Management of Hyponatremia
INDICATION
This chapter outlines the treatment of low serum sodium levels in patients in the neonatal intensive care unit (NICU), particularly those dependent on parenteral fluids.
Epidemiology
The reported incidence of a serum sodium below 130 for very low birth weight infants in the NICU varies in the literature from about one-quarter to one-third.
Clinical Findings
Initially, neonates should be in good fluid and electrolyte balance and thus have normal serum sodium concentrations at birth. Exceptions can and do occur rarely but need to be recognized in a timely fashion.
1. Maternal history suggestive of abnormal fluid and electrolyte status
a. Renal diseases with abnormal electrolytes
b. Diuretic therapy
c. Malnutrition or very abnormal diet
d. Oligohydramnios
2. Physical findings suggestive of abnormal electrolyte balance
a. Edema/anasarca
b. Ascites, abdominal/flank masses
c. Ambiguous genitalia
Laboratory
Usually, the neonate, even the very premature patient, does not need measurement of serum electrolytes immediately after birth. Initially, a neonate’s electrolytes and creatinine values should reflect the mother’s status. Patients with history or physical findings such as those mentioned may need to have an early evaluation of their electrolyte panel. Note that, in the face of normal placental and maternal renal function, a totally anephric neonate may have normal (ie, maternal) serum creatinine and sodium levels at birth.
1. Serum chemistries. These should be followed closely in all low birth weight (LBW) and sick patients in the NICU.
a. Serum sodium levels in neonates tend to be somewhat lower than in older children and adults, and not uncommonly, they will be in the range of 130 to 140 mEq/L. However, levels less than 130 mEq/L should be watched closely, and levels less than 120 mEq/L are associated with poor outcomes.
b. Serum potassium levels may be elevated in several conditions associated with hyponatremia (as discussed in the material that follows) and thus also should be followed.
c. Serum urea and creatinine are markers for renal dysfunction and should be followed; again, they will be normal initially if placental and maternal renal functions are normal.
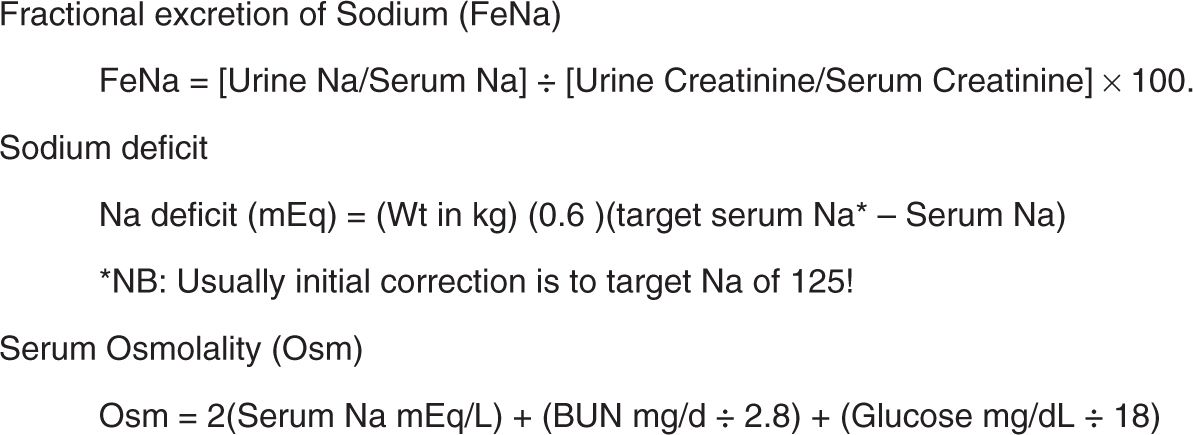
2. Urine chemistries. Urine sodium levels generally run below 30 mEq/L. We do not recommend routinely following urine chemistries, but they can be useful in determining the etiology of electrolyte abnormalities. Simultaneous urine creatinine determinations also can be useful for calculating the fractional excretion of sodium (FeNa) (see Figure 74-1).
3. Serum and urine osmolality.
4. Weights. Weights need to be checked daily at a minimum. Falling serum sodium with climbing weight suggests fluid retention; falling weight suggests sodium depletion.
FIGURE 74–1 Calculations for the fractional excretion of sodium. BUN, serum urea nitrogen.
Differential Diagnosis/Diagnostic Algorithm
Hyponatremia in the first days of life generally reflects only a few pathophysiologies:
1. Fluid (“free water”) overload. As discussed in Chapter 9, neonates are born with excess water that must be excreted. Because they are eunatremic at birth, this means that newborns also have a high total body sodium. However, the neonatal, particularly the premature, kidney has a limited ability to excrete a fluid load in the first few days of life. Thus, very early hyponatremia commonly is a problem of too much water and not too little sodium. Note that the chronic lack of thyroid hormone results in an inability to excrete a water load and thus can cause hyponatremia.
2. Increased sodium losses. Although unusual in the first few days, these can occur later in the NICU stay. Increased sodium losses can be caused by the following:
a. Renal losses (eg, diuretic therapy)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree