FIGURE 43-1 Clinical photograph depicting a transverse fingertip amputation of the right ring finger.
Despite the sense of urgency that often accompanies the initial evaluation of patients with traumatic fingertip amputations or soft tissue loss, a thorough history and clinical examination should be performed. As with other traumatic conditions, hand dominance, functional demands, and any associated medical comorbidities must be documented. Careful assessment of wound contamination, vascular status, and the condition of proximal soft tissues (nerves, tendons, subcutaneous tissue, and skin) should be done. Furthermore, characterization is made for the pattern of tissue loss, which will help determine the most appropriate reconstructive technique (Figure 43-2). All amputated parts should be salvaged, saved, and examined for possible repair, replantation, or use as “spare parts.” Radiographic evaluation of the affected anatomic parts is necessary to assess for the presence and pattern of skeletal injury and/or articular involvement. With more proximal amputations, x-rays of both the injured finger and amputated part are helpful in reconstructive planning. Antibiotics and tetanus boosters should be provided in the emergency setting. The injured hand/upper limb is irrigated with sterile saline and bulky soft bandages, and splint immobilization is applied. The amputated part is wrapped in saline-soaked gauze and placed in a sterile container.
Surgical Indications
The goal of treatment for fingertip injuries is the reconstitution of a durable, sensate, viable digital tip that possesses adequate bony coverage and, if possible, preserves digital length. As a host of treatment options are available, the particular reconstructive strategy must be tailored to each individual patient. Surgical indications are therefore equally variable. In general, surgical treatment is indicated in cases of extensive fingertip soft tissue loss exceeding 1 cm2 in cross-sectional area and/or bone exposed. It should be noted that the vast majority of simple fingertip injuries may be treated effectively with nonoperative means, particularly in young children, who demonstrate great healing potential.
In cases of more extensive soft tissue loss, treatment is indicated for coverage of bony, tendinous, or neurovascular structures that cannot be achieved by simple primary closure alone.
SURGICAL PROCEDURES
Good sound habits are more important than rules—use concepts.
—Mike Krzyzewski
While a host of surgical procedures are within the armamentarium of the pediatric hand and upper extremity surgeon, a few fundamental principles are universally applicable. First, every effort should be made to avoid infection by thorough irrigation and debridement of contaminated wounds and timely soft tissue (and bony) reconstruction. Second, in a child, emphasis is placed on preserving digital length, function, and growth potential whenever practical. Finally, simpler solutions are favored over more complex solutions, particularly in the anxious, distressed, often nonverbal child in whom multiple procedures and/or anesthetics are to be avoided.
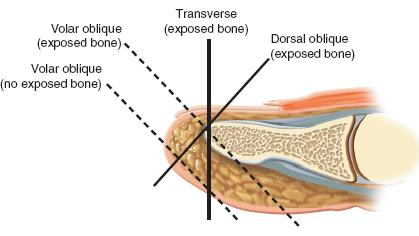
FIGURE 43-2 Schematic diagram depicting the patterns of digital tip loss: dorsal oblique, transverse, and volar oblique.
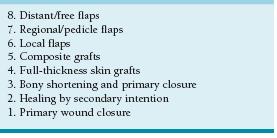
The “reconstructive ladder” has been proposed to guide the surgeon on treatment options2 (Table 43.1). Each successive “rung” of the reconstructive ladder represents a more complex surgical strategy to achieve soft tissue coverage and should only be considered if simpler, less complicated procedures are ruled out. Pediatric hand and upper extremity surgeons should be familiar with these surgical options, and a systematic approach to reconstructive decision making is recommended.
 Primary Wound Closure, Healing by Secondary Intention, Bony Shortening and Primary Closure or Healing by Secondary Intention
Primary Wound Closure, Healing by Secondary Intention, Bony Shortening and Primary Closure or Healing by Secondary Intention
Simple solutions are possible in the vast majority of pediatric fingertip injuries. When there is adequate skin and soft tissue available, primary wound closure is easy, effective, and almost universally successful. In cases with uncovered distal phalangeal bone, simple skeletal shortening by rongeuring the exposed tip of the distal phalanx will allow for primary wound closure or adequate healing by secondary intention.
In these cases, small defects (<1 cm2 in cross-sectional area) may be treated with serial dressing changes, allowing the wound to heal by secondary intention.3–6 When wound healing by secondary intention is pursued, the primary dressing may be left in place for 1 to 2 weeks in cases of clean uncontaminated wounds. At this time, once there is confirmation that there is no infection, parents and families may be instructed on daily half-strength hydrogen peroxide soaks and dressing changes. Our preference is to use petrolatum gauze (Xeroform, Covidien, Mansfield, MA) and Coban self-adherent wrap (3M, St. Paul, MN) to the affected digit. While the long-term results are highly satisfactory in terms of both sensibility and aesthetic appearance, this strategy takes time and may be challenging in the very young patient. Parents and other care providers must be dedicated and sophisticated in their understanding and adherence to this treatment plan.
 Split-Thickness Skin Grafts, Full-Thickness Skin Grafts, and Composite Grafts
Split-Thickness Skin Grafts, Full-Thickness Skin Grafts, and Composite Grafts
Skin grafting for fingertip injuries is rare in children. A prerequisite to skin grafting is an uncontaminated recipient soft tissue bed; adequate vascularity to support graft healing; and no exposed bone, tendon, or neurovascular bundles.
Split-thickness skin grafting (STSG) is rarely used in the hand except for large palmar areas of skin loss, such as with deep burns. The STSG is used in delayed closure of large traumatic forearm wounds, such as post fasciotomies for compartment syndromes, when there is an underlying bed of healthy muscle. The graft donor site is usually the upper posterior thigh to lessen the poor aesthetics of the resultant scar. An appropriate-size dermatome to match the recipient site is utilized. Usually this is 0.015″. Mineral oil is placed on the donor site, and tension is maintained on the dermatome throughout the harvest to obtain a uniform thickness graft. The STSG is meshed with standard equipment and then placed with mild tension over the recipient site. The STSG is sutured in place, so there is adherence of the graft over the entire recipient site. A petrolatum gauze (Xeroform, Covidien, Mansfield, MA) and moist cotton bolster are secured over the graft to promote healing. This is removed in the office at 5 to 14 days, depending on the clinical scenario.
Full-thickness skin grafting (FTSG) may similarly be utilized in cases of large (>1 to 2 cm) skin loss with adequate vascularized subcutaneous tissue. Skin grafts are not indicated in cases of exposed bone, tendon, or cartilage, and they may lack the bulk and durability desired for hand function; for this reason, it is unusual for skin grafts to be used in cases of fingertip avulsions or digital tissue loss. Potential donor sites for FTSG include the inguinal fold (lateral to the palpable femoral pulse to avoid harvest of future hair-bearing skin), antecubital flexion crease, wrist flexion crease (though this is not preferred given the potentially aesthetically and socially unpleasing transverse scar), and hypothenar eminence of the hand.7 Ideally, glabrous skin of equal pigmentation is chosen to achieve a more durable and aesthetically pleasing result. After harvest and defatting, the skin graft may be sewn in using multiple interrupted 5-0 or 6-0 polyglactin suture (Chromic, Ethicon, Inc., Somerville, NJ), the tails of which are left long to secure a saline-soaked cotton and petrolatum gauze (Xeroform, Covidien, Mansfield, MA) bolster, which is placed over the graft to promote adherence and subsequent graft take. Dressings and the petrolatum gauze-cotton bolster may be removed after 2 weeks, and near-universal take is expected in young, healthy children with clean, vascularized soft tissue beds.
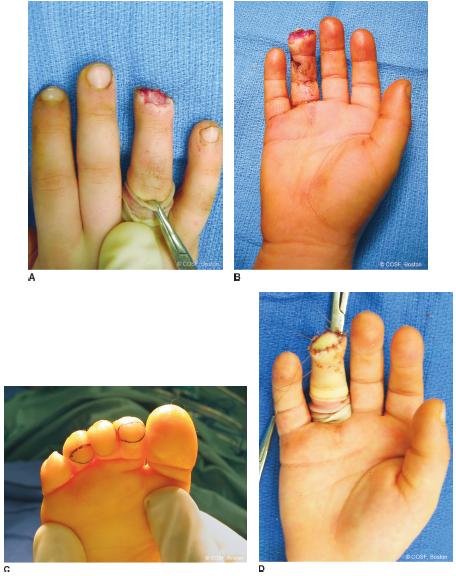

FIGURE 43-3 Clinical photographs depicting the technique of composite toe grafting for digital tip amputations. A, B: Intraoperative photographs depicting the dorsal and volar aspects of the injured ring finger. C: Intraoperative photograph depicting the incisions used to harvest free composite toe pulp graft. The elliptical design facilitates primary wound closure of the harvest site while allowing appropriate recipient site coverage. D: Intraoperative appearance after graft placement. E: The donor site is closed primarily. F, G: Appearance of the fingertip 2 months postoperatively. The pulp has been reconstituted with complete take of the composite graft. H: The appearance of the donor site postoperatively.
Another strategy that is particularly helpful for fingertip reconstruction in children is the use of composite grafts . If the amputated digital tip is available, it may be repaired primarily; in children, there is a higher likelihood of healing than in adults.8,9 In cases where the digital tip is not available, contaminated, or too damaged to allow for “repositioning,” composite toe grafting may be performed10,11 (Figure 43-3). Under general anesthesia and digital tourniquet control, an elliptical-shaped incision is made over the plantar pulp of one of the lesser toes, the dimensions of which are determined by the size of the fingertip defect. Skin and approximately 4 mm of subcutaneous fat are excised as a composite graft. Provided that the major axis of the ellipse is two to three times greater than the minor axis, the donor defect may be easily closed primarily with multiple interrupted 4-0 or 5-0 polyglactin suture (Chromic, Ethicon, Inc., Somerville, NJ), followed by application of a simple bandage. The composite graft is then placed in the recipient bed and reapproximated using multiple interrupted 5-0 polyglactin suture (Chromic, Ethicon, Inc., Somerville, NJ), the tails of which are left long to secure a saline-soaked cotton and petrolatum gauze (Xeroform, Covidien, Mansfield, MA) bolster secured over the graft site. Sterile bandages are applied, followed by cast immobilization in the very young to ensure compliance with postoperative care.

FIGURE 43-4 Schematic diagram of the volar V-Y local advancement flap.
 Local Advancement Flaps (V-Y, Moberg, Thenar)
Local Advancement Flaps (V-Y, Moberg, Thenar)
Local flaps involve the use of adjacent vascularized skin and soft tissue to provide soft tissue coverage.12 These flaps are used when the area involved is larger than healing by secondary intention will tolerate, and more substantial distal soft tissue coverage of the fingertip is required for durability and function long term. In most situations, the blood supply to this tissue is provided by the subdermal or subcutaneous microcirculation, so-called random pattern flaps. In other situations, the arterial inflow and venous outflow of the local flap are supplied by a single, identifiable vascular pedicle, the “axial” flap.
A number of random pattern local flaps are available for fingertip injuries. In general, these local flaps are preferred given their location, tissue match, and simplicity. This is particularly true in cases of preserved but exposed distal phalanx. Knowledge of the pattern of fingertip tissue loss in part guides decision making regarding the choice of flap to be used.
Transverse and dorsal oblique fingertip amputations may be successfully treated with V-Y advancement flaps.13 While in theory up to 10 mm of “length” may be obtained, in reality these flaps are of greatest utility when greater than half the volar tissue measured from the digital tip to the distal interphalangeal (DIP) joint flexion crease is available for advancement. Under local or general anesthesia and digital tourniquet control, an apex-proximal V-shaped incision is created through the dermis only; the apex is placed at the level of the DIP flexion crease, and the distal extensions are made obliquely to the midaxial line (Figure 43-4). Following skin incision, blunt dissection is performed in the subcutaneous tissues via longitudinal spreading of tenotomy or Iris scissors, breaking up the fibrous septae of the digital pulp while preserving the subcutaneous tissue connections—and thus vascularity—to the overlying skin. After flap mobilization, the leading distal edge of the volar skin is advanced and sewn primarily into the dorsal skin and nail bed using interrupted 5-0 polyglactin suture (Chromic, Ethicon, Inc., Somerville, NJ). It is critical that the distal suture line not be made with undue tension, so as to avoid volar curvature of the nail bed and subsequent “hook nail” deformity. The two oblique limbs are similarly closed with interrupted 5-0 polyglactin suture (Chromic, Ethicon, Inc., Somerville, NJ), further alleviating any tension on the distal suture line. Given the distal tissue advancement, the most proximal aspect of the wound will be closed primarily, forming the stem of the resultant Y-shaped wound. The tourniquet is released to ensure digital tip and flap viability, and a sterile bandage is applied. The digit is splint or cast immobilized, particularly in the very young, active, noncompliant patient.
Fingertip reconstruction may be similarly achieved using radial and ulnar V-Y advancement flaps, first described and popularized by Kutler.14 This technique is most effective in cases of transverse or volar oblique fingertip avulsions.
The Moberg volar advancement flap is also a useful tool for soft tissue avulsions of the thumb tip15,16 (Figure 43-5). This technique of distal tip coverage is applicable to the thumb but not other digits, owing to the dorsal blood supply to the thumb tip, which is undisturbed during volar flap elevation and mobilization. Its advantages include preservation of thumb length and reconstruction with durable, thick, vascular and sensate tissue. Again, under general anesthesia and tourniquet control, midaxial incisions are created from the soft tissue defect at the thumb tip and extended proximally. Sharp dissection is performed down to the level of the flexor tendon sheath, and the volar skin, subcutaneous tissue, and both radial and ulnar neurovascular bundles are elevated from distal to proximal as a tongue of soft tissue. Care is taken to preserve the flexor tendon sheath during this dissection. After adequate soft tissue elevation, the volar flap is advanced distally and reapproximated using simple interrupted polyglactin sutures. Up to 1 cm of distal coverage may be achieved. The tourniquet is released and vascularity to the thumb and flap ascertained. Dressings are applied, as well as cast or splint immobilization as necessary.
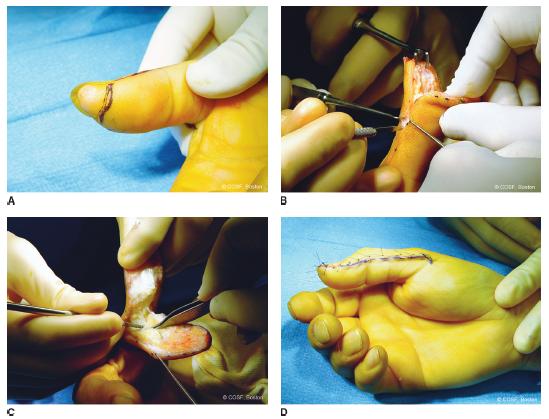
FIGURE 43-5 The Moberg volar advancement flap for the thumb. A: Preoperative photograph of a thumb previously treated with skin graft alone for soft tissue avulsion. The patient complained of pain and hypersensitivity at the thumb tip. There is a paucity of soft tissue bulk over the distal phalangeal tip. B: Midaxial incisions are created, and the volar skin flap is raised from distal to proximal, just superficial to the flexor tendon sheath. C: The flap is generously elevated, taking the neurovascular bundles with the volar tissue. D: After advancement and skin closure, there is reconstitution of a durable, bulky soft tissue pad over the distal phalanx, achieved without undue flexion of the interphalangeal joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree