Background
Twin pregnancies are at increased risk for perinatal morbidity and death because of many factors that include a high incidence of preterm delivery. Compared with singleton pregnancies, overall perinatal risk of death is higher in twin pregnancies; however, for the preterm period, the perinatal mortality rate has been reported to be lower in twins.
Objective
The purpose of this study was to compare perinatal mortality rates in relation to gestational age at birth between singleton and twin pregnancies, taking into account socioeconomic status, fetal sex, and parity.
Study Design
We studied perinatal mortality rates according to gestational age at birth in 1,502,120 singletons pregnancies and 51,658 twin pregnancies without congenital malformations who were delivered between 2002 and 2010 after 28 weeks of gestation. Data were collected from the nationwide Netherlands Perinatal Registry.
Results
Overall the perinatal mortality rate in twin pregnancies (6.6/1000 infants) was higher than in singleton pregnancies (4.1/1000 infants). However, in the preterm period, the perinatal mortality rate in twin pregnancies was substantially lower than in singleton pregnancies (10.4 per 1000 infants as compared with 34.5 per 1000 infants, respectively) for infants who were born at <37 weeks of gestation; this held especially for antepartum deaths. After 39 weeks of gestation, the perinatal mortality rate was higher in twin pregnancies. Differences in parity, fetal sex, and socioeconomic status did not explain the observed differences in outcome.
Conclusion
Overall the perinatal mortality rate was higher in twin pregnancies than in singleton pregnancies, which is most likely caused by the high preterm birth rate in twins and not by a higher mortality rate for gestation, apart from term pregnancies. During the preterm period, the antepartum mortality rate was much lower in twin pregnancies than in singleton pregnancies. We suggest that this might be partially due to a closer monitoring of twin pregnancies, which indirectly suggests a need for closer surveillance of singleton pregnancies.
Twin pregnancies are at increased risk for preterm birth, intrauterine growth restriction, and a number of multiplet-related conditions. Monochorionic twins have additional risks for death and morbidity, primarily because of the twin-to-twin transfusion syndrome and congenital abnormalities.
Although registry data in Western countries (Euro-Peristat) confirm a crude 2- to 3-fold increased perinatal risk of death in a twin pregnancy, only few reports have compared mortality and morbidity rates between twin and singleton pregnancies by taking into account differences in gestational age at delivery. They all found a lower perinatal mortality rate in twins who were born at <37 weeks of gestation. These studies were all small, with the exception of 1 (Kahn et al ), and did not include separation between zygosity and chorionicity in twins, nor did they take into account known prognostic important factors such as parity and socioeconomic status (SES) of the mother and sex of the child.
The objective of this study was to compare perinatal mortality rates in relation to gestational age at birth between singleton and twin pregnancies, taking into account parity, SES, fetal sex and mode of delivery. For this study, we used a large national anonymized data set from The Netherlands Perinatal Registry.
Materials and Methods
General
This was a retrospective population-based cohort study. We obtained, after previous permission from The Netherlands Perinatal Registry (Perined), aggregated data and analyses on all births in The Netherlands from 2002–2010. This registry contains information on approximately 95% of all births from 16.0 weeks of gestational age onwards, where coverage of twins is even higher. Details of this dataset can be found elsewhere.
Variables
The Perined dataset includes routine maternal data on age, parity, socioeconomic background (zip-code based), and ethnic background. Information is available on intervention (induction of labor, mode of delivery [instrumental, elective, and emergency cesarean]), neonatal intensive care unit admission of the child, and specific features of the delivery.
Data on the child comprise singleton or multiplet, sex of the child, presence of congenital anomalies, gestational age at birth, birthweight, and Apgar score at 5 minutes. From birthweight, sex, and gestational age, the birthweight is computed as a percentile score.
Data are recorded on the size of the multiplet and for each child its rank number at birth. No information is available on zygosity/chorionicity. Congenital abnormalities were recorded if they were present and recognized either at birth or at first neonatal intensive care unit admission by the neonatologist and include any abnormality already noticed during antenatal ultrasound scanning or, occasionally, with genetic tests. All children with congenital abnormalities were excluded. Gestational age was calculated from the first day of the last menstrual period or from an ultrasound dating scan by measurement of the crown-rump length in the first trimester. In this period, 91% of the pregnancies had a reliable dating, which was obtained by a first-trimester dating scan. For twins conceived spontaneously, dating was based on the mean crown-rump length measurement of both fetuses. Pregnancies that were achieved by assisted reproductive technology were dated based on the assisted reproductive technology–derived gestational age.
In this report a gestational age of 37 weeks means 37 weeks+0 days to 37 weeks+6 days containing whole-week groups. For this analysis, births between 28+0 and 43+6 weeks of gestation were included, to allow comparison with data from other countries in which registration practices may differ at earlier gestational ages. Children with missing gestational age at birth were excluded from the analysis. A total of 1839 children from a twin pregnancy were excluded because a twin pair could not be linked or information on congenital malformations or gestational age of 1 of the twins was missing. In this group, there were 42 perinatal deaths. If 1 of the twins died at <28 weeks of gestation, both children were excluded from analysis. If 1 of the twins died at >28 weeks of gestation and the pregnancy continued for the benefit of the other twin, the gestational age at birth was registered for both twins; the exact gestational age of death for the dead twin was not available in this database.
Perinatal mortality rate was defined as fetal or neonatal death up to 7 days after birth; antepartum death was defined as death that occurred before labor; intrapartum death was defined as death during labor, and neonatal death was defined as death that occurred within 0–7 days after live birth. This information is always available in all cases.
Statistical analysis
Perinatal mortality rate was expressed as rate (number of deaths per 1000 infants, including stillbirths). Mortality rate was subdivided to time of occurrence: antepartum, intrapartum, and neonatal. Perinatal mortality rate was compared between singleton and twin pregnancies, according to gestational age. The mortality rates at 42 and 43 weeks of gestation were not displayed because of the extremely small number of cases. Comparisons were made between groups with the use of multivariate logistic regression with gestational age in the model or chi-square test.
The mode of delivery in singleton and twin pregnancies was studied. Vaginal delivery was divided in spontaneous vaginal delivery and instrumental delivery and defined as delivery by forceps or a vacuum device. Cesarean delivery was divided into planned cesarean section, which was defined as a scheduled or elective cesarean delivery, and an emergency cesarean, which was defined as any cesarean delivery that was not planned or scheduled.
To investigate the influence of parity, maternal SES, and child sex, we calculated perinatal mortality rates for each parameter for twin and singleton pregnancies: parity (0 vs ≥1), SES (p<20 poor vs p>20), and child sex (male/female). For classification of SES, the “socioeconomic status score” was used as a proxy. This score takes into account the average income per household in a given 4-digit postal code area and the percentage of households with low income, without paid job, and with low education level. The level of SES was categorized as low if the score was <20th percentile.
No information on zygosity was available in the data set. The only information we could obtain on zygosity indirectly were the twin pairs with unequal gender; male-female twins are per definition dizygotic and dichorial.
Results
We studied 1,502,120 singleton infants and 51,658 twin infants who were born from 2002–2010 after 28 weeks of gestation. In singleton pregnancies, there were 6,087 perinatal deaths (4.1/1000). For twins, a total of 340 deaths occurred that resulted in a perinatal mortality rate of 6.6 per 1000 infants. The perinatal mortality rate according to gestational age is shown in Table 1 .
| Gestational age, wk | Singleton pregnancies | All twin pregnancies | Dizygotic twin pregnancies (unequal gender) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total deaths, n | Total infants, n | Perinatal mortality rate within the week | Total deaths, n | Total infants, n | Perinatal mortality rate within the week | Total deaths, n | Total infants, n | Perinatal mortality rate within the week | |
| 28 | 326 | 1,443 | 225.92 | 15 | 406 | 36.95 | 1 | 96 | 10.42 |
| 29 | 308 | 1,718 | 179.28 | 23 | 592 | 38.85 | 5 | 174 | 28.74 |
| 30 | 278 | 2,285 | 121.66 | 22 | 730 | 30.14 | 3 | 208 | 14.42 |
| 31 | 275 | 2,899 | 94.86 | 16 | 1,048 | 15.27 | 4 | 362 | 11.05 |
| 32 | 285 | 4,130 | 69.01 | 21 | 1,666 | 12.61 | 11 | 510 | 21.57 |
| 33 | 289 | 6,337 | 45.61 | 22 | 2,496 | 8.81 | 4 | 773 | 5.17 |
| 34 | 309 | 10,732 | 28.79 | 41 | 3,900 | 10.51 | 9 | 1,270 | 7.09 |
| 35 | 350 | 17,319 | 20.21 | 42 | 5,088 | 8.25 | 14 | 1,783 | 7.85 |
| 36 | 371 | 33,999 | 10.91 | 47 | 8,088 | 5.81 | 15 | 2,684 | 5.59 |
| 37 | 530 | 85,521 | 6.20 | 42 | 13,588 | 3.09 | 19 | 5,102 | 3.72 |
| 38 | 648 | 215,586 | 3.01 | 25 | 9,374 | 2.67 | 8 | 3,621 | 2.21 |
| 39 | 720 | 357,042 | 2.02 | 15 | 3,502 | 4.28 | 4 | 1,377 | 2.90 |
| 40 | 696 | 420,017 | 1.66 | 8 | 1,039 | 7.70 | 1 | 415 | 2.41 |
| 41 | 567 | 274,563 | 2.07 | 1 | 129 | 7.75 | 0 | 59 | 0.00 |
| 42 | 134 | 67,638 | 1.98 | 0 | 10 | 0.00 | 0 | 4 | 0.00 |
| 43 | 1 | 891 | 1.12 | 0 | 2 | 0.00 | 0 | 0 | 0.00 |
| Total | 6087 | 1,502,120 | 4.05 | 340 | 51,658 | 6.58 | 98 | 18,438 | 5.32 |
Of all twins, 46% were born at <37 weeks of gestation, in contrast to only 5% in the singletons. For deliveries at <37 weeks of gestation, the perinatal mortality rate in twins was 10.4 per 1000 infants compared with 34.5 per 1000 infants in singletons. For infants who were born at <34 weeks of gestation, mortality rates were 17.2 per 1000 infants in twins and 93.6 per 1000 infants in singletons.
In singleton pregnancies, perinatal mortality rate decreased with increasing gestational age, with the lowest mortality rate at 40 weeks of gestational age. In twin pregnancies, mortality rates also decreased with increasing gestational age, with the lowest mortality rate at 38 weeks of gestation and an increase thereafter ( Figure 1 ). In the preterm period, the perinatal mortality rate in twin pregnancies was substantially lower than in singleton pregnancies. After 39+0 weeks, the mortality rate was higher in twin pregnancies.
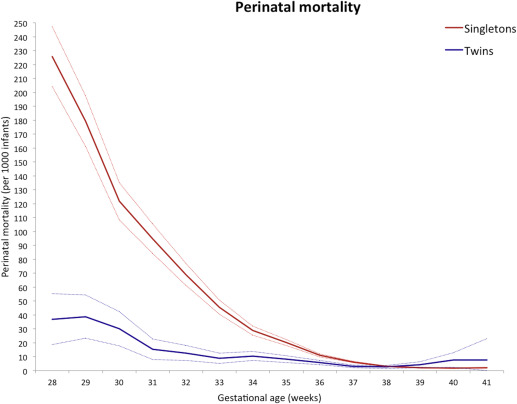
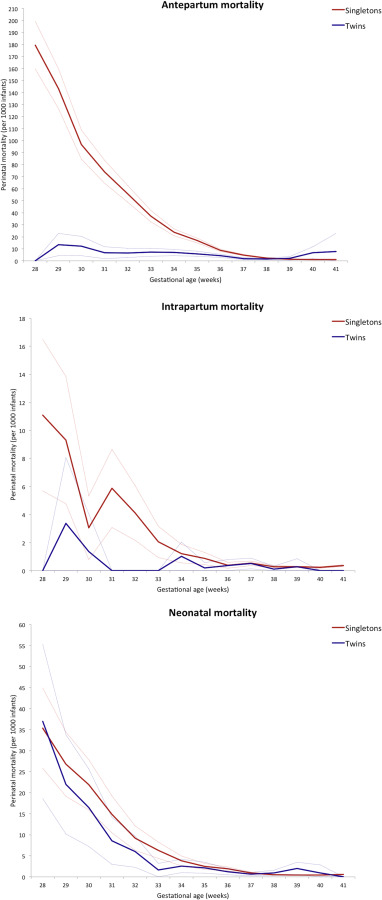
Figure 2 shows the perinatal mortality rate according to time period of occurrence of death. In both singleton and twin pregnancies, most perinatal deaths occurred in the antepartum period, followed by the neonatal period and the intrapartum period, respectively. In singleton pregnancies, the distribution of the time period of death was 72% antepartum, 9% intrapartum, and 19% neonatal; for twin pregnancies, this distribution was 59% antepartum, 6% intrapartum, and 35% neonatal. Antepartum mortality was significantly lower in twin pregnancies as compared with singleton pregnancies during the whole preterm period ( P <.001). After 40 weeks of gestation, antepartum mortality rates were significantly higher for twin pregnancies ( P =.02). The intrapartum mortality rate was significantly lower from 31–33 weeks of gestation but did not differ in the term period. The neonatal mortality rate was more or less similar during the whole preterm period; mortality rates were higher for twin pregnancies in the term period. Twins were more often delivered by cesarean section than singletons ( Table 2 ).
| Delivery mode | Singleton pregnancies | All twin pregnancies | P value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Spontaneous | 1.129.542 | 75.20 | 26.628 | 51.55 | <.001 |
| Instrumental | 153.354 | 10.21 | 5.006 | 9.69 | .23 |
| Planned cesarean | 95.792 | 6.38 | 10.720 | 20.75 | <.001 |
| Emergency cesarean | 120.141 | 8.00 | 9.171 | 17.75 | <.001 |
| Unknown | 3.291 | 0.22 | 133 | 0.26 | .92 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


