Induction with Prostaglandins
Prostaglandin E2 (PGE2) gel (normally 2 mg) is inserted into the posterior vaginal fornix. This is the best method in most nulliparous women, and in most multiparous women unless the cervix is very favourable. It either starts labour, or the ‘ripeness’ of the cervix is improved to allow amniotomy. If one dose does not increase the cervical ripeness, another may be given a minimum of 6 h later, providing there is no uterine activity; more than two doses are not helpful. Prostaglandins may be more effective if first administered in the evening.
Induction with Amniotomy ±oxytocin
The forewaters are ruptured with an instrument called an amnihook (artificial rupture of the membranes [ARM]). An oxytocin infusion is then usually started within 2 h if labour has not ensued. Oxytocin is often used alone if spontaneous rupture of the membranes has already occurred [→ p.267], although prostaglandins are as effective.
Methods of Induction
| Medical: | Prostaglandins |
| Oxytocin (after amniotomy/membrane rupture) | |
| Surgical: | Amniotomy |
Natural Induction
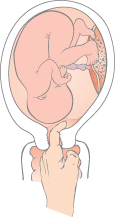
Cervical sweeping involves passing a finger through the cervix and ‘stripping’ between the membranes and the lower segment of the uterus (Fig. 30.2). At 40 weeks, this reduces the chance of induction and postdates pregnancy. However, it can be uncomfortable.
Fig. 30.2 Sweeping the membranes. A finger is inserted through the cervix and rotated: the membranes are peeled off the lower segment.
Indications for Induction
In practice, the decision to induce, and the choice of method and timing, are dependent on each individual case.
Fetal indications include high-risk situations such as prolonged pregnancy [→ p.224], suspected intrauterine growth restriction (IUGR) or compromise [→ p.217], antepartum haemorrhage, poor obstetric history and prelabour term rupture of the membranes [→ p.267].
Materno–fetal indications, where both mother and fetus should benefit, include pre-eclampsia and maternal disease such as diabetes.
Maternal indications are social reasons and in utero death.
Common Indications for Induction
Prolonged pregnancy
Suspected growth restriction
Prelabour term rupture of the membranes
Pre-eclampsia
Medical disease: hypertension and diabetes
Contraindications
Absolute contraindications include acute fetal compromise, abnormal lie, placenta praevia or pelvic obstruction such as a pelvic mass or pelvic deformity causing cephalo-pelvic disproportion. It is usually considered inappropriate after more than one Caesarean section.
Relative contraindications include one previous Caesarean section (increased scar rupture rate) and prematurity.
Management of Induced Labour
Because of both the indication for induction and the use of drugs, the fetus is at increased risk in labour. Cardiotocography (CTG) should be used for an hour, 1 h after the use of prostaglandins or when they stimulate uterine activity. Oxytocin is commonly required in labour, and also warrants CTG monitoring. Induction commonly increases the time spent in ‘early labour’, and the woman should be warned of this.
Complications
Labour may fail to start or be slow due to inefficient uterine activity. The risk of instrumental delivery or Caesarean section is higher, even allowing for the higher-risk pregnancies. Paradoxically, overactivity of the uterus can occur. This hyperstimulation is rare but causes fetal distress and even uterine rupture. The umbilical cord can prolapse [→ p.277] at amniotomy. Postpartum haemorrhage (PPH) is more likely, as is intrapartum and postpartum infection. Prematurity can follow, by accident (incorrect gestation) or design.
Labour/Vaginal Delivery After a Previous Caesarean Section
Repeat, elective Caesarean sections account for more than one-quarter of all Caesarean sections performed, yet vaginal delivery after Caesarean (VBAC) can often be safely achieved.
Contraindications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


