Logan Basic Technique for Infants, Children, and Pregnant Women
D. Patrick Montgomery
Hugh B. Logan, DC, presented his new technique, called the “Universal Health-Basic Technique” in 1931 (1). Within a few years it was called simply the Logan Basic Technique (LBT). The term “Basic” is used because it deals with the base of the spine, the sacrum.
Logan liked the structural approach to chiropractic and reasoned that because the spine rested on the sacrum, if the sacrum was subluxated or unlevel, it would be deleterious to the stability of the spine and could allow for other subluxations within the spine to remain not corrected by localized adjustments to those subluxations. Sacral subluxations may indeed allow subluxation in the spine to occur more readily. Logan worked out a method of analyzing the normal spine and its biomechanics as well as the pathomechanics of pelvic and spinal distortions caused by sacral subluxations. Sacral subluxations would cause both bony misalignments in the spine and abnormal muscle function throughout the length of the spine. The neurological component of these effects would have profound ramifications in the functions of the body, which would be magnified in a pregnant woman’s body.
LBT is a light-force chiropractic procedure with a long history of clinical effectiveness for infants, children, and pregnant women.
Infants should be checked by a chiropractor soon after birth for any evidence of spinal or pelvic misalignments. For an infant and a child up to 5 years of age, checking for and correcting pelvic misalignments is easily accomplished by using one of the procedures in LBT. When examining an infant using the “indicators” for LBT, one indicator that is easily checked is the gluteal line deviation. Place the infant on his or her abdomen and squeeze the upper parts of the gluteal region together. If there is proper sacral alignment, the crease formed follows the line of the spine. However, if there is an anterior displacement of the sacrum on one side, the line deviates to that side (Fig. 31-1) (2).
When an infant is adjusted, a suggestion for positioning the child is to place the child on the parent’s supine chest or abdomen. Have the child face the parent for security and to dismiss any of the child’s fears.
If a Zenith or other hi-lo table is used, have the parent holding the infant stand with his or her back to the table, then cautiously lower the table, stabilizing the parent/child if necessary. If the infant is a newborn, then lay the child down on a clean pad and baby blanket or similar cloth towel. In either case, pull down or undo the diaper only on one side, leaving the other side attached. This protects the equipment, the parent, and the doctor from unexpected bowel or urinary voiding.
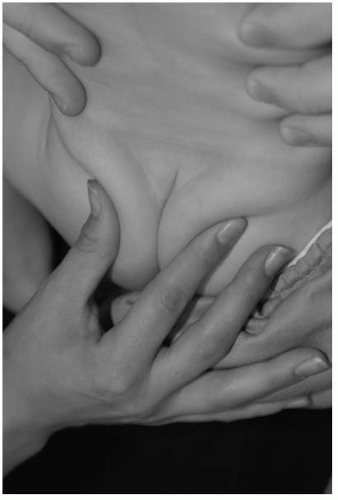
The pelvis should be raised by either the doctor’s non-adjusting hand or a rolled-up towel. This allows easy access to the LBT apex contact point on the infant’s pelvis (Fig. 31-2). The contact point is located where the sacrotuberous ligament attaches to the sacrum. In the infant, this point will feel like an inverted “V,” about the size of the space formed by the doctor’s thumb and index finger when pressed together. It is very important for the success of the contact that the doctor’s adjusting finger be placed anterior to this junction.
For doctors who have a large thumb, the end of the last phalanx for the little finger should be used for the contact. If the doctor has a small hand, the end of the thumb can be used, just as if the apex contact was applied to an adult. The finger should be flexed with the end of the finger or thumb pointing posteriorly (toward the ceiling) and with some laterality to the same side as the contact (Fig. 31-3).
This contact should be held from 15 seconds up to a minute. Check immediately after the contact for its effectiveness. Most of the time, the gluteal line will be
straight just after the application. If it has not changed or seems to be more marked, the apex contact was not given anterior to the sacrotuberous ligament. Rather, it was given either to the inferior side or the posterior side. In this case, the doctor should give the apex contact again. In the case of a very symptomatic infant, the contact should be given for up to 3 to 4 minutes.
straight just after the application. If it has not changed or seems to be more marked, the apex contact was not given anterior to the sacrotuberous ligament. Rather, it was given either to the inferior side or the posterior side. In this case, the doctor should give the apex contact again. In the case of a very symptomatic infant, the contact should be given for up to 3 to 4 minutes.
Sometimes during the first examination of an infant, when the gluteal line is checked, two lines are formed, one deviating to the right and one deviating to the left. This may indicate a bilateral anterior sacral subluxation (2). In this presentation, the apex contact is applied on one side first and then, during the same visit, the contact is applied to the other side.
At the end of the adjustment, re-checking the deviation is required to see the effectiveness and whether or not the child should be adjusted again. In Figure 31-4 the recheck shows partial correction of the sacral subluxation. This child will be scheduled for a follow-up check in a few days.
YOUNG CHILD
For a young child, one who is walking, more of the LBT indicators beyond just the gluteal line deviation may be positive. A posterior-inferior ilium with a prominent posterior superior iliac spine on the same side as the anteroinferior sacral subluxation may be palpated, there may be tight lumbar erector spinae muscles on the same side, and possible toeing-out of the leg on the same side may be detected.
With the patient’s face in the headpiece, the abdominal piece is raised to lift the pelvis for the application of the apex contact (Fig. 31-5). A rolled up, clean towel or sternal roll should be placed under the ankles to lessen the tension of the hamstring muscles (Fig. 31-6). The child is now in the proper position for the application of the LBT procedures.
The apex contact is administered to a young child in much the same manner as in the infant, with the distal end of the doctor’s fifth finger placed anterior to the junction of the sacrotuberous ligament and the sacrum. The doctor’s other hand then palpates up the spine to detect muscular imbalances and vertebral rotations (Fig. 31-7).
 FIGURE 31-7 The doctor’s non-adjusting hand palpates for muscular imbalances and vertebral rotation. |
The doctor is seated on the side opposite the contact. This allows for the proper line of correction (LOC) of the apex contact. The LOC should be directed posteriorly (toward the ceiling) and laterally. As the LOC is directed more lateral, the doctor will tend to detect the pull of the erector spinae muscles bilaterally more caudally. As the doctor detects symmetry of the lower erector spinae muscles, the LOC gradually is directed more cephalad. The effect of this may cause the erector spinae muscles to have more symmetrical tone higher up in the spine, which is detected by the doctor’s non-adjusting hand (Fig. 31-8). At this point, the doctor can easily palpate deeper to detect any rotational subluxations. If one or more is detected, the doctor then gently contacts the posterior transverse process, mamillary process, or articular pillar with light but steady anterior pressure while changing the LOC of the apex contact.
When the LOC of the apex contact reaches the proper angle to affect that level of the spine, the doctor will feel the subluxated vertebra shift to a more correct position.
When the LOC of the apex contact reaches the proper angle to affect that level of the spine, the doctor will feel the subluxated vertebra shift to a more correct position.
When the spinal musculature seems to be symmetrical in tone, the doctor then gives a gentle light thrust of the apex contact hand along the last LOC given. This theoretically “sets” the adjustment and the session is finished.
OLDER CHILD
Checking the pelvis and spine of an older child with LBT procedures requires much of the same examination that is performed in the adult.
The five cardinal signs (the acronym “HELPS”) are used during this examination (3):