Laparoscopic Surgery
Joseph S. Sanfilippo
Lisa M. Roberts
Endoscopic (minimally invasive) surgery originated in 1847; the pioneering work of Sir James Y. Simpson of Edinburgh, Scotland, introduced chloroform narcosis. The first endoscopic evaluation of the abdominal cavity utilized a dog model in 1901 and was undertaken by Kelling. In 1911, Jacobaeus reported the first laparoscopic procedure in the human. Cold illumination fiber optics by Semm followed in 1963 and then the surgical area evolved rapidly. The first laparoscopic appendectomy was performed in 1980 and the first cholecystectomy in 1985.
This relatively new aspect of endoscopic surgery has far-reaching and ever-increasing innovative aspects. Advances in hysteroscopic surgery have altered the approach to uterine leiomyomas. Currently, the spectrum of laparoscopy includes radical hysterectomies and node sampling. The technical advances, including new instrumentation, are within the scope of this chapter. There appears to be a continuous state of evolution and more far-reaching new and improved instrumentation within the discipline of minimally invasive surgery.
Laparoscopy
Patient Positioning
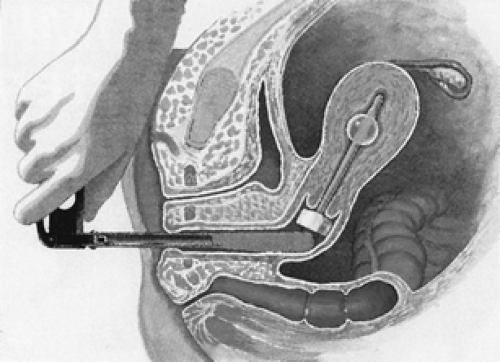
Proper patient positioning is paramount to avoid injuries. The surgeon should position the patient so as to prevent any excessive pressure on the lower extremities. Use of intermittent pneumatic compression devices is becoming more commonplace in order to prevent thromboembolic events. Surgeons must also be aware of nerve injuries that can result from improper placement of the lower extremities in stirrups. The lithotomy position with access to steep Trendelenburg is oftentimes utilized. The physician should discuss with the anesthesia team decisions regarding whether the arms should be extended or “tucked” along the sides of the patient. The latter requires particular attention to prevent any trauma to the hands and fingers when the table is maneuvered. Plastic “sleds” can be utilized to secure the upper extremities in obese patients.
With the patient in the low lithotomy position and the legs supported in stirrups, the buttocks should protrude slightly from the lower edge of the table. The lateral aspect of the knee should be protected with padding in the stirrup to prevent peroneal nerve injury. The knees should be kept in slight flexion to minimize stretching of the sciatic nerves and to provide increased stability in the Trendelenburg position. With respect to positioning of the arms, care should be taken not to stretch or traumatize the brachial plexus.
It has been advocated that an angle of 145 degrees between the abdomen and the lower extremity (thigh) is ideal, providing the surgeon with adequate space for instrumentation. The typical patient positioning for endoscopic surgery is noted in Figure 46.1.
Equipment
The array of instruments designed to facilitate operative laparoscopic procedures continues to evolve. This section describes a number of instruments.
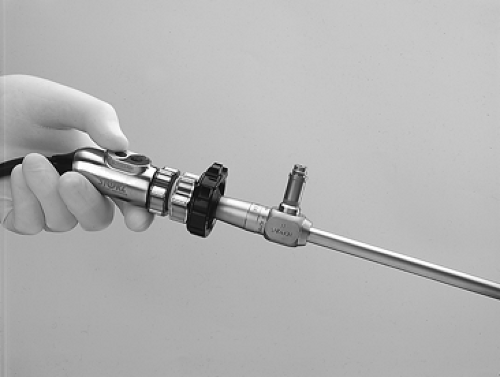
Viewing System
The video equipment should include a three-chip camera, a processor, a 300-watt xenon light source with fiber-optic cable, a high-resolution monitor, and a video recorder. The three-chip camera provides a sharper, brighter image with higher resolution than the older single-chip cameras (Fig. 46.2). Three-chip cameras can deliver over 600 lines of resolution; therefore, the video monitor’s horizontal resolution should be greater to maximize image quality. Fiber light cables should be inspected for broken fibers and replaced if a significant number of fibers are broken, because damaged fibers will result in suboptimal light delivery.
Operating Table
An operating room table that allows 30 degrees of flexion (Trendelenburg position) is ideal for visualization of the deep pelvis. Shoulder braces (Stierlen-Maquet Shoulder Braces, Siemens Medical Systems, Englewood, CO) placed at the acromioclavicular joints and the arms placed at the patient’s sides will minimize nerve injuries.
Insufflator
For most procedures, the pneumoperitoneum may be maintained with an insufflator that flows at a rate of 2 to 7 L per minute. High-flow insufflators that achieve up to 30 L per minute are available and will maintain the pneumoperitoneum during procedures with frequent changes in instruments that allow escape of large amounts of carbon dioxide (CO2), such as during tissue morcellation.
 Figure 46.2 Autoclavable Goldtip videolaparoscope with camera processor and xenon light source (Olympus, Melville, NY). |
Carbon Dioxide Warmer
There is evidence that warmed CO2 is less irritating to the peritoneal surface and, therefore, may cause fewer postoperative adhesions. CO2 warmers are available commercially.
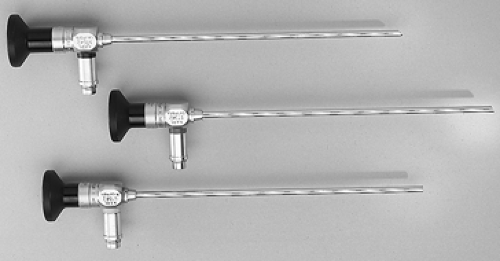
Laparoscopes
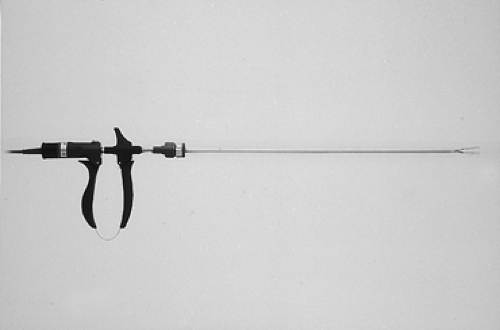
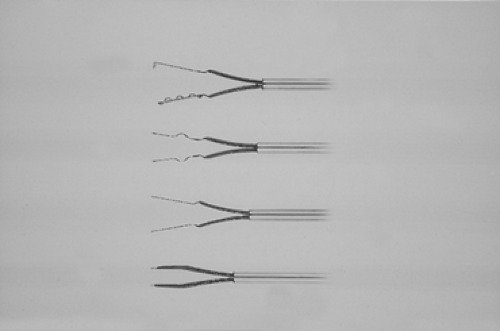
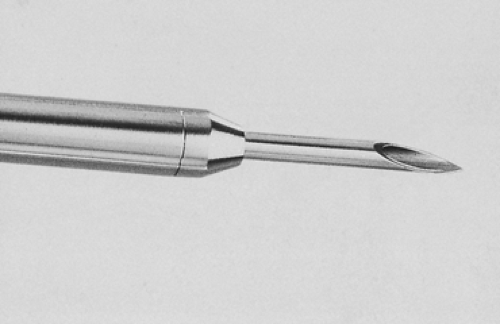
Laparoscopes are telescopes that vary in size from 2 to 10 mm. Viewing angles are available in 0-, 30-, 45-, and 70-degree increments. The choice is operator dependent. Most diagnostic laparoscopes do not contain an operating channel. Operative laparoscopes, with a smaller fiber diameter, contain a channel through which instruments or a laser (Figs. 46.3, 46.4) can be used.
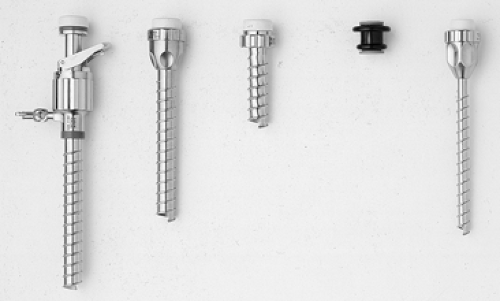
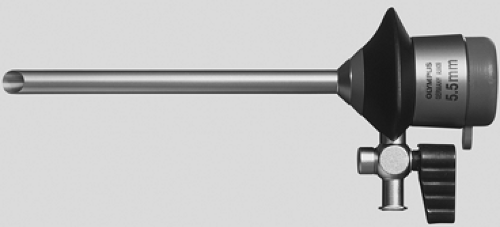
Trocars
Trocars come in a variety of sizes, materials, and designs. Sizes range from 3 to 15 mm. Reusable metal trocars have the advantage of cost efficiency, but they may actually be
more dangerous if the tips are not kept sharp (Figs. 46.5,46.6,46.7). Disposable trocars are utilized in most operating rooms; they decrease the risk of injury during insertion compared with reusuable instrumentation that may require increased force during insertion (Fig. 46.8). Some trocars are designed to stretch the fascia so that fascial closure is not necessary. Others have been designed to allow visualization of tissue layer separation with the laparoscope during insertion. Advocates assert that this type of trocar decreases bowel and vascular injuries. There are no objective data supportive of a reduction in risk for any trocar. The trocar chosen should be based on the surgeon’s preference. Hasson-type trocars have a blunt end for placement in open laparoscopy (Figs. 46.9, 46.10).
more dangerous if the tips are not kept sharp (Figs. 46.5,46.6,46.7). Disposable trocars are utilized in most operating rooms; they decrease the risk of injury during insertion compared with reusuable instrumentation that may require increased force during insertion (Fig. 46.8). Some trocars are designed to stretch the fascia so that fascial closure is not necessary. Others have been designed to allow visualization of tissue layer separation with the laparoscope during insertion. Advocates assert that this type of trocar decreases bowel and vascular injuries. There are no objective data supportive of a reduction in risk for any trocar. The trocar chosen should be based on the surgeon’s preference. Hasson-type trocars have a blunt end for placement in open laparoscopy (Figs. 46.9, 46.10).
Operating Instruments
A standard laparoscopy set should include the following:
Trocars
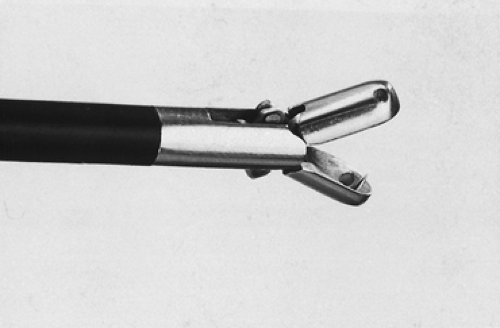
Bipolar forceps (Figs. 46.11, 46.12)
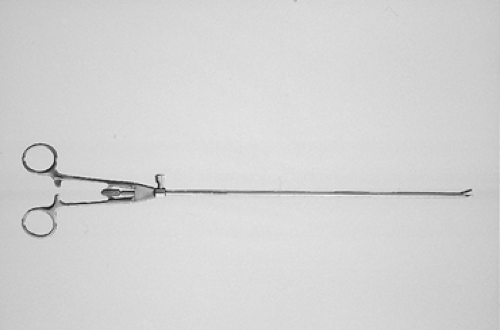
Biopsy forceps (Fig. 46.16)
Blunt probe
Blunt sawtooth scissors (Fig. 46.17)
Pointed Metzenbaum scissors (Fig. 46.18)
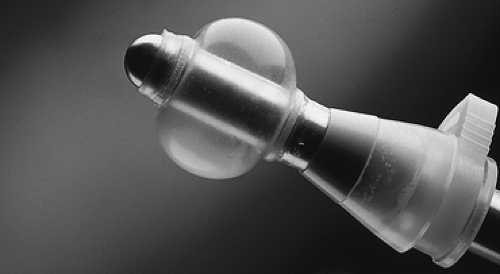
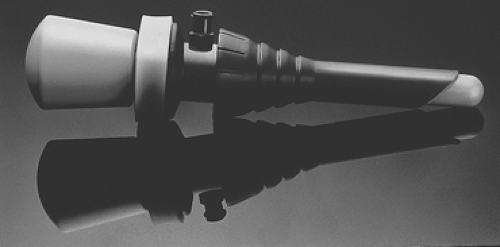
Figure 46.9 Ten-millimeter blunt trocar for open laparoscopy (Marlow Surgical Technologies Inc., Willoughby, OH).
Cyst aspiration needle (Fig. 46.19)
Suction and irrigator
Uterine manipulator (Figs. 46.20, 46.21)
An advanced laparoscopy set may include the following:
Knot pusher (Fig. 46.25)
Vaginal delineator (Fig. 46.26)
Babcock atraumatic grasper (Fig. 46.27)
Allis clamp
Adson forceps (Fig. 46.28)
Corkscrew
Single-tooth tenaculum
Atraumatic bowel grasper
Monopolar spatula (Fig. 46.29)
Endoscopic specimen retrieval bags (Figs. 46.30, 46.31)
Endoscopic suture ligatures (Fig. 46.32)
Microbipolar forceps
Morcellator
Rectal probe
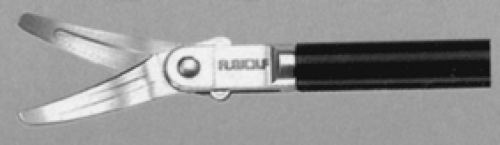
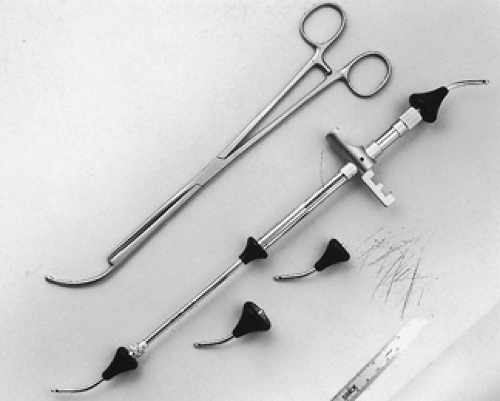 Figure 46.21 Hulka uterine manipulator tenaculum (Richard Wolf Medical Instruments, Vernon Hills, IL) and Cohen Uterine Cannula (Karl Storz Endoscopy–America, Culver City, CA). |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree