2Edinburgh Breast Unit Western General Hospital, Edinburgh, UK
Overview
- Breast pain alone or painful lumpiness is common and accounts for approximately 50% of all referrals of new patients to clinics
- Breast pain is a rare symptom of breast cancer
- Pain in the breast can arise from the breast or from the underlying chest wall
- Careful examination can differentiate chest wall pain from true breast pain
- Few patients with breast pain need treatment with drugs
Mastalgia is pain in the breast. Up to 70% of women will experience this at some time during their life. The pain women describe as breast pain can arise either in the breast tissue itself or it can be referred pain, which is felt in the breast. The nerve supply to the breast is from the anterolateral and anteromedial branches of the intercostal nerves from T3 to T5 and irritation of these nerves anywhere along their course can lead to pain that is felt in the breast or nipple. A branch of T4 penetrates the deep surface of the breast and runs up to the nipple. Irritation of this nerve can result in the shooting pain up to the nipple that many women describe. Pain can also be referred from the breast or chest wall through the intercostobrachial nerve to the inner aspect of the arm.
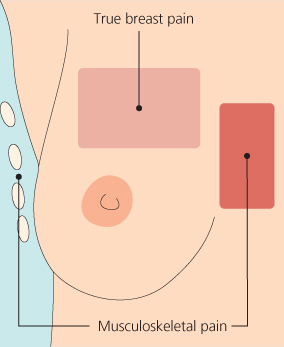
It is important to differentiate between pain referred to the breast from the chest wall and true breast pain, because management of these two conditions is different. It is less important to differentiate cyclical mastalgia—pain that occurs only in the premenstrual part of the menstrual cycle—from non-cyclical mastalgia, as management of these conditions is similar. Pain may last throughout the cycle or bear no relation to the menstrual cycle.
Primary care studies indicate that the most common type of mastalgia is pain referred from the chest wall. In breast clinics chest wall pain is now also more common than true breast pain. Clinical examination reveals that even in women with a classic history of cyclical breast pain, the chest wall is most often the site of origin of the pain (Table 3.1).
Table 3.1 Classification of non-cyclical mastalgia.
| Chest wall causes | Non-breast causes |
| Such as tender costochondral | Cervical and thoracic spondylosis |
| junctions (Tietze’s syndrome) | Lung disease |
| Gall stones | |
| True breast pain | Exogenous oestrogens, such as |
| Diffuse breast pain | hormone replacement therapy |
| Trigger spots in breast | Thoracic outlet syndrome |
Chest Wall Pain
Features suggesting that breast pain is referred rather than originating in the breast include pain that
- is unilateral, and brought on by activity;
- is very lateral or medial in the breast; and
- can be reproduced by pressure on a specific area of the chest wall.
Women who are postmenopausal and not taking hormonal supplements or who are known to have spondylosis or osteoarthritis are much more likely to have musculoskeletal pain rather than true breast pain.
Careful clinical examination is essential to help determine the site of origin of the pain (Table 3.2; Figures 3.1–3.3). Any patient complaining of breast pain should have a complete breast examination including palpation with the woman lying on each side, allowing the breast to fall away from the chest wall, and palpation of the underlying muscles and ribs. The patient should be asked to indicate whether there is any localised tenderness on palpation of the chest wall and whether any discomfort evident during examination is similar to the pain they normally experience. If the patient has pain in the lower part of the breast the underlying chest wall is examined by lifting the breast with one hand while palpating the underlying chest wall with the other hand. Allowing the woman herself to confirm that the site of maximal tenderness is in the underlying chest wall rather than the breast is an effective method of reassuring patients of the site of the pain.
Table 3.2 Principles of mastalgia treatment.
| Exclude cancer | Assess site of pain |
|
|
| Provide reassurance and information |
Figure 3.1 How to examine for lateral chest wall tenderness. The patient is rolled on her side with the breast falling away from the site of the pain laterally. The underlying chest wall is then palpated to identify any area of localised tenderness.

Figure 3.2 How to examine for medial chest wall tenderness over the costochondral junctions. The patient is rolled on her side with the breast falling away from the site of the pain medially. The underlying chest wall is then palpated to identify any area of localised tenderness.

Figure 3.3 How to examine for chest wall tenderness under the lower part of the breast. The breast is lifted upwards by one hand while the other hand presses gently on the underlying chest wall to identify any area of localised tenderness.

Treatment of Chest Wall Pain
The mainstay of treating chest wall pain is reassurance that there is no serious underlying cause for the pain. In women with troublesome pain, providing that there are no contraindications, non-steroidal anti-inflammatory drugs (NSAIDs) are usually effective. Although there is no evidence to suggest that topical NSAIDs have any benefit over oral preparations, there is some evidence that topical agents cause fewer gastrointestinal problems. Women often report a recent increase in activities, such as gardening, decorating, lifting or increased visits to the gym, after which they become aware of pain. Lifestyle is important in relation to breast pain. It is more common in women who spend many hours sitting at a desk in front of a computer. Identifying any underlying behaviour and modifying lifestyle accordingly form the cornerstone of treatment.
If the pain is very localised to one specific spot, then infiltrating the affected chest wall with prednisolone 40 mg in depot form combined with long-acting local anaesthetic can produce long-lasting pain relief (Table 3.3). If the correct area has been targeted, the pain should disappear quickly. About half of women with a localised tender spot get enduring benefit from a single injection. Repeating the injection after 4–6 weeks increases both the number of women getting benefit and provides long-lasting pain control for two-thirds of women with very localised troublesome pain that ‘interferes’ with regular daily activities.
Table 3.3 Outcome of women with chest wall pain treated by local infiltration of bupivacaine (Marcain) plus depot steroid (injected group) or observation alone (comparative group).
| Injected group | Comparative group | |
| No of women | 104 | 34 |
| No who attended follow up | 100 | 29 |
| No (%) with complete resolution of pain* | 61* (61) | 5 (17) |
| No (%) with partial resolution of pain | 22 (22) | 8 (22.5) |
| No (%) with successful outcome* | 83* (83) | 13 (44.8) |
*Differences significant at p < 0.0001.
Chronic Pain Following Breast Surgery
Similar symptoms of chest wall pain are commonly reported after breast surgery, affecting up to 50% of women in some surveys. It is important to rule out underlying causes such as local recurrence or a prior underlying cause of chronic pain. Typically the introduction of gabapentin, pregabalin or amitryptiline is recommended in all forms of neuropathic pain such as scar pain or intercostobrachial neuralgia. The authors have used external neuromodulation for postoperative neuropathic pain with promising results. External neuromodulation consists of the application of electrical current through an external probe over the painful area, trigger zone or affected nerve. The pain reduction can be immediate and quality of life can be dramatically improved following regular applications. Further studies are required to establish the role of this treatment in chronic breast pain.
True Mastalgia
Pain arising in the breast tissue itself is often associated with cyclical swelling and nodularity (Figure 3.4). Hormonal changes are thought to be responsible for these changes in the breast, as they are most commonly seen in the week before menstruation and are relieved by its onset. In addition, the pain can be brought on by hormonal manipulation such as oestrogen containing hormone replacement therapy. It is much less of a problem in women taking tibolone. There are several theories regarding the pathophysiology of mastalgia.
Figure 3.4 Classification of non-cyclical breast pain. Non-cyclical pain can be divided into true breast pain arising from the breast tissue or musculoskeletal pain arising from the ribs or chest wall. Musculoskeletal pain is commonly medially (Tietze’s syndrome) or laterally at the edge of the breast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


