Background
Choice of delivery route after previous cesarean delivery can be difficult because both trial of labor after cesarean delivery and elective repeat cesarean delivery are associated with risks. The major risk that is associated with trial of labor after cesarean delivery is uterine rupture that requires emergency laparotomy.
Objective
This study aimed to estimate the occurrence of uterine rupture during trial of labor after cesarean delivery when lower uterine segment thickness measurement is included in the decision-making process about the route of delivery.
Study Design
In 4 tertiary-care centers, we prospectively recruited women between 34 and 38 weeks of gestation who were contemplating a vaginal birth after a previous single low-transverse cesarean delivery. Lower uterine segment thickness was measured by ultrasound imaging and integrated in the decision of delivery route. According to lower uterine segment thickness, women were classified in 3 risk categories for uterine rupture: high risk (<2.0 mm), intermediate risk (2.0–2.4 mm), and low risk (≥2.5 mm). Our primary outcome was symptomatic uterine rupture, which was defined as requiring urgent laparotomy. We calculated that 942 women who were undergoing a trial of labor after cesarean delivery should be included to be able to show a risk of uterine rupture <0.8%.
Results
We recruited 1856 women, of whom 1849 (99%) had a complete follow-up data. Lower uterine segment thickness was <2.0 mm in 194 women (11%), 2.0–2.4 mm in 217 women (12%), and ≥2.5 mm in 1438 women (78%). Rate of trial of labor was 9%, 42%, and 61% in the 3 categories, respectively ( P <.0001). Of 984 trials of labor, there were no symptomatic uterine ruptures, which is a rate that was lower than the 0.8% expected rate ( P =.0001).
Conclusion
The inclusion of lower uterine segment thickness measurement in the decision of the route of delivery allows a low risk of uterine rupture during trial of labor after cesarean delivery.
In the last 3 decades, the rate of cesarean deliveries has been rising continuously worldwide and has reached >30% in many countries. A major contributor to this trend is the concomitant decline in the percentage of trial of labor after cesarean delivery (TOLAC) and vaginal birth after cesarean delivery (VBAC). Fear of intrapartum uterine rupture, a rare (0.4–1.1%) but potentially catastrophic complication of TOLAC, represents the main reason for this trend. Uterine rupture can lead to perinatal asphyxia or death and severe maternal complications. The alternative for TOLAC is to perform an elective repeat cesarean delivery (ERC). ECR will reduce the risk of uterine rupture but can also be associated with risks of short-term maternal complications, such as hemorrhage, hysterectomy, thromboembolism, and neonatal complications that include respiratory distress syndrome. In addition, cesarean delivery is associated with a higher risk of longer term complications, such as placenta praevia and accreta in future pregnancies. Therefore, the selection of the good candidate who is at low risk for uterine rupture during TOLAC is crucial.
Assessment of lower uterine segment (LUS) thickness by ultrasound imaging in the third trimester of pregnancy has been proposed to predict the risk of uterine rupture. A landmark study by Rozenberg et al showed that the risk of a defective scar at delivery (uterine scar dehiscence and uterine rupture) is related directly to the degree of thinning of the LUS. They reported a risk of uterine scar defect at delivery of 16% of women when the LUS thickness was <2.5 mm compared with 0.7% when the thickness was 3.5 mm or more. More recently, a LUS thickness of <2.3 mm was identified as a significant risk factor for uterine rupture. Although meta-analyses report no LUS thickness cut-off that can predict all uterine ruptures, most authors agree that the risk is high when the LUS thickness is <2.0 mm.
We aimed to evaluate the occurrence of uterine rupture when LUS thickness measurement was included in the decision about delivery route in a large cohort of women who wanted to attempt TOLAC.
Materials and Methods
Study design and participants
We conducted a prospective cohort study between April 2009 and June 2013 in 3 Canadian Hospitals (Centre Hospitalier Universitaire de Québec, Québec; Centre Hospitalier Universitaire Sainte-Justine, Montreal; Centre Hospitalier Universitaire Fleurimont, Sherbrooke) and a Swiss Hospital (Hôpitaux Universitaires de Genève, Geneva). We recruited women who were contemplating a TOLAC with a single previous low-transverse cesarean delivery and a singleton pregnancy in cephalic presentation. The likelihood of VBAC and the risk of uterine rupture were evaluated and discussed between 34 weeks 0 days and 38 weeks 6 days of gestation.
Procedures
After informed consent was obtained from the participant, a research nurse or midwife recorded maternal characteristics and medical and reproductive history, including the features of the previous cesarean delivery. Body mass index was calculated with the use of the maternal weight at inclusion (end of pregnancy). Tobacco use was considered when the woman was currently smoking. Diabetes mellitus included gestational and pregestational diabetes mellitus. Previous cesarean delivery that was performed for labor dystocia, cephalopelvic disproportion, descent arrest, or failure to progress was reported as previous cesarean delivery for recurrent reason.
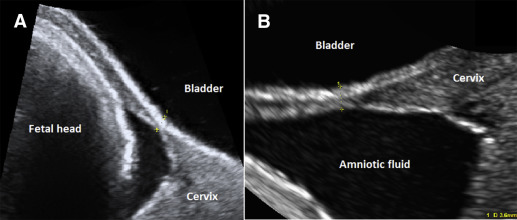
Examination of the LUS was performed with transabdominal and transvaginal ultrasound imaging with Voluson Expert or Voluson E8 (GE Healthcare, Milwaukee, WI) between 34 weeks 0 days and 38 weeks 6 days of gestation by a trained sonographer or midwife who was supervised by a maternal-fetal medicine specialist in each center. At least 6 measurements (3 transabdominal and 3 transvaginal) of the LUS thickness were performed, with the use of the method previously described ( Figure ). The thinnest LUS value was retained. Fetal biometry (head circumference, biparietal diameter, abdominal circumference, femur length) was measured to estimate fetal weight with the use of the Hadlock formula. According to LUS thickness, women were classified in 3 risk categories for uterine rupture during TOLAC: high risk (<2.0 mm), intermediate risk (2.0–2.4 mm), and low risk (≥2.5 mm). Participants and their health care providers were informed of the risk category. All participants met with the obstetrician after the LUS assessment. During this consultation, each woman was informed about her risk of uterine rupture during TOLAC according to LUS thickness (average of 0.5–1%, most likely >1% when LUS is <2.0 mm and most likely <0.5% when LUS thickness is ≥2.5 mm); the consequences of uterine rupture (including perinatal asphyxia and death), the maternal and neonatal complications of ECR, and the chances of successful VBAC based on the indication of previous cesarean delivery (recurrent or not), previous vaginal birth, and estimated fetal weight. Finally, women were informed that mode of delivery would be discussed again in case of induction of labor or in case of labor dystocia. The institutional ethics committee in each center approved the study. Medical records were reviewed for obstetric and neonatal outcomes after delivery.
Our primary outcome was symptomatic uterine rupture, defined as a complete separation of the uterine scar that resulted in protrusion of fetal or placental parts in the peritoneal cavity and required urgent laparotomy. Secondary outcomes included incidental scar disruption (complete opening of the previous scar without protrusion of fetal or placental parts in the peritoneal cavity) and uterine scar dehiscence (defined as a small window in the LUS) that was diagnosed during cesarean delivery. A routine manual revision of the LUS integrity was not performed after vaginal birth.
Other secondary outcomes included the rates of TOLAC and VBAC, maternal outcomes (postpartum hysterectomy, blood transfusion, and maternal death), neonatal outcomes (5-minute Apgar score <7, cord blood pH <7.0, perinatal asphyxia [defined as a 5-minute Apgar score <4, a cord blood pH <7.0 when available], and evidence of altered neurologic status, and/or multisystem organ failure), and intrapartum or neonatal death.
Statistical analysis
Labor and delivery characteristics and uterine scar defects were reported according to LUS thickness categories (<2.0 mm, 2.0–2.4 mm, and ≥2.5 mm). Neonatal and maternal outcomes were stratified according to intended mode of delivery. We estimated that the use of the LUS thickness could result in a low risk of uterine rupture in women who undergo TOLAC. We calculated that a minimum of 942 women who underwent a TOLAC should be included to exclude the value of 0.8% from our estimate of the risk of uterine rupture (1-sided test; α=.05; power=0.80) should the observed risk be 0.2%. We estimated that a minimum of 1450 women who were contemplating VBAC would need to be recruited to have at least 942 (65%) women who would choose to attempt TOLAC. Statistical analyses were performed with SPSS software (version 22.0; SPSS Inc, Chicago, IL). We calculated the confidence interval for proportions using the Fisher exact method and tested the statistical significance of the observed proportion compared with 0.8% using the method of the normal approximation of the binomial distribution.
Results
We recruited 1856 women, of whom >99% (n=1849) had complete follow-up data. Participant’s characteristics are described in Table 1 . LUS thickness was <2.0 mm in 194 women (11%), between 2.0–2.4 mm in 217 women (18%), and ≥2.5 mm in 1445 women (78%). All 7 women who were lost to follow up had a LUS thickness ≥2.5 mm and had similar characteristics as the others. We observed that women who were recruited in the center with most recruitment (Centre Hospitalier Universitaire de Québec [CHUQ]) were more likely to have a LUS <2 mm (13% vs 5%, 6% and 9%, respectively; P <.001) or 2.0–2.4 mm (15% vs 7%, 5% and 9%, respectively; P <.001).
| Patients characteristics | All (n=1856) | <2.0 mm (n=194) | 2.0-2.4 mm (n=217) | ≥2.5 mm (n=1445) |
|---|---|---|---|---|
| Maternal age, y a | 31.5 ± 4.3 | 31.6 ± 4.4 | 31.3 ± 3.7 | 31.6 ± 4.4 |
| Body mass index, kg/m 2 a | 29.2 ± 5.2 | 27.7 ± 4.1 | 28.6 ± 4.9 | 29.5 ± 5.3 |
| Tobacco use, n (%) | 149 (8) | 12 (6) | 26 (12) | 111 (8) |
| Diabetes mellitus (pregestational or gestational), n (%) | 144 (8) | 11 (6) | 16 (7) | 117 (8) |
| Previous vaginal delivery, n (%) | 305 (16) | 16 (8) | 46 (21) | 243 (17) |
| Interdelivery interval, mo a | 44.1 ± 31.3 | 39.7 ± 24.3 | 46.7 ± 33.8 | 44.3 ± 31.7 |
| Previous cesarean delivery for recurrent reason, n (%) | 766 (41) | 39 (20) | 57 (26) | 670 (46) |
| Gestational age at sonography, wk a | 36.6 ± 1.7 | 36.7 ± 0.8 | 36.8 ± 0.8 | 36.6 ± 1.9 |
| Estimated fetal weight, g a | 2999 ± 396 | 2920 ± 355 | 2997 ± 375 | 3010 ± 403 |
| Lower uterine segment thickness, mm a | 3.3 ± 1.3 | 1.6 ± 0.3 | 2.2 ± 0.2 | 3.7 ± 1.1 |
| Centers, n (%) | ||||
| Centre Hospitalier Universitaire (Quebec) | 1081 (58) | 139 (72) | 164 (76) | 778 (54) |
| Ste-Justine Hospital (Montreal) | 340 (18) | 16 (8) | 16 (7) | 308 (21) |
| Centre Hospitalier Universitaire (Sherbrooke) | 63 (3) | 4 (2) | 3 (1) | 56 (4) |
| Hôpitaux Universitaires de Genève (Geneva) | 372 (20) | 35 (18) | 34 (16) | 303 (21) |
Labor characteristics and delivery outcomes are reported in Table 2 . LUS thickness measurement had a significant impact on the choice of intended mode of delivery; women with a thin LUS were more likely to undergo ERC. We did not observe any case of symptomatic uterine rupture in the entire cohort (0%; 95% confidence interval, 0.0–0.4%). No case of 984 TOLACs was significantly <0.8%, which was the expected risk ( P =.0001). Three cases of incidental scar disruption without adverse perinatal outcomes were reported in 3 women who underwent repeat cesarean delivery for labor dystocia after TOLAC. All 3 women had no progression of cervical dilation or no progression of fetal descent for >2 hours before the cesarean delivery was performed. Uterine scar dehiscence was observed in 22 other women who underwent TOLAC. Looking specifically at women who underwent repeat cesarean delivery during labor, uterine scar defects of any type (incidental scar disruption or uterine scar dehiscence) were observed more frequently in women with a LUS of 2.0–2.4 mm.



