FIGURE 7-1 Macrodactyly of both the long and, less so, the index finger with divergence of the digits. An MRI of this patient revealed lipofibromatosis of the median nerve at the wrist extending distally to the common digital nerve and proper digital nerves of the index and long fingers.
CLINICAL QUESTIONS
- What causes digital and limb enlargement?
- Is macrodactyly a genetic condition?
- Are there associated malformations with digital or limb hypertrophy?
- What is the evaluation of a child with macrodactyly or limb hypertrophy?
- How is the clinical course monitored?
- What are the surgical indications?
- Which procedures are performed at which time?
- What are the expected outcomes from natural history and/or surgery?
THE FUNDAMENTALS
You and I do not see things as they are. We see things as we are.
—Herb Cohen
Unfortunately, people continue to expect other people to fit in a perceived social norm. This is particularly true of the appearance of the hands and upper limbs. Digital enlargement or entire limb overgrowth, if profound or progressive, can be a psychosocial issue for affected children, their parents, and families. Even the pseudoscientific, descriptive term “gigantism” evokes perceived horror or a circus-freak quality for macrodactyly and limb overgrowth. Such stigma is unfair and detrimental to these children
Enlargement of a limb does not necessarily make it less functional. If the motion and sensibility are normal, then the superhero-appearing limb functions quite well. However, if the enlarged digits or limbs are stiff, relatively insensate, painful, or weak, then function is impaired.
Etiology and Epidemiology
Increased vascular or neural supply will result in increased growth of all tissues (skin and soft tissues, muscles, and bones). Macrodactyly and limb hypertrophy are thus seen with lipofibrohamartomatous peripheral nerves (involving the median more commonly than ulnar nerves) and neu-rofibromatosis; vascular enlargement with arteriovenous fistulas, vascular malformations, and Klippel-Trenaunay syndrome; and lymphatic malformations. Increased bone and cartilage growth will result in macrodactyly, such as is seen with osteochondromatosis and Ollier enchondromatosis (see Chapters 47 and 49).1–4 Hemihypertrophy is a regional form of enlargement that can include part or all of one limb or the entire half of the body including the face. Hemihypertrophy can be associated with Wilms tumor. Enlargement can be due to congenital muscular hyperplasia of a limb.5 Limb hypertrophy can also be seen with more generalized syndromes such as Proteus or CLOVES.6–8 Aside from neurofibromatosis, which has an autosomal dominant inheritance, all of these conditions are sporadic and rare. Macrodactyly due to lipofibromatosis of the nerve is rare in all races but less common in non-Caucasians. Blacks have more macrodactyly of the foot than of the hand.9
Clinical Evaluation
The principles of clinical evaluation involve defining (1) the form of macrodactyly or limb hypertrophy, (2) whether the postnatal growth is proportional or progressive, and (3) the width and length of the affected part compared to expected adult growth. These days, the diagnosis is often made in utero by ultrasound.10 Otherwise, in most cases, it is obvious at birth. Serial exams with exact length and girth measurements are recorded yearly from diagnosis. Plain radiographs are obtained to assess osseous deformity, length of each bone, and physeal maturity compared to the opposite side. The use of magnetic resonance imaging (MRI) and computed tomography scans 11–13 provides definitive diagnosis by assessing fatty infiltration of lipofibromatous peripheral nerves, vascular anomalies, congenital muscular hyperplasia or anomalous muscles, and lymphatic malformations. With hemihypertrophy, a screening ultrasound is obtained for Wilms tumor. Electrodiagnostic studies are more sensitive than clinical exam in children for compressive neuropathy, a common complication of macrodactyly and limb hypertrophy.14,15
Flatt classified macrodactyly as: Type I is lipofibromatosis, type II is neurofibromatosis, type III is polyostotic, and type IV is hemihypertrophy. Lipofibromatosis has also been named lipofibroma hamartomatosis, macrodystrophia lipomatosa, and macrodactylia fibrolipomatosis, among others. The name signifies digital enlargement due to fat and fibrous infiltration in a peripheral nerve distribution, much more commonly in the median than the ulnar nerve (Figure 7-1).16,17 The index finger is most commonly involved, often in conjunction with the long finger or thumb. The dilation of the nerve often starts in the distal forearm and extends through the carpal canal and common digital nerve out to the proper digital nerve. The involved nerve has fatty infiltration and fibrosis. The bone often has altered architecture by biopsy with wide medullary canals and distorted trabeculae.18 The subcutaneous tissue is fibrotic. The skin is expansile with volar greater than dorsal, and distal greater than proximal, enlargement of skin and subcutaneous tissues.
Multiple digital involvement is more frequent than single digit. Unilateral hand involvement is most common. Syndactyly occurs in about 10% of cases. Asymmetric growth of each involved digit with angular and rotational malalignment is common and corresponds to the degree of proper digital nerve lipofibromatosis. The involved digit(s) often hyperextend and radially deviate due to more palmar and ulnar involvement. Flatt called these “banana fingers.” The growth can be progressive or proportional. With progressive enlargement, digital motion and function diminishes.
Sensibility by two-point discrimination and light touch measurements are, surprisingly, usually normal. However, compressive neuropathy can occur with loss of sensibility and motor function over time. This is usually due to a carpal tunnel syndrome14,15 but also has been described with lipofibromatosis of the ulnar nerve and cubital tunnel compression.19 Electrodiagnostic studies are often required due to limits of history and physical exam for carpal or cubital tunnel syndrome diagnosis in these children. There are children with lipofibromatosis of the median nerve who present with only a palpable mass in the distal forearm without macrodactyly. MRI and electromyography and nerve conduction velocity (EMG/NCV) studies are necessary for diagnosis. These lesions are usually monitored over time when the nerve is functioning normally since it is not a neoplasia. Neural decompression and carpal release are indicated if weakness and loss of sensibility develop.
Flatt’s other types of macrodactyly include neurofibromatosis, hemihypertrophy, and polyostotic forms. A syndromic class should be included with Proteus, CLOVES, and Klippel-Trenaunay syndromes, among others. In addition, congenital unilateral muscular hyperplasia is seen seindentte from hemihypertrophy. Vascular and lymphatic malformations will result in limb and/or digital enlargement. With all digits involved, upper limb and even truncal involvement, these conditions are more likely. MRI scan is used to define pathoanatomy and aid in diagnosis and treatment. Genetics consultation and multidisciplinary clinic evaluation and care are important in these situations.
Surgical Indications
The presence of macrodactyly or limb hypertrophy alone is not an indication for surgery. There is wide variation in clinical presentation. Some minor increases in size can be near normal in appearance and function. Alternatively, there are many instances of limb and/or digital hypertrophy that cannot be resolved or “normalized” even by surgical intervention. Often, care for these children is a case of managing expectations.
In the cases of lipofibromatosis of a major peripheral nerve, progressive deformity and loss of function are indications for surgical treatment. Options include (1) soft tissue debulking, (2) appropriately timed physeal arrests, (3) digital realignment (Figure 7-2), (4) bony reduction, (5) any combination of options (1) to (4), and (6) ray resection. Repeat surgery is common.20

FIGURE 7-2 X-ray of the index finger after debulking of radial-sided macrodactyly and corrective osteotomy of ulnar deviation deformity with pin fixation.
In terms of congenital muscular hyperplasia and certain forms of hemihypertrophy debulking of excessive and/or accessory muscles and soft tissues is indicated when digital malalignment becomes too problematic for proper hand function. Median nerve decompression in the carpal canal is indicated with loss of sensibility and thenar strength.
Neurofibromatosis and osteocartilaginous causes of macrodactyly and limb hypertrophy are discussed in Chapters 47 and 28.
SURGICAL PROCEDURES
 Nerve Decompression
Nerve Decompression
When these children or their parents complain of loss of manual dexterity, carpal tunnel syndrome should be suspected. As mentioned in the clinical evaluation section, nerve conduction and electromyographic electrodiagnostic studies are important for accurate diagnosis. If confirmed, nerve decompression should occur before irreversible neuromuscular changes occur.
The incision extends from distal forearm across palm. The median nerve and the adjacent muscles and tendons are identified proximally and isolated. With lipofibromatosis, the nerve is inspected closely with loupe or microscopic magnification. Dissection of the nerve extends from proximal to distal across the palm. The transverse carpal ligament is incised longitudinally along the ulnar border while protecting the ulnar nerve and palmar vascular arch exiting from Guyon canal and transversing the palm distal to the transverse carpal ligament. If the carpal tunnel release is part of a digital debulking procedure, the nerve is followed distally through the bifurcation of the common digital nerve(s) into the proper digital nerves of the affected digit(s). If this surgery is for congenital muscle hyperplasia or hemihypertrophy, the extrinsic and intrinsic muscular anatomy is defined by direct inspection and isolation. Often there is increased bulk or accessory muscles present. The increased inter-osseous bulk may be splaying the digital metacarpals, and the dynamic muscle imbalance may be responsible for digital malalignment. Resection of this redundancy is performed as necessary. The exact amount of resection is difficult to quantify. Similar resection of excessive skin and soft tissues is performed before tension-free closure in all these conditions.
In children and adolescents, we close the transverse carpal ligament with a Z-plasty. A second, partial longitudinal incision from distal to proximal is made in the ligament indentllel to the original ulnar longitudinal incision. This incision is carried proximally until the ligament can be rotated ulnarly for nonconstrictive coverage of the nerve. Care is taken to identify and protect the recurrent motor branch to the thenars during this incision. Remember, though this nerve is usually extraligamentous, it can course through the ligament. Also, though it usually branches from the median nerve distal to the transverse carpal ligament, it can also branch proximal to or under the ligament. The ligament is then rotated on its radial base adjacent to thenar muscle origins. It is repaired to the ulnar proximal base of the incised ligament for tension-free coverage. A Freer elevator should pass easily under the repaired ligament. This ligament reconstruction prevents bowstringing of the nerve and adherent scarring of the nerve directly to the skin and superficial subcutaneous tissues.
As mentioned, redundant skin and subcutaneous tissues are excised as necessary. The amount of resection is dependent on viability of the flaps with a tension-free closure. Deflation of the tourniquet is important to assess the vascularity of the soft tissues. A large compressive dressing is left in place for 2 weeks. Postoperative therapy is critical to regain full wrist and digital mobility.
If the nerve compression syndrome occurs in any other anatomic location, such as the ulnar nerve at the elbow, similar principles of nerve decompression are followed.
Progressive macrodactyly can be disfiguring and dysfunctional. If the decision is made with the parents to preserve the digit, then repeated and/or sequential soft tissue debulking operations are usually necessary Unfortunately like a digital replant, once down that road, there is no turning back Flap necrosis, digital ischemia, and neural impairment are risks with excessive resection in any one procedure. Long-term stiffness is possible from repeated surgeries. Remember, soft tissue debulking will reduce the circumference and width but not the longitudinal growth or size. Reduction in length will require timely restriction of growth by epiphysiodesis or acute shortening by bony reduction. Digital malalignment that affects function will require osteotomy. Bone and soft tissue reduction and realignment can be done in conjunction or seindenttely. Remember, each surgical intervention carries an increased risk of loss of motion and scar problems, so more comprehensive surgical care in one setting is best as long as the complication risk does not increase. Complex combined soft tissue and bony reduction procedures cross over into the double black diamond category of surgeons, so beware. This section will cover debulking of soft tissues alone.
The optimal case for soft tissue reduction is marked increase in girth but equivalent length to the same digit of the contralateral hand and appropriate length for digital cascade of the affected hand (Figure 7-3A). The goal of the surgery is a more normal-appearing digit that maintains mobility. A Z-plasty midaxial incision is utilized over the involved digital nerve. This allows for appropriate resection and easy insetting of flaps (Figure 7-3B). Elevation of the redundant skin and subcutaneous flaps is performed while protecting the underlying neurovascular bundle (NVB). The nerve is generally quite large and tortuous. The artery is often compressed by the abnormal fibrous stroma. Preserving the digital artery is a delicate dissection. The amount of tissue resection is limited by concerns of digital and flap viability (Figure 7-3C). Like constriction ring excision and flap rotation, about 270 degrees of digital circumference is safe in one procedure. The opposite (NVB) is usually left in situ without dissection. A decision has to be made regarding the lipofibrohamartomatous digital nerve. It can be left in situ, carefully debulked under the microscope leaving longitudinal fascicles, or excised. Surprisingly, all options seem to leave normal digital light and two-point discrimination sensibility. At the first reconstruction, we usually leave it intact or debulk it. However, if it is clear that it is a large, convoluted bundle of scar and it distorts digital size, we boldly excise it leaving the artery intact. Excision of redundant skin and subcutaneous tissue is performed to allow for tension-free closure (Figure 7-3D). There may be some additional trimming of Z-plasty edges to get it right where you want it. This tinkering does count in finding the fine line between flap necrosis and inadequate debulking. Postoperative casting is used for 2 weeks, followed by rapid mobilization and scar management with hand therapy. Preventing loss of digital motion is imperative.
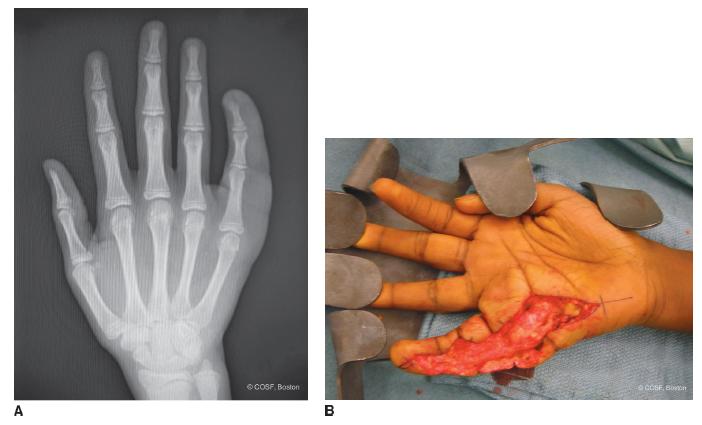
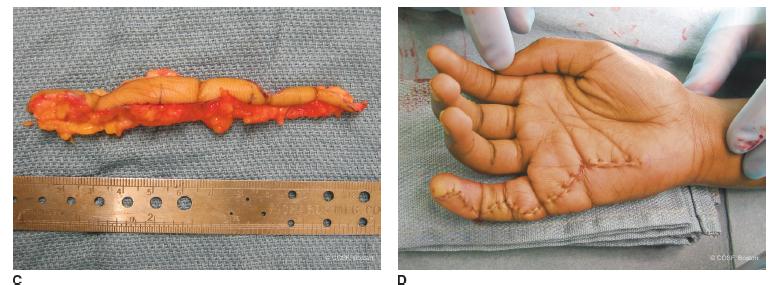
FIGURE 7-3 A: X-ray of macrodactyly of small finger with proportionate length but girth increased due to involvement of ulnar digital nerve lipofibromatosis. There is mild radial deviation of the digit present. B: Z-plasty midaxial incision for debulk-ing procedureC: Resected skin and fat. D: Z-plasty closure after debulking. In this case, the nerve was debulked and preserved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Debulking Procedures
Debulking Procedures