pregnancy and up to 1 year after the end of pregnancy per 100,000 pregnancies lasting at least 20 weeks’ gestation. Italicized numbers represent subcategories of the numbers listed above. Data from reference 5 below.
References
Venous thromboembolism was the leading direct cause of maternal death in the United Kingdom for many years (see online Table 40-e1), but a national campaign to improve venous thromboembolism prophylaxis heralded a 60% reduction in the cause-specific mortality ratio to 0.79 per 100,000 in the 2006 to 2008 CEMD report.63,76,77
During this period, sepsis due to genital tract infection emerged as the leading cause of direct obstetric death in the United Kingdom and was largely attributed to community-acquired group A streptococcal disease.63,64 Current recommendations focus on early warning scoring systems to identify vital sign derangements that could indicate systemic infection, standardized management according to the Surviving Sepsis Campaign, and early involvement of anesthesiologists and intensivists.63,78 More detail is provided in Chapters 37 and 55.
In the United States between 1998 and 2005, seven conditions each accounted for 10% to 13% of all pregnancy-related deaths, including hemorrhage, hypertensive disorders of pregnancy, sepsis, thrombotic pulmonary embolism, cardiomyopathy, other cardiovascular disorders, and noncardiovascular medical disorders (see online Table 40-e1).75
Injury-related deaths are considered pregnancy-associated but not pregnancy-related; they are discussed in Chapter 55.
Risk Factors
Detailed descriptions of hypertensive disorders of pregnancy, obstetric sepsis, maternal hemorrhage, embolic disorders, and cardiovascular diseases in pregnancy are provided in Chapters 36, 37, 38, 39, and 42, respectively. Common clinical and sociodemographic factors that increase the risk for maternal death from all of these complications are discussed in this chapter (see later discussion).
Advanced maternal age increases maternal risk,79 with a linear trend evident for each 5-year increase in maternal age beyond 34 years.63 In the United States between 1998 and 2005, the PRMR among women 40 years of age and older was 166.9 for black women (compared with 24.8 for black women 20 to 24 years of age) and 40.0 for white women (compared with 7.5 for white women 20 to 24 years of age).75 Based on data from the PMSS for the years 1991 through 1999, the association between age and mortality persisted after data were controlled for parity, prenatal care, race, and education.79 Among older black women (≥ 40 years), the excess risks were greatest for hypertensive disorders of pregnancy, infection, cerebrovascular accident, and other medical conditions. Among older white women, the greatest excess risks for death were due to hemorrhage, cardiomyopathy, embolic disorders, and other medical conditions.79
In the United States, black or African-American race significantly correlates with the risk for death. Non-Hispanic black women experience a PRMR that is 3.5-fold higher than non-Hispanic white women. Based on death certificate data (1999 to 2009), disparities are most dramatic for deaths associated with ectopic pregnancy (black-to-white ratio of 4.8), cardiomyopathy (4.2), and deaths from complications of anesthesia (2.9).70 In a case series of anesthesia-related maternal deaths in Michigan published in 2007, six of eight deaths occurred among non-Hispanic black women in Detroit, suggesting a profound concentration of maternal risk.80 The disparity in maternal mortality between black and white women persists after data are controlled for maternal age, income, and receipt of prenatal care81 and appears to be related to a higher case-fatality rate.82
Other racial and ethnic groups also experience increased risk.63 In the United States between 1999 and 2009, in comparison with non-Hispanic white women, the MMR was 80% higher for American Indian or Alaska Native women.70 In England, black African, black Caribbean, Indian, Pakistani, and Chinese women have higher relative risks of death than white women.63,83
Immigrants, asylum seekers, and non-native speakers appear to be particularly vulnerable to both maternal death and substandard care, based on data from the United Kingdom and the Netherlands.63,67,83,84 In the United States, Hispanic and Asian/Pacific Islander immigrants face increased risk compared with women of these same racial/ethnic groups born in the United States.85
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree