Low-Force Specific Upper Cervical: Atlas Orthogonal for Infants and Children
Laura Sheehan
In the early part of the 20th century, the first pioneer of atlas (C1) adjusting was Dr. B.J. Palmer. He had medical doctors and chiropractors evaluate patients who had flown in from around the world in the clinic in Davenport, Iowa, with numerous tests, including neurological and orthopedic exams, lab values, and x-rays. The atlas (C1 vertebrae) position was evaluated by motion palpation as well as x-ray. A high-force vectored adjustment was given on a knee chest table to the patient’s posterior arch of C1. Then, all exam procedures were repeated including new comparison x-rays of the cervical, thoracic, and lumbar regions. He observed significant changes, which revealed that many systems of the body were affected by the alignment and repositioning of this important area of the spine (1).
Over time, other chiropractors, like Dr. John F. Grostic, who studied with Palmer, further advanced the analysis and treatment of atlas subluxations in the early 30s (1).
Grostic developed a low-force, three-dimensional chiropractic adjustment, that is vectored, and in which corrections can be duplicated with high reliability. Orthospinology, Atlas Orthogonality, and NUCCA evolved from his work through his students. Dr. Roy Sweat founded Atlas Orthogonal (AO) in the mid-1980s and invented an x-ray system with a C-arm and the Atlas Orthogonal Precision Adjusting Instrument. There are many other upper cervical techniques: HIO, modified Toggle, Grostic, Blair, Knee Chest Table, and Applied Biophysics, to name a few. This chapter discusses the basics of the Atlas Orthogonal procedure.
The case studies presented utilize a straightforward AO protocol. X-rays are always utilized in the Atlas Orthogonal program (2).
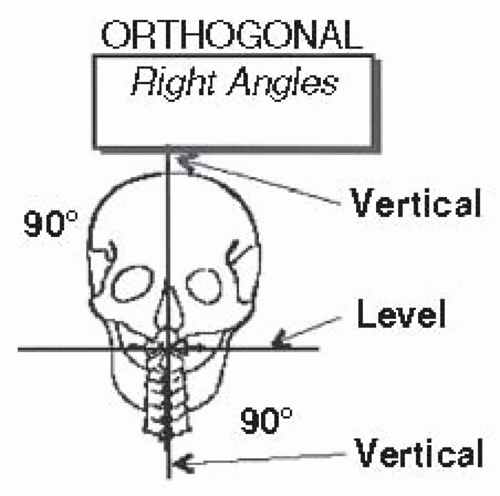
There are minor variations in x-ray procedures from NUCCA as well as nomenclature of the radiographs and subluxation types, but they are the closest allies to AO. The Grostic technique and NUCCA stand apart in their adjustment approach as it is done by hand. The adjustment in the AO program is done with a table model instrument or a handheld spring-loaded instrument. Orthogonal is an adjective having to do with or involving right angles, mutually perpendicular. It is based on the right-handed cartesian system (Fig. 33-1A,B).
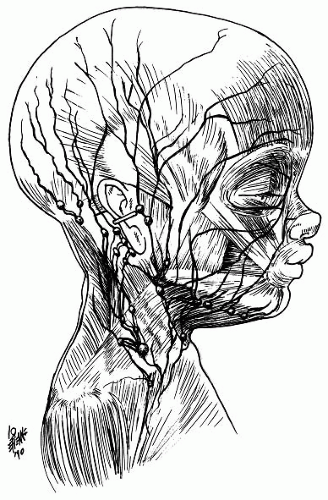
“The cranium should be vertical over the neck, the atlas should be level, and the cervical spine should be vertical to be in an optimal and neurologically sound Orthogonal position (2)” (Fig. 33-2). Other differences in the orthogonal program are palpation of the C1 and C2 dorsal nerve roots that are near the surface of the skin at the back of the neck just under the occiput and are palpable only at these two levels (Fig. 33-3).
THE DEVELOPMENT OF UPPER CERVICAL EVALUATION
In the low-force, vectored upper cervical techniques, it became important for the originators to develop an accurate and reproducible way to determine the atlas plane line in relation to the upper central skull line and the cervical spine. Atlas laterality (±ΘZ) is determined by their relationship. The inferior attachments of the posterior arch of the lateral masses were chosen where they intersected the posterior arch because these are primary growth centers and are the most reliable. Transverse processes vary greatly in size and are rarely symmetrical. The inferior aspect of the transverse process of C1 was chosen over the superior because of the position of the vertebral artery and any anomalies associated with it (2,3).
The adjusting equipment is a head mounted with a solenoid inside, hitting the stylus creating a mechanical
compressional wave with a force of 5 lbs at 1/20 of a second in orthogonal procedures, which are generally not even felt by the patient. The orthogonal stylus is thin (narrower in circumference than a pencil), cylindrical, and composed of an alloy metal to ensure a consistent transmission. The proper material and firmness of the headpiece is thought to be essential for a successful atlas correction. The mastoid support of the headpiece needs to be quite firm so that the mastoid resting just above the edge can allow the atlas easier movement with which to change position once the compressional wave is released into the stylus (4).
compressional wave with a force of 5 lbs at 1/20 of a second in orthogonal procedures, which are generally not even felt by the patient. The orthogonal stylus is thin (narrower in circumference than a pencil), cylindrical, and composed of an alloy metal to ensure a consistent transmission. The proper material and firmness of the headpiece is thought to be essential for a successful atlas correction. The mastoid support of the headpiece needs to be quite firm so that the mastoid resting just above the edge can allow the atlas easier movement with which to change position once the compressional wave is released into the stylus (4).
 FIGURE 33-1 A,B: Right-handed cartesian system and screw rotation. Drawing from Atlas Orthogonal Program, Module I-IV, R.W. Sweat Foundation. |
When the AO correction vectors are calculated, the leg length balance is checked, and neurological scanning is performed at the C1 and C2 nerve roots. If these parameters are in agreement, then the atlas correction goes forward and the headpiece is set at a specific height and angle. The patient is placed on the mastoid support, and adjustment factors are set up on the AO instrument. The shoulder is placed in order to enhance the correction. The compression wave is then released into the stylus.
EXAMINATION
Palpation of the First and Second Cervical Nerve Roots
Palpation of the pediatric patient in infancy can be done with the infant held in the parent’s lap, seated with one hand supporting the chest. The other hand supports the back. The practitioner will support the head. Another
approach for the newborn is the supine position resting on the adjusting bench. If the child is supine, lighter palpation should occur because muscle tension will be minimal in a supine position.
approach for the newborn is the supine position resting on the adjusting bench. If the child is supine, lighter palpation should occur because muscle tension will be minimal in a supine position.
A child over the age of 4 months can sit to have his or her neck lightly palpated. Upon inspection, one may notice contracted muscles in the upper neck, which are usually unilateral. The doctor will approach the back of the head with the pad of the first digit of his or her palpating hand sliding down from the occiput to the first dorsal rami under the occiput. The thumb is placed opposite the index finger just under the occiput to gently palpate the dorsal rami of C1 (Fig. 33-4). Then, sliding down to C2, the largest spinous in the neck, just slightly lateral and inferior from the C1 nerve roots, the C2 nerve roots may be palpable. The AO procedure is done by first palpating the first and second nerve roots, which are not palpable anywhere else in the cervical spine (2,3,5).
In a prone infant, this tiny area can be palpated with the fifth digit pad and is easily missed if the practitioner is anatomically unfamiliar with this region. A swollen dorsal rami feels similar to a tiny nodule or jelly bean under the skin and can be painful or tender by palpation. Extra care should be taken in this delicate area on infants and children as they do not always have the usual muscle hypertonicity that adults do to protect their nerve roots.
If the C1 segment is subluxated, there may be a palpable nodule felt under the occiput just lateral to the rectus capitus posterior major muscle. At the next caudal level, C2 may be palpable and tender just lateral to the C1 nerve root and will typically have a larger nodule than C1. In an infant, the nodule may be only the size of a tip of a pencil or a small pea. In the adult, it may feel pea-sized or like a marble. It is important to not confuse this finding with inflamed lymph nodes, which are much more lateral on the neck (Fig. 33-5). One interexaminer reliability study of adult patients has been done regarding palpation of the upper cervical spine, which found 97% agreement among palpators (6).
CHECKING FOR LEG LENGTH INEQUALITY
In the AO program, the doctor touches the feet minimally so as to not introduce tension or energy into the legs. Requiring the patient to wear shoes, the legs should be flat and the heels and ankles should hang over the end of the table. A grid at the end of the table is helpful in determining the level of shortness by comparing one heel to the other. In toddlers and infants, straightening the legs at the knee is almost always necessary.
The medial malleoli may be used instead of the calcanei if leg length is still unclear. The patient’s feet should extend just past the edge of the adjusting table with the patient supine if the child is over 1 year of age (Fig. 33-6).
Parents can help the doctor by assisting their child to remain still long enough for the doctor to ascertain the inequality in the leg length. This inequality is thought to be a function of the spinal thalamic tracts in the spinal cord beginning in the brainstem and the effects are extending down all the way to the bottom of the feet (1).
In a supine position, the presence of a lateral atlas may present with a short leg (1). Paraspinal hypertonicity may also be found present in the thoracic spine. Placing the patient in a supine position and palpating the erector spinae muscles, specifically the upper dorsal longissimus group, should be symmetrical in tone compared to the other side if no subluxation is present in the upper cervical spine. The doctor will also have to rule out a possible thoracic subluxation causing the hypertonicity as well. There is no “atlas challenge test” for laterality in the Atlas Orthogonal program. However, it is interesting to note that if there is an atlas misalignment in a child, the doctor will often notice an elevated (+Z) ipsilateral clavicle and +Y rib distortion contralateral to atlas laterality and an elevated pubic symphysis on one side. Once the right vector of atlas is delivered through an adjustment, these distortions are no longer visible.
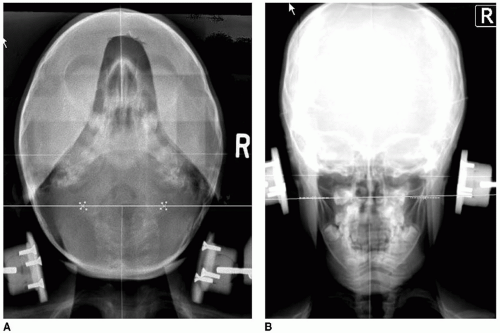
Radiographs in the AO Procedures
The x-rays of a child should be minimal and consist of a frontal view of the skull with the lower cervical spine visible, taken after the lateral cervical shows the atlas tilt. The tilt of the atlas on the lateral cervical x-ray gives a reference for directing the central ray through the facial structures at the precise level of the C1 vertebrae on the frontal x-ray. A horizontal view is also taken with the chin placed on the Bucky with the head in extension. In adults, an APOM and lower cervical spine A-P is also taken. Post x-rays are taken immediately after the first adjustment to verify correction has been made and to make any adjustments to the correction formula for the patient. X-ray line markings are similar to the NUCCA program, but the AO program uses primary ossification centers especially on the horizontal view; the inferior lateral masses facet is marked giving a more accurate measurement than the transverse foramen of C1 (Fig. 33-7A-C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree