Ureteral HD grade
Endoscopic findings
H0
No orifice distension evident
H1
Orifice opens, intramural tunnel not evident
H2
Intramural tunnel evident, extramural tunnel not evident
H3
Extramural tunnel evident or ureter can accept the cystoscope
Fig. 22.1
Injection volume based on HD grade. The injected volume increases significantly with each increase in HD grade from H1 to H3. The bold line represents the average injected volume. Dashed lines represent the 95 % confidence intervals for the mean
When employing the double HIT methodology, the needle is placed into the ureteral orifice and inserted in the mid-ureteral tunnel at the 6 o’clock position after performing ureteral hydrodistention. This differs from the STING technique, where the needle is inserted 2–3 mm below the refluxing orifice. Bulking agent is injected until a sufficient bulge is produced, which coapts the detrusor tunnel. A second injection at the distal most aspect of the intraureteral tunnel results in coaptation of the orifice (Fig. 22.2). Hydrodistention with the bladder nearly empty is performed following each injection to monitor progress. Additional injection(s) may be needed to achieve an H0 ureter during hydrodistention.
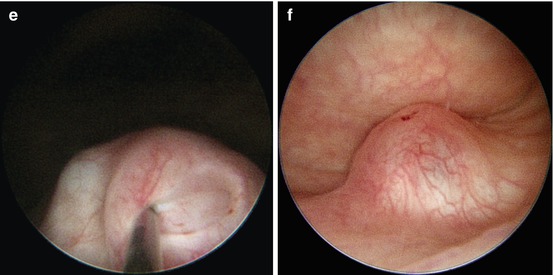
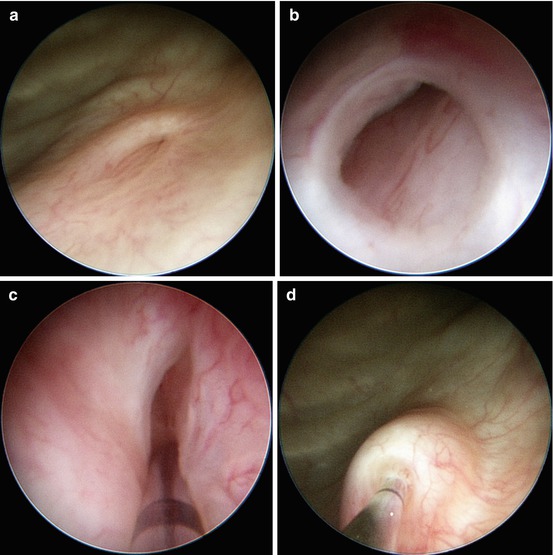
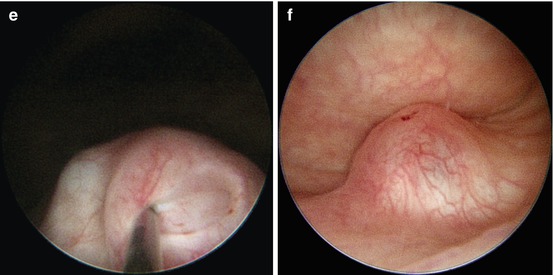
Fig. 22.2
Double HIT method. The bladder is emptied and the ureteral orifice visualized (a), followed by hydrodistention (b). The proximal HIT is performed with the needle inserted into the mid-ureteral tunnel at the 6 o’clock position (c), and sufficient bulking agent is injected to produce a bulge which coapts the detrusor tunnel (d). The distal HIT (e) leads to coaptation of the ureteral orifice (f). The double HIT coapts both the detrusor tunnel and the ureteral orifice and results in non-distensibility of the ureteral orifice (H0)
Clinical and Radiographic Outcomes Following Endoscopic Injection
The clinical success of any type of anti-reflux surgery can be measured radiographically (absence or downgrading of VUR) and clinically (absence or decrease in frequency of febrile urinary tract infections). In the medical literature, there is considerable variability as to how success is measured; therefore, true surgical outcomes are difficult to ascertain [13]. The average resolution of VUR following a single endoscopic injection is 83 % based on aggregate data, though success rates have ranged from 70 to 95 % [11]. In our long-term experience with the double HIT method, both radiographic and clinical successes at 1-year follow-up were 93 % [14]. Importantly, 95 % of patients avoided open surgery during a 4-year follow-up [13].
Preventative Measures to Avoid Complications
Families should be thoroughly counseled regarding the various VUR management options, and all children should undergo screening for and treatment of bowel/bladder dysfunction. In addition to proper patient selection, there are a number of technical principles that can help to ensure a successful outcome. Proper injection technique, selection of correct injection site(s), adequate injected volume, and recognizing the endpoints of the injection are all important components of the injection procedure necessary to follow in order to avert failure. Volume of injection varies depending on the injection method(s). As stated above, the HD grade of the ureter should directly correlate with the volume used when the double HIT method is employed. It is important to note that although higher grades of VUR are associated with higher HD grades, even lower grades of VUR may have high HD grades and require increased volumes of injection [12]. After injection, the bladder should be emptied and hydrodistention repeated to confirm the absence of ureteral distensibility (i.e., H0 ureter).
Complications
Complications can be categorized into those that occur in the immediate postoperative period and those that manifest as long as several years from the time of surgical intervention. Early complications typically occur within the first 48 h following injection and are often transient. Less than 4 % of children undergoing endoscopic VUR therapy complain of flank pain or nausea postoperatively and nearly all resolve with analgesics. Ureteral obstruction following endoscopic injection occurs in approximately 0.6 % of patients and is frequently associated with voiding dysfunction, secondary VUR, or with larger ureters when a large volume of bulking agent is injected [4, 11]. If anuria or oliguria persists beyond 24 h, a renal bladder ultrasound and serum creatinine level should be obtained to exclude obstruction. Complete obstruction requires placement of either ureteral stents or nephrostomy tubes to allow upper tract drainage. The latter might be preferable because the obstruction may be transient, and resolution can be anticipated when the hyaluronic acid component dissipates within 2 weeks of the injection. Hematuria and bladder spasms are frequent complications of ureteral reimplantation, but these complications are rare following endoscopic treatment.
It is not uncommon for patients to develop a febrile urinary tract infection after endoscopic injection. Checking the urine preoperatively and beginning appropriate antibiotics if indicated can usually avoid this. In patients with a symptomatic UTI, surgery should be postponed.
Postoperative reflux may be the result of uncorrected, ipsilateral, or new onset contralateral reflux. Although persistent reflux may be the result of the aforementioned reasons for failure of the procedure, it often is the result of overt bladder pathology (neurogenic bladder or anatomical anomalies) or failure to recognize underlying bladder dysfunction. Voiding dysfunction or dysfunctional elimination accounts for treatment failures after open or endoscopic correction of VUR. These patients typically have urinary tract infections, incontinence, urgency, frequency, and constipation. Aggressive bathroom management, including strict adherence to voiding and bowel regimens, will often result in resolution of reflux as well as associated lower urinary tract infections. The 2010 AUA Reflux Guidelines recommend management of any suspected bladder/bowel dysfunction, preferably prior to any surgical intervention for VUR [2]. Patients with a previous history of voiding dysfunction must be encouraged to continue their bathroom program preoperatively.
Treatment failure following endoscopic therapy ranges from 7 to 50 % and is dependent upon the technique, VUR grade, and surgeon experience [15]. Success rates for the HIT and double HIT technique approach those following ureteral reimplantation [14] and are currently the most common procedures performed in the USA (Salix Pharmaceuticals, unpublished data).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


