Site of spread
Route of spread
1. Nasal cavity and nasopharynx
Medially through sphenopalatine foramen
2. Infratemporal fossa
Laterally through pterygomaxillary fissure
3. Maxillary sinus
Anteriorly by destruction and dislocation of sinus walls
4. Pterygopalatine fossa
Through inferior orbital fissure
5. Orbit
Through inferior orbital fissure
Through medial orbital wall from ethmoid labyrinth
6. Ethmoid and sphenoid sinuses
Through natural ostia
By bony destruction
7. Middle cranial fossa
From infratemporal fossa
Through foramina (rotundum, ovale, lacerum)
By bony destruction of greater sphenoid wings and pterygoids process
Through superior orbital fissure
By destruction of wall of sphenoid sinus
8. Anterior cranial fossa
By destruction of ethmoid roof
9. Cavernous sinus and chiasmatic-sellar region
By destruction of boundaries of sphenoid sinus
JNA, in most cases, spreads through the paranasal sinuses by “pushing” of bony walls without destruction. Intracranial involvement secondary to skull base invasion is caused by local bony destruction through relentless expansion rather than cellular infiltration [11].
Blood Supply
In most cases, JNA receives the majority of its blood supply from the ipsilateral internal maxillary artery, a terminal branch of the external carotid artery [12]. The ascending pharyngeal artery and vidian artery may also contribute to the blood supply. In rare cases, the tumor is supplied by unnamed branches from the internal carotid artery. Bilateral vascular supply of a JNA is rare, but has been reported and its incidence in JNA may in fact be underappreciated [13].
Presentation
The classic presentation of JNA is an adolescent male patient (mean 15 years of age) with the following:
1.
Nasal obstruction (painless)
2.
Epistaxis (usually unilateral)
3.
Nasopharyngeal mass
Onset of JNA is most commonly in the second decade, ranging from 7 to 21 years of age. Mean age at diagnosis is 15 years of age [14, 15]. It is rare in patients older than 25 years of age. Symptoms are typically present for at least 6 to 12 months before the patient attends for assessment [14].
Advanced Disease
JNA is a slow growing tumor but extranasopharyngeal symptoms can manifest as a result of its locally destructive nature and local spread. Facial swelling, proptosis, headache, visual disturbance, and cranial nerve palsies may be signs of advanced disease [14, 15]. Rare presenting symptoms include hyponasal speech, hyposmia, hearing loss, dacrocystitis, and palatal swelling or deformity [16]. Patients with intracranial extension, secondary to tumor extension through the roof of the infratemporal fossa or via the superior orbital fissure with extension into the cavernous sinus, may present with the classic signs of superior orbital fissure syndrome, ptosis, paralysis of extraocular muscles, and exophthalmos. Intracranial spread is observed in approximately 10–20 % of all patients with JNA [11].
Differential Diagnosis
All causes of a nasopharyngeal mass, epistaxis, and orbital swelling should be included in the differential diagnosis of a JNA (Table 25.2).
Table 25.2
Differential diagnosis of JNA
Inflammatory | Antrochoanal nasal polyp |
Nasal polyposis | |
Inverting papilloma | |
Congenital/developmental | Dermoid cyst |
Encephalocele | |
Neoplastic | Rhabdomyosarcoma |
Squamous cell carcinoma | |
Lymphoma |
Diagnosis and Evaluation
Clinical history and presentation should raise suspicion for JNA. A comprehensive history and physical examination is essential in all patients.
Examination
Examination includes a thorough nasoendoscopy, which typically reveals a vascular lesion with prominent submucosal blood vessels arising along the posterolateral wall of the nasal cavity at the sphenopalatine foramen, and frequently spreading anteriorly into the nasal cavity and posteriorly into the nasopharynx. Grossly, JNA appears sessile, lobulated, rubbery, and red-pink in appearance. It may be polypoid or pedunculated (Fig. 25.1a, b).
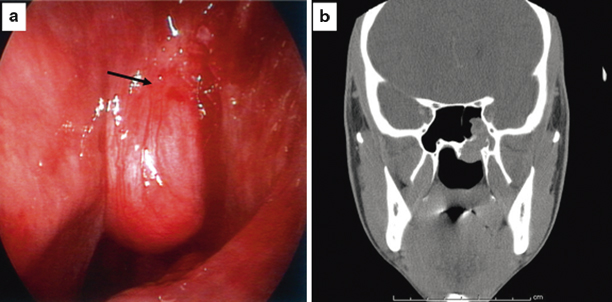
Fig. 25.1
Localized JNA . a Endoscopic image of a localized angiofibroma located at the sphenopalatine foramen in the left nasopharynx. The black arrow shows a site of pulsation consistent with the location of the sphenopalatine artery. b Coronal CT scan showing a soft tissue lesion centered on the left sphenopalatine foramen. It is extending into the left sphenoid sinus and left nasopharynx
Other clinical findings on examination may include serous otitis due to eustachian tube blockage, zygomatic swelling, and trismus, which may indicate tumor spread to the infratemporal fossa. Vision may also be decreased secondary to spread into the orbit or tenting of the optic nerve.
Imaging Evaluation
Advances in imaging techniques allow for accurate measurement of tumor, and evaluation of its localization and spread, all of which are essential to enable correct staging and appropriate surgical planning. Plain radiography images of the sinuses may show opacification, but their usefulness has essentially been surpassed by newer radiographic modalities. Computed tomography (CT) and magnetic resonance imaging (MRI) with contrast enhancement are the two most commonly utilized modalities [5]. Due to the vascular nature of JNA, angiography is also important to identify the primary vessels that feed the tumor and allow for preoperative embolization to reduce intraoperative blood loss .
CT scan is excellent for evaluation of bony erosion and extension of the tumor into the skull base. JNAs appear as hyperintense lesions on CT (Fig. 25.2a, b, c). Characteristic anterior bowing of the posterior wall of the maxillary sinus seen on CT, due to tumor in the pterygomaxillary space, is known as Holman-Miller’s sign [11].
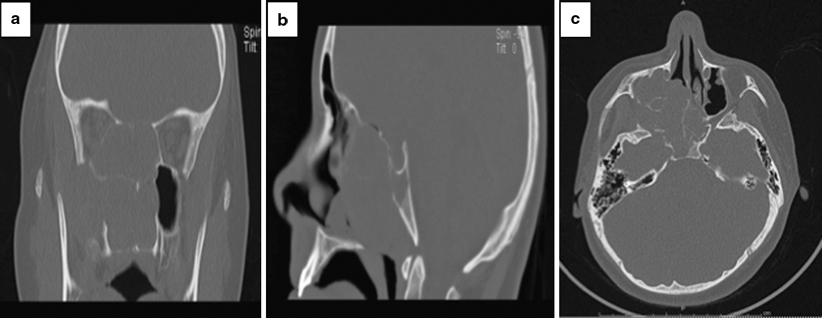
Fig. 25.2
Advanced JNA. Coronal (a), saggital (b), and axial (c) maxillofacial CT images showing a large right nasopharyngeal mass with a widened sphenopalatine foramen (a). The mass extends into the right pterygopalatine fossa with erosion of the right medial pterygoid plate (c). There is invasion of the clivus with erosion of the posterior wall of the clivus (b, c). There is erosion through the planum sphenoidale, with several foci of air at the site of cranial vault dehiscence (b)
MRI is indicated to delineate the extent of the tumor, especially in cases of intracranial involvement and extension into the cavernous sinus. MRI characteristics of JNA depend on the relative combination of vascular fibrous components and tissue edema. JNAs are markedly enhanced on contrast-enhanced T1-weighted MRI with multiple flow-related signal voids and have a lobulated appearance of variable signal intensity on T2-weighted MR images (Fig. 25.3a, b, c). MRI also enables the distinction between inssipated secretions in obstructed sinuses and tumor, which is important to prevent upstaging of the tumor.

Fig. 25.3
Advanced JNA. Coronal (a), axial (b), and saggital (c) T1-weighted maxillofacial MRI images post contrast showing a large nasopharyngeal mass with multiple flow-related signal voids (a, b). Laterally the mass extends into the right maxillary antrum and right pterygopalatine fossa (a, b). The right medial and inferior recti muscles are displaced laterally by the mass, with convex remodeling of the right orbital floor (a). There is invasion of the clivus with erosion of the posterior wall of the clivus and through the planum sphenoidale (b, c). The mass erodes the anterior right carotid canal with possible invasion of the cavernous sinus (c). There is erosion of the right vidian canal and the right foramen rotundum is expanded (b)
Angiography should be routinely performed preoperatively. The characteristic “angiographic tumor blush” of JNA identifies the branches of the internal maxillary, ascending pharyngeal, and palatine arteries supplying the tumor (Fig. 25.4a, b).
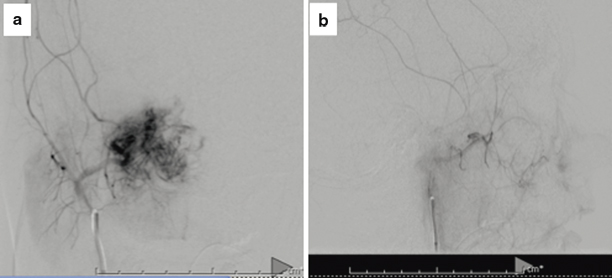
Fig. 25.4
Angiography and embolization of the right internal maxillary artery. Characteristic “tumor blush” seen in JNA following catheterization of right internal maxillary artery (a). Following selective embolization of distal right internal maxillary artery using PVA particles, there is virtually no residual tumor blush (b)
Biopsy
Biopsy is almost never required prior to surgical intervention. In most cases it is avoided due to the vascular nature of JNA and the possibility of causing severe hemorrhage . The characteristic age of the patient, clinical presentation, and imaging features usually permit a confident preoperative diagnosis of JNA to be made without the need for tissue diagnosis. Key features of JNA, including the location in the nose and pterygopalatine fossa, prominent vascularity, and pattern of bony erosion posteriorly help to distinguish JNA from other tumors found in this site including rhabdomyosarcoma and lymphoma.
Staging
There is no consensus on the ideal staging system for JNA. Several staging systems have been proposed, including those of Sessions, Andrews, Chandler, and Radkowski [17–21]. The common feature of these systems is that staging is based on tumor spread, and sites of involvement, assessed radiologically by CT and MRI. Advanced lesions are those with skull base involvement and intracranial extension. A more recent staging system, UPMC staging system, was proposed by Synderman et al. 2010, which accounts for two important prognostic factors, including tumor vascularity (the extent of vascular supply from the internal carotid artery) and route of skull base extension [22]. This newer staging system reflects changes in surgical approach, that is the increasing use of the endoscopic approach, and provides a better prediction of morbidity (blood loss) and tumor recurrence (Table 25.3).
Table 25.3
Staging systems for JNA
Stage | |||||
|---|---|---|---|---|---|
System | I | II | III | IV | V |
Sessions et al. 1981 | Ia: limited to nose and nasopharynx | IIa: minimal extension into pterygomaxillary fossa | Intracranial extension | NA | |
Ib: extension into ≥ 1 sinus | IIb: full occupation of pterygomaxillary fossas with or without orbital involvement | ||||
IIIc: extension into infratemporal fossa with or without cheek extension | |||||
Chandler et al. 1984 | Limited to nasopharynx | Extension into nasal cavity or sphenoid sinus | Extension into maxillary antrum, ethmoid sinus, pterygomaxillary fossa, infratemporal fossa, orbit, and/or cheek | Intracranial extension | |
Andrews et al. 1989 | Limited to nasopharynx; limited to sphenopalatine foramen; no bone destruction | Invading sphenoid, ethmoid, maxillary sinus or pterygopalatine fossa with bony destruction | Invading infratemporal fossa or orbit; | Intracranial, intradural extension; | |
IIIa: no intracranial extension | IVa: with cavernous sinus, pituitary or optic chiasm infiltration | ||||
IIIb: extradural extension | IVb: without cavernous sinus, pituitary or optic chiasm infiltration | ||||
Radkowski et al. 1996 | Ia: limited to nose or nasopharynx | IIa: extension through sphenopalatine foramen and into pterygomaxillary fossa | Erosion of skull base: | NA | |
Ib: extension into ≥ 1 sinus
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||