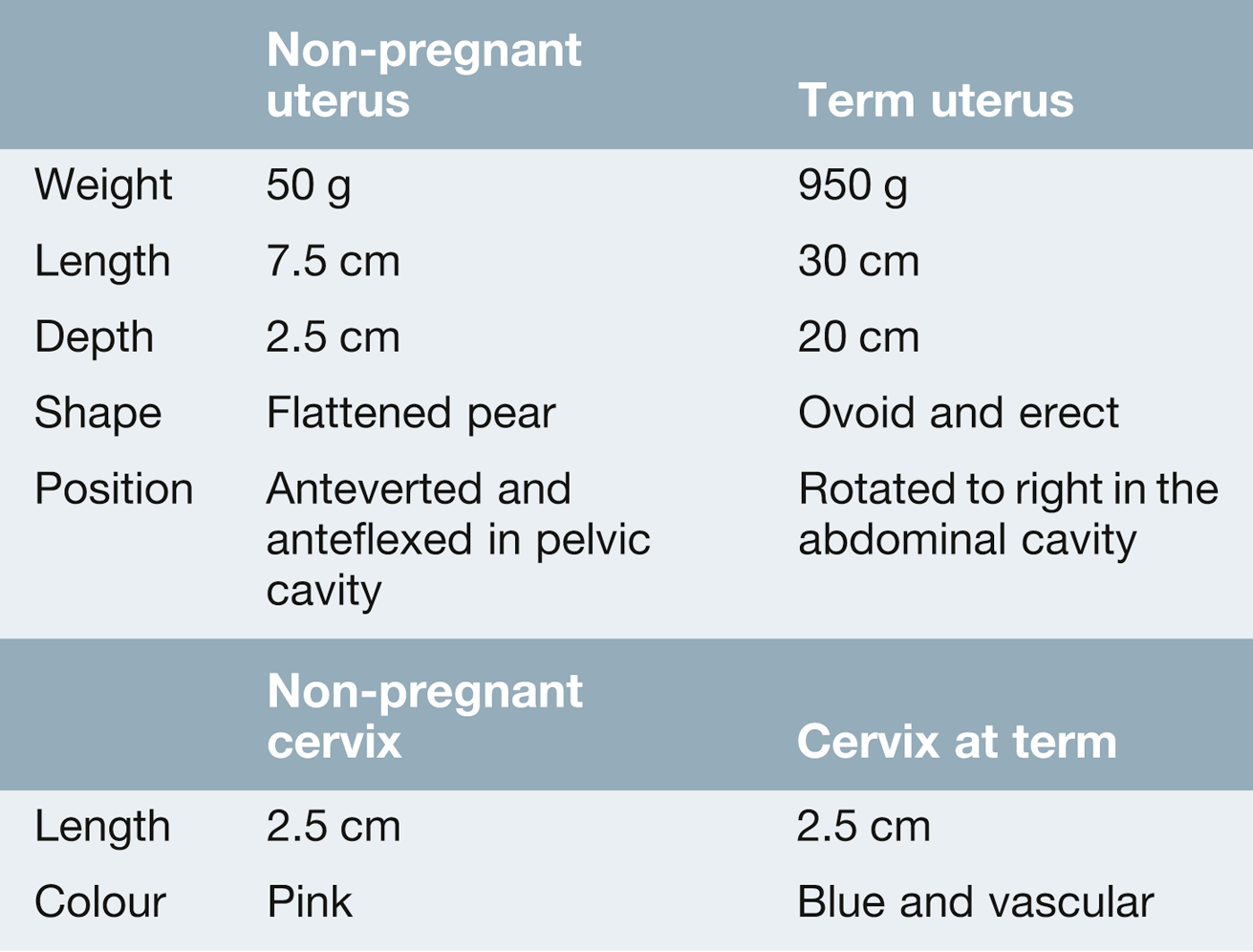
40 Labour is defined as the onset of regular uterine activity associated with effacement and dilatation of the cervix and descent of the presenting part through the cervix. The control and timing of delivery is crucial in the survival of any species and, in most, the interval between conception and parturition varies little. This is not the case in human pregnancy, where delivery can occur many weeks before or after the expected date. Labour in humans is surprisingly hazardous. Evolution ought to have favoured those mothers who deliver without problems, and yet, for those without access to good medical care, the lifetime risk of dying from labour and postnatal complications may be ≥ 10%. Apes are able to give birth with little problem. Their pelvises are relatively large, the fetal head is relatively small and the fetus is born facing anteriorly. When the Australopithecines adopted an upright posture around 4 million years ago, the pelvic shape became narrower in the anteroposterior plane to allow more efficient weight transfer from the trunk to the femurs. As the fetal head was still relatively small, the Australopithecines were also able to deliver without much problem, although the head was this time in the transverse position. With further evolution 1.5 million years ago, to Homo erectus and then Homo sapiens, the volume of the brain increased from around 500 mL to 1000–2000 mL. This increased the chance of the head being bigger than the pelvis (cephalopelvic disproportion) and to deliver successfully, it became necessary for the head to rotate during delivery. The head entered the pelvic brim in the transverse position, as the inlet is widest in the transverse plane, but rotated at the pelvic floor to the anteroposterior plane, which is the widest diameter of the pelvic outlet. This process requires efficient uterine activity and is aided by ‘moulding’ of the fetal head. Moulding is possible because the individual skull bones are unfused and can therefore move or even override each other to form the most efficient shape for delivery. The pelvic ligaments, particularly the cartilaginous joint of the symphysis pubis, relax antenatally under the influence of a hormone called relaxin, to maximize the pelvic diameters. Successful delivery also requires the fetus to enter the pelvis in the appropriate position. When these criteria are not met, problems may occur and these are discussed further in Chapter 45. The difficulty with human delivery, then, is related to the balance between our need to run (and therefore have a narrow pelvis) and our need to think (and therefore have a big head). There is a considerable difference between the labour of a primigravida (a mother having her first labour) and that of a parous woman who has had a previous vaginal delivery (Table 40.1). A successful vaginal delivery first time around usually leads to subsequent deliveries being relatively uneventful. Conversely, a caesarean section in a first labour can lead to subsequent obstetric problems. Table 40.1 The difference between a normal primigravid and multigravid labour The uterus is a thick-walled hollow organ, normally located entirely, in the non-pregnant state, within the lesser pelvis (Table 40.2). The smooth muscle fibres interdigitate to form a single functional muscle which increases markedly during pregnancy, mainly by hypertrophy (an increase in size of cells) and to a lesser extent, by hyperplasia (an increase in the number of smooth muscle cells). From early pregnancy onwards, the uterus contracts intermittently, and the frequency and amplitude of these contractions increase as labour approaches. These ‘Braxton Hicks’ contractions are irregular, low frequency and high amplitude in character and are only occasionally painful. They normally begin at a ‘pacemaker point’ close to the junction of the uterus and the fallopian tube and spread from this point downwards. Intensity is maximal at the fundus (where the muscle is thickest), intermediate at the mid-zone and least at the lower segment. The mechanisms controlling the onset of labour are different for different mammals. In some mammals, it is the changing levels of oestrogen and progesterone which regulate the timing of onset. In other animals, for example sheep, there is some evidence that the fetal adrenal secretion of corticosteroids is the responsible trigger. In humans, however, despite major advances in molecular biology and the science of reproduction, there is still much that is not known about the physiological processes involved in the initiation of labour. Any proposed mechanism must therefore be considered to be a hypothesis. It seems that there is a balance between pro-pregnancy factors and pro-labour factors (Box 40.1), the pro-pregnancy factors promoting pregnancy continuation and the pro-labour factors stimulating the onset of labour. Labour may be triggered when the pro-pregnancy factors become overwhelmed by increasing levels of the pro-labour factors, although why this should occur at one particular point remains uncertain. There is some limited evidence that the human fetus may play a role in regulating this balance, but the mother also has a role. Progesterone is derived from the corpus luteum for the first 8 weeks or so of pregnancy and thereafter from the placenta. It has the direct effect of decreasing uterine oxytocin receptor sensitivity and therefore promotes uterine smooth muscle relaxation. That it plays a significant pro-pregnancy role is illustrated by the fact that the progesterone antagonist mifepristone increases myometrial contractility, and has been successfully used to induce labour. Nitric oxide, a highly reactive free radical, is also a pro-pregnancy factor. Some studies have observed a fall in uterine nitric oxide synthetase activity as pregnancy advances, but these findings are not confirmed in other studies. Catecholamines act directly on the myometrial cell membrane to alter contractility and beta-sympathomimetics are used as tocolytics to suppress preterm labour. The specific roles for catecholamines in physiological terms and the role of the hormone relaxin are unclear. Oxytocin, a nonapeptide from the posterior pituitary, is a potent stimulator of uterine contractility. Circulating levels, however, do not change as term approaches. Oestrogen levels do increase, and oestrogens increase oxytocin receptor expression within the uterus. This gradual rise may be mediated in part by fetal adrenocorticotrophic hormone (ACTH). Prostaglandin levels also increase prior to the onset of labour. These are synthesized from arachidonic acid by cyclo-oxygenase (COX), and COX-2 enzyme expression in the fetal membranes has been observed to double by the time labour begins. Prostaglandins promote cervical ripening and stimulate uterine contractility both directly and by upregulation of oxytocin receptors, and there is some evidence that the increased levels may be mediated by maternal corticotrophin-releasing hormone (CRH) secretion. (See also Clinical pelvic anatomy, Chapter 1.) The mechanism of labour involves effacement and then dilatation of the cervix, followed by expulsion of the fetus by uterine contraction. The lower part of the uterus is anchored to the pelvis by the transverse cervical (or cardinal) ligaments, as well as the uterosacral ligaments, allowing the shortening uterine muscle to drive the fetus downwards (Box 40.2).
Labour
Introduction
Primigravid compared with multigravid labour
Primigravida
Multigravida
Unique psychological experience
Inefficient uterine action is common, therefore labour is often longer
Uterine action is efficient and genital tract stretches more easily, therefore labour is usually shorter
The functional capacity of the pelvis is not known – cephalopelvic disproportion is a possibility
Cephalopelvic disproportion is rare. If it does occur, it is usually secondary to some serious problem
Serious injury to the child is relatively more common. The incidence of instrumental delivery is higher
Serious injury to the child is rare. Furthermore, the risk of birth injury is less when the baby is born by propulsion rather than traction
Uterus is virtually immune to rupture
There is a small risk of uterine rupture, particularly if there is a pre-existing caesarean section scar
The uterus during pregnancy
The initiation of labour
Pro-pregnancy factors
Pro-labour factors
The mechanism of normal labour and delivery
Obgyn Key
Fastest Obstetric, Gynecology and Pediatric Insight Engine