Fig. 19.1
Abdominal skin marking for instrument placement
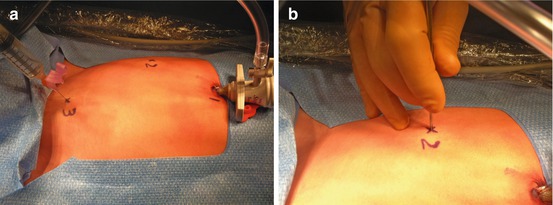
Fig. 19.2
(a, b) Local anesthetic and stab incisions made under direct visualization after placement of umbilical trocar

Fig. 19.3
Maryland dissector and bipolar device passed directly through stab incisions
Once all instruments are inserted satisfactorily, the left spermatic vessels are identified, and a site for incision of the posterior peritoneum above the spermatic vessels is identified as far cephalad from the internal ring as possible to avoid injury to the vas deferens and collateral blood supply from the deferential vessels (Fig. 19.4). Trendelenburg positioning is often helpful during this step. Occasionally there are adhesions, especially of the sigmoid in this area. They can usually be lysed with the Maryland and bipolar device, and rarely will another working port or other instrumentation be required. Still the surgeon should be prepared for any eventuality, especially in a patient with prior abdominal, pelvic, or inguinal surgery.
Fig. 19.4
Anatomy of relevant structures
The left-handed Maryland dissector is used to grasp the posterior peritoneum overlying the spermatic vessels, and the right-handed bipolar device pierces through the peritoneum, creating a window through which the vessels can be dissected free and isolated (Fig. 19.5). Once this maneuver has been accomplished, the vessels are grasped completely with the Maryland, and the bipolar is used to create a window behind the vessels, and the window is extending cephalad and caudad bluntly until an adequate area is visible for ligation. No attempt is made to separate the artery from the veins or to identify lymphatics as noted above (Fig. 19.6).
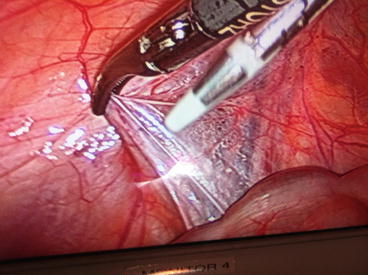
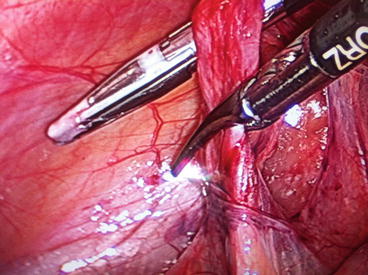
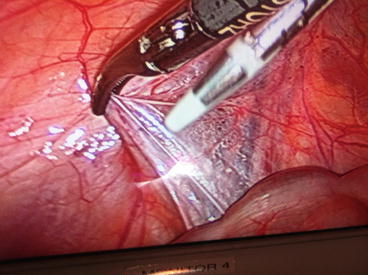
Fig. 19.5
Creation of peritoneal window
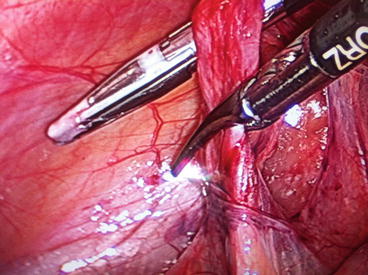
Fig. 19.6
Isolation of the spermatic cord using the bipolar device as dissector while grasping the cord with the Maryland dissector
The bipolar device is applied to the entire vascular package 2–3 times to completely seal all vessels (Fig. 19.7). Intermittent traction on the ipsilateral testis can be applied to identify any additional vessels missed initially. The vessels are not routinely divided. Final inspection confirms no additional venous collaterals are present, hemostasis is achieved, the vas deferens and deferential vessels are undisturbed, and no overt complications have occurred (Fig. 19.8).
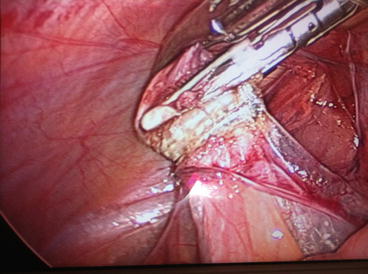
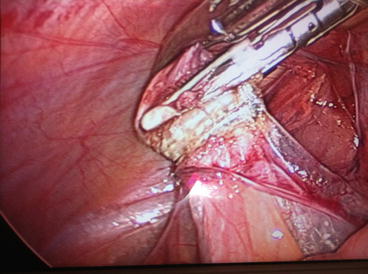
Fig. 19.7
Bipolar sealing performed 2–3 times without dividing the vascular package
Fig. 19.8
Final inspection, ensuring no complications have occurred, and the varicocele is completely ligated
The abdomen is desufflated, and all instruments and the trocar are removed. A single 3-0 or 4-0 absorbable suture is used to close the umbilical fascia in a figure of eight fashion, to prevent herniation. No suture closure of the stab incisions is necessary. Additional local anesthetic is infiltrated, and the skin at the incision sites are all reapproximated with skin glue. Ketorolac 0.5 mg/kg IV is administered in the operating room, and the patient is discharged the same day with minimal oral analgesic requirements (NSAIDs and acetaminophen). We do not routinely prescribe narcotics postoperatively. Patients are allowed to resume full activities and bathe normally immediately. The average surgical time from skin to skin is 15–20 min.
Additional Comments
A patent processus vaginalis might be encountered on either side during laparoscopic exploration. Repair is not indicated unless it is thought to be “clinically significant,” but this is beyond the scope of this chapter.
This technique is safe and effective in cases where there has been previous ipsilateral inguinal surgery performed [11]. More extensive dissection of the left colon made be required, as well as adhesiolysis to find a safe window for the dissection. Additional ports may need to be placed in these cases to allow for exchange of instrumentation.
Outcomes and Complications
Intraoperative issues are rare, and all children are discharged the same day. In follow-up, no studies which measured testes pre- and postoperatively via orchidometer or ultrasound showed any evidence of loss of testicular size. Atassi et al. showed that the average relative left testicular volume increased by 20 % in the Palomo group, and this was not different from the group that underwent an artery-sparing procedure [12]. This is consistent with earlier work published by Kass et al. [13]. The majority of patients in the published literature demonstrated catch-up growth of the left testicle following laparoscopic varicocelectomy [14, 15]. Poon et al. compared catch-up growth between those who underwent a lymphatic sparing procedure to those who had a non-lymphatic-sparing operation and found that most demonstrated catch-up growth, regardless of the choice of procedure [16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


