Fig. 1
Images of a 2.5 year old boy. (a) Sagittal view of CT scan showing craniovertebral instability. (b) Axial view of arch of atlas showing its trifid nature. (c) T2-weighted MRI in neutral position showing cord changes suggesting evidence of injury. (d) Lateral X-ray with the head in flexion showing atlantoaxial dislocation. (e) X-ray with the head in extension showing reduction of the dislocation. (f) Postoperative scan showing fixation in reduced position. (g) Axial images showing screws in the lateral mass of the axis. (h) Sagittal image showing lateral mass plate and screw fixation. Images of 6-year-old boy
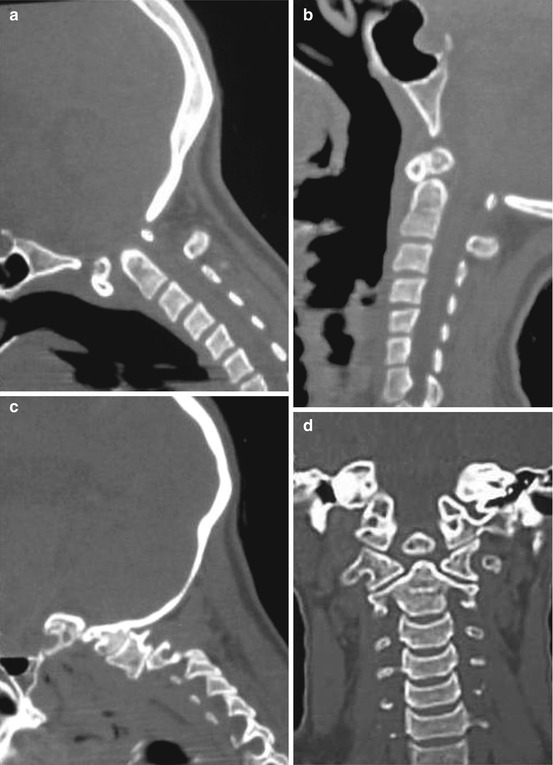

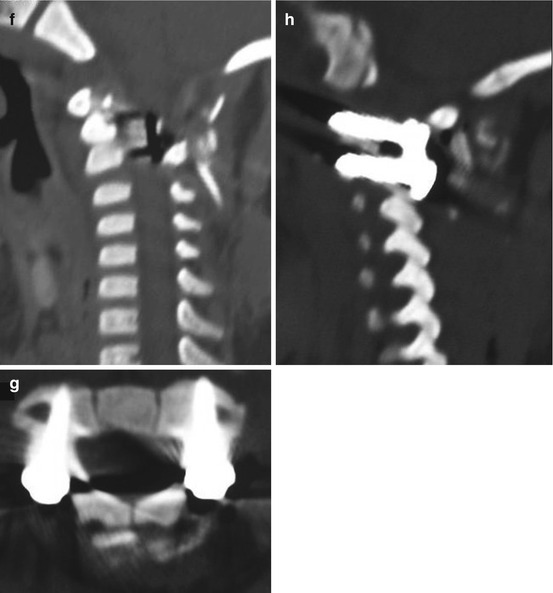
Fig. 2
(a) Sagittal image showing atlantoaxial dislocation. There is os odontoideum. (b) CT scan with head in extension showing reduction of dislocation. (c) Lateral view of sagittal image showing listhesis of facet of C1 over facet of C2. (d) Coronal image showing the craniovertebral junction. Os odontoideum is distinctly seen. (e) T2-weighted MRI showing the compression of the cord. (f) Postoperative scan showing reduction of dislocation. (g) Image showing plate and screw fixation of the facets
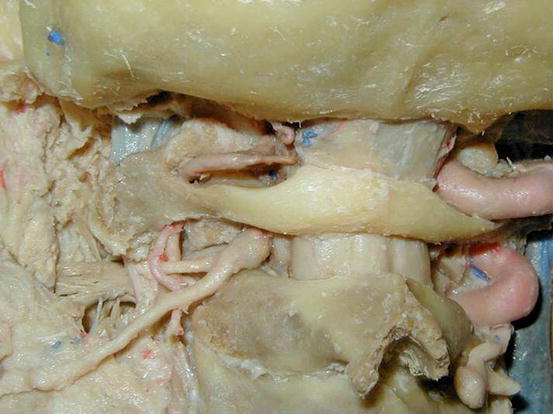
Fig. 3
Cadaver dissection picture is shown. Note the relationship of the C2 ganglion with the atlantoaxial joint. Also note the hypoplastic vertebral artery on the left side and the dominant vertebral artery on the right side
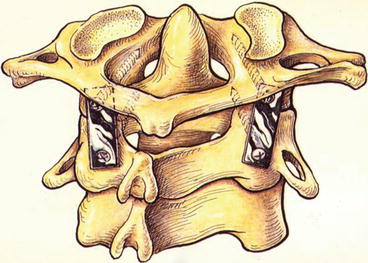
Fig. 4
Line drawing showing plate and screw fixation of the atlantoaxial joint. Screws are inserted into the facets of the atlas and facets of axis. The C2 ganglion is sectioned, joint cavity is opened, articular surface is denuded, bone graft is inserted into the cavity, and subsequently plate and screw fixation is done
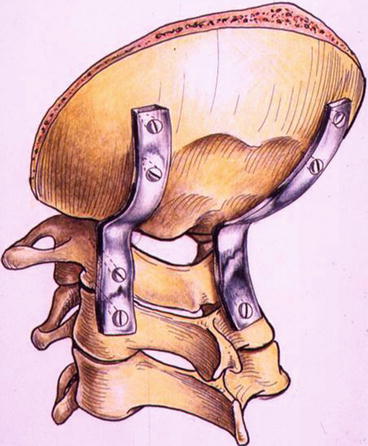
Fig. 5
Line drawing showing occipitocervical fixation. The occipital end of the plate is fixed with occipital screws, and the cervical end of the plate is fixed with screws inserted into facets of C2 alone and into facets of C1 and C2
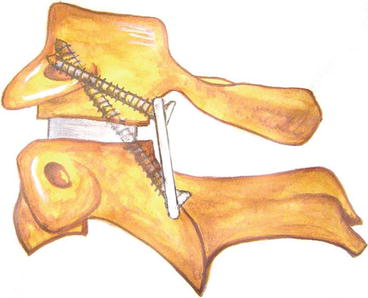
Fig. 6
Line drawing showing ‘double insurance’ atlantoaxial fixation. The C1 screw is inserted directly into the facet of atlas, whilst C2 screw is inserted in a transarticular fashion
Atlantoaxial dislocation can be due to a number of etiological factors. The dislocation can be of mobile and reducible type or of a ‘fixed’ or irreducible type. In the more common form of AAD, the atlas dislocates over the axis. In cases with occipitalisation of the atlas, the head and atlas form one unit, and the axis and the rest of the spine form the other unit. The odontoid process of the axis is normally in close approximation with the anterior arch of the atlas. In AAD, the head and atlas dislocate ventrally on the axis on flexion of the head, markedly widening the atlantodental interval and reducing the diameter of the spinal canal, with consequent pressure on the cervicomedullary junction cord. The dislocation increases on flexion of the head and reduces in extension in the mobile variety of AAD. In the fixed or irreducible variety, the dislocation persists entirely or at least partially on full extension of the head. In our recent analysis we identified that atlantoaxial dislocation is very rarely of fixed or irreducible variety and can almost always be reduced by direct manipulation and distraction of the facets [14, 18].
Mobile and Reducible Atlantoaxial Dislocation
In the year 2001, we analysed 160 cases with mobile and reducible atlantoaxial dislocation treated in our department [18]. Whilst trauma leads to mechanical disruption of ligaments of the region, in ‘congenital’ dislocation, laxity or incompetence of the ligaments is more often the cause. In several cases, the exact differentiation between a congenital and acquired cause is difficult to decipher. The range of mobility of the dislocation is in general significantly higher in cases with congenital dislocation than in cases with trauma-related dislocation. Children usually tolerate dislocation better and symptoms may be subtle and long-standing. In children, the dislocation is usually reducible.
Symptoms
Pain in the upper part of the neck and restriction of neck movements are common symptoms. The patient may give a history of an injury that flexed the head and neck (as when he is hit on the back of the head) as the precipitating factor. Weakness and spasticity of all limbs can follow the event of trauma. A range of motor and sensory deficits can occur. The sensory deficits are relatively less severe. Severe injuries to the cervicomedullary cord may produce respiratory paralysis, coma and even death. The tissues are more supple and stronger in children and traumatic dislocations are relatively uncommon. However, pre-existing muscle/ligament disorder can lead to atlantoaxial dislocation.
Investigations
Radiographs showing the lateral views of the atlantoaxial region with the head and neck flexed and extended are always done. The atlantodental interval of less than 3 mm is generally considered within the normal range in infants and children in Group A and Group B. The atlantodental interval of more than 3 mm usually confirms the diagnosis. Dynamic CT scan with appropriate reconstruction images shows the dislocation clearly. MR showing signal alterations are important and frequently confirmatory evidence indicating compression of the cervicomedullary cord. MR and CT angiography can show the relationship of the vertebral artery to the facets of C2 and C1. Such information is crucial when lateral mass fixation techniques are employed for surgery. MRI provides useful information regarding the nature of soft tissue alterations. The status of bones in general and of facets in particular should be elaborately evaluated on investigations.
Treatment
The treatment of patients with atlantoaxial instability is a surgical challenge, and achieving a successful outcome for these patients is gratifying. The complications of surgery, however, are potentially lethal. Various methods of fixation have been described and used successfully in the treatment of patients with atlantoaxial instability. The techniques of craniovertebral fixation evolved during the twentieth century as the anatomy and biomechanics of the craniovertebral region became clearer. The aim of surgery in general is to restore normal or the best possible alignment and to achieve stability of the atlantoaxial joint. The techniques of fixation for atlantoaxial dislocation can be divided into midline procedures that involve the fixation of arch of the atlas with the lamina of axis and lateral mass fixation procedures. Midline methods of fixation include sublaminar wire fixation and metal loop fixation. Metal implants and fixation methods provide an initial period of fixation of the region facilitating bony fusion. Bony fusion takes about 3 months, and the metal implants should be strong enough to hold the region for that period. It ultimately depends on bony fusion to provide stability to the region. Bone harvested from the patient’s own iliac crest has been identified by several authors to be superior to any other form of bone graft or artificial material [34]. Compromise on using the type of bone graft can lead to inadequate fusion, a phenomenon that can mar the entire operative procedure. Multiple pieces of corticocancellous bone graft should be placed in the craniovertebral region after elaborately preparing the host bone. The movements in the atlantoaxial region occur in atlantoaxial joint. Any method of stabilisation that directly fixes the joint and the fixation is segmental in nature, having superiority over methods that employ fixation remote to the site of maximum movements and those that attempt to fix multiple bone segments [29]. The lateral mass fixation techniques have been identified to be philosophically superior and biomechanically stronger to the techniques that involve fixation of the midline structures like lamina and arch of atlas (Fig. 4). In children with multiple joint ligamental laxity, occipitocervical fixation may sometimes be necessary. Methods incorporating screw fixation of the occipital end of the implant and inclusion of C1 and C2 facets by screw fixation were first described by us [14] (Fig. 5).
Irreducible or Fixed Atlantoaxial Dislocation
The issue of ‘irreducible’ or ‘fixed’ atlantoaxial dislocation has been under discussion for a long time. On the basis of our analysis we have concluded that atlantoaxial dislocation is only rarely fixed and can be manually distracted and reduced [23]. The joint is usually active and functional when a joint space is evident of CT scanning and the articular surfaces are smooth and well defined even when they are not in alignment. Direct distraction of facets of atlas and axis and placement of bone graft within it, with or without additional support of metallic spacers, can result in significant or complete reduction of dislocation. Subsequent atlantoaxial fixation that can sustain the reduction is then carried out. The mechanism of the screw tightening can also be modified and can simulate the technique used in the treatment of spondylolisthesis [23, 42]. The C2 screw is tightened first completely and subsequently the C1 screw is tightened. Such a technique assists in pulling the C1 back into alignment. Transoral decompression of the odontoid process followed by posterior fixation is also a useful method of treatment, particularly when the surgeon is not familiar with lateral mass fixation and distraction procedures.
Basilar Invagination (Figs. 7, 8, 9, and 10)
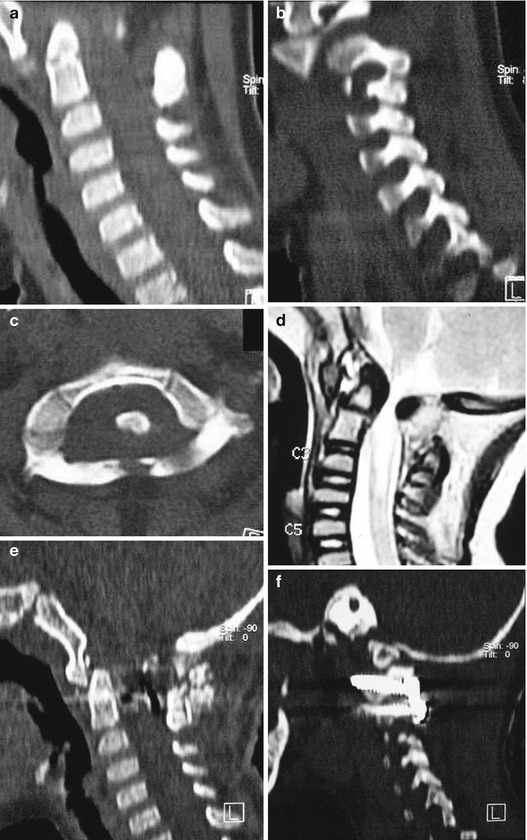
Fig. 7
Images of a 4-year-old boy. (a) Sagittal image of CT scan showing basilar invagination. (b) CT scan showing listhesis of facet of C1 over the facet of C2. (c) Axial view of CT scan showing the atlas bone in multiple segments. (d) T2-weighted MRI showing basilar invagination and cord compression. (e) Postoperative image showing reduction of the basilar invagination. There is craniovertebral realignment without any bone decompression. (f) Lateral sagittal view showing plate and screw fixation of the facets
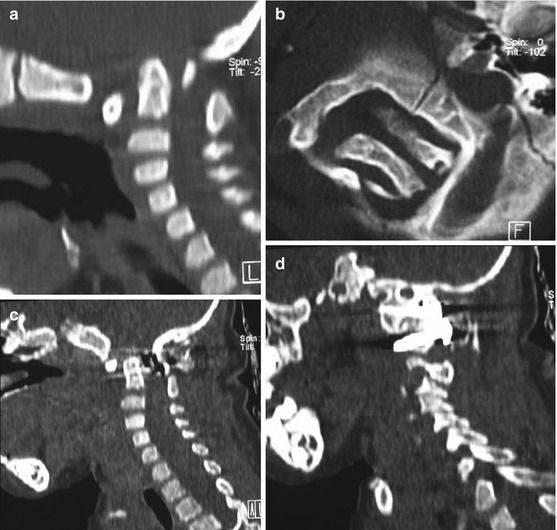
Fig. 8
Images of a 4-year-old girl. (a) Sagittal image of CT scan showing a complex craniovertebral anomaly with severe basilar invagination. (b) Axial CT scan image showing complex bone alignment at the craniovertebral junction. (c) Postoperative image showing craniovertebral realignment. Reduction of basilar invagination can be seen. There is no anterior or posterior bone decompression. (d) Lateral cut of sagittal image shows lateral mass plate and screw fixation
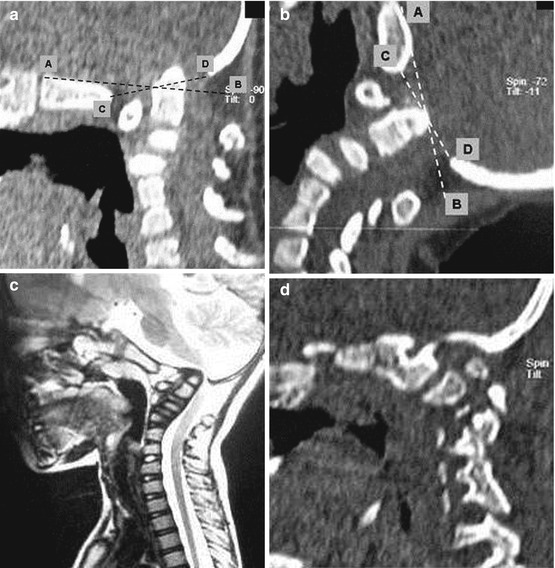
Fig. 9
(a) Sagittal image of CT scan with the head in flexed position showing basilar invagination. (b) CT scan image with the head in extension showing reduction of basilar invagination. Line A, B Wackenheim’s clival line, Line C, D McRae’s Foramen Magnum line. (c) T2-weighted MRI showing basilar invagination. (d) Image through the lateral masses showing incompetence of the facets

Fig. 10
(a) Sagittal view of CT scan with the head in flexed position showing basilar invagination. (b) View with head in extension position showing complete reduction of basilar invagination. (c) View through the facets showing their abnormal orientation. (d) Postoperative view showing reduction of basilar invagination
Basilar invagination forms a prominent component of the craniovertebral anomalies. Chiari malformation and syringomyelia are common associates of basilar invagination and are the soft tissue components of the dysgenesis. Plain radiological and tomographic parameters have been principally used to diagnose basilar invagination for many years. There has been a renewed interest in the normal anatomy and pathologic lesions of the craniovertebral junction with the development of imaging by high-resolution CT scan and MRI. Dynamic MRI and CT scan have helped in the evaluation of the pathology of basilar invagination, in the assessment of biomechanics of the joints and in the formulation of a rationale surgical strategy. Despite the clarity of imaging, controversy regarding the management of basilar invagination continues. Even the natural history has not been clearly elucidated in the literature. The surgical indications for a given approach together with the timing of the surgical stages are still under discussion.
Pathogenesis
Several theories have been suggested to elucidate the probable cause and origin of basilar invagination. Most of these theories point towards embryological dysgenesis, genetic abnormalities and viral infections [5, 26, 36, 55, 56]. Several authors, for over a century, have thought that deformation had a mechanical cause and therefore applied the name ‘impressio baseos cranii’ (Berg and Retzius is cited by Virchow 1857) [55], or basilar impression [5]. Grawitz [36] believed that basilar invagination was often a result of under- or maldevelopment of the craniovertebral transition region. A range of malformations is frequently associated with anomalies of the atlas and axis, some of which may be quite atypical, and with fissures or defects and bone projections from the spinal column in the craniovertebral transition zone. The latter anomalies were grouped together by von Torklus and Gehle as suboccipital dysplasias [56].
Basilar invagination can be secondary to abnormally inclined alignment of the facets of atlas and axis [16, 19, 42]. The progressive slippage of the atlas over the axis secondary to this malalignment, a process similar to spondylolisthesis in the lumbosacral spine, results in invagination of the odontoid process into the craniocervical cord [42]. Short neck, low hairline, web-shaped neck muscles, torticollis, reduction in the range of neck movements and several such physical variations have been described as hallmarks of basilar invagination for over a century. A number of bone fusion deformities and platybasia have also been recorded. Neck pain, muscle spasms and restriction of neck movements are frequently noted and suggest instability of the region
Classification into Groups I and II
In the year 1997, we presented a classification system for basilar invagination that divided it into two discrete categories. This classification helped in clarifying the understanding of the pathology and pathogenesis of the anomaly, in the selection of the surgical treatment and in prediction of the outcome [16]. Based on a single criterion of the absence or presence of Chiari malformation, the anomaly was classified into Groups I and II, respectively.
Essentially, Group I included cases where there was invagination of the odontoid process into the foramen magnum and it indented into the brainstem. The tip of the odontoid process distanced itself from the anterior arch of the atlas or the inferior aspect of the clivus. The distancing of the odontoid process from the anterior arch suggested the presence of instability of the region and atlantoaxial dislocation. The angle of the clivus and the posterior cranial fossa volume were essentially unaffected in these cases. In Group II, on the other hand, the assembly of odontoid process, anterior arch of the atlas and the clivus migrated superiorly in unison resulting in reduction of the posterior cranial fossa volume, which was the primary pathology in these cases. The Chiari malformation or herniation of the cerebellar tonsil was considered to be a result of reduction in the posterior cranial fossa volume. In the year 1997, Goel first defined the clinical implication of association of small posterior cranial fossa volume and Chiari malformation [16].
Classification into Groups A and B
In our recent study, we identified a subgroup of patients where there was clear radiological evidence of instability of the region that was manifested by distancing of the odontoid process away from the anterior arch of the atlas and the radiological features matching those of Group I cases. Considering this current evaluation we have proposed a new classification for basilar invagination into two groups based on parameters that determined an alternative treatment strategy [19]. In Group A basilar invagination, there was a ‘fixed’ atlantoaxial dislocation, and the tip of the odontoid process ‘invaginated’ into the foramen magnum and was above the Chamberlain’s line [5], McRae’s line of foramen magnum [47] and Wackenheim’s clival line [54]. The definition of basilar invagination of prolapse of the cervical spine into the base of the skull, as suggested by von Torklus [56], was suitable for this group of patients. Group B basilar invagination was where the odontoid process and clivus remained anatomically aligned despite the presence of basilar invagination and other associated anomalies. In this group, the tip of the odontoid process was above the Chamberlain’s line but below the McRae’s and the Wackenheim’s lines. The radiological findings suggested that the odontoid process in Group A patients resulted in direct compression of the brainstem. Essentially, in Group A basilar invagination, the pathogenesis appeared to be mechanical instability of the region that was manifested by the tip of the odontoid process distancing itself from the anterior arch of the atlas or the lower end of the clivus. In some Group A patients, there was Chiari malformation, and this feature differentiates the present classification from the earlier classification. In this group, the atlantoaxial joints were ‘active’, and their orientation was oblique as shown in the figure, instead of the normally found horizontal orientation. Similarities of such a position of the C1–2 facets with spondylolisthesis seen in the subaxial spine can be seen. It appears that the atlantoaxial joint in such cases is in an abnormal position, and progressive worsening of the dislocation is probably secondary to increasing ‘slippage’ of the facets of atlas over the facets of axis. In Group B, the pathogenesis appeared to be congenital dysgenesis, and atlantoaxial joints were normally aligned or were entirely fused. The pathogenesis of basilar invagination appears to be different in the two groups. Understanding of these two types of basilar invagination is crucial in understanding the various involved management issues.
Diagnosis
Radiological Criteria
(a)
Chamberlain’s line: Basilar invagination was diagnosed when the tip of the odontoid process was at least 2 mm above the Chamberlain’s line [5]. Measurement of Chamberlain’s line on lateral sagittal reconstruction pictures of CT scan and sagittal MRI was seen to be reliable and accurate. The analysis of basilar invagination in the two groups on the basis of Chamberlain’s line suggested that the basilar invagination is much more severe in Group B than in Group A.
(b)
Distance between the odontoid tip and the pontomedullary junction: The distance of the tip of the odontoid from the pontomedullary junction, as observed on MRI, is a useful index to define the reduction of the posterior cranial fossa bone size [16]. The distance was markedly reduced in Group B cases, whilst it was relatively large in Group A cases.
(c)
Atlantodental or clivo–dental interval: In Group A cases, it was seen that the odontoid process migrated superiorly and posteriorly into the foramen magnum and distanced itself from the anterior arch of the atlas and the inferior end of the clivus. As judged from the atlantodental or clivo-dental interval, there was an element of ‘fixed’ atlantoaxial dislocation in these cases. Actual mobility of the atlantoaxial joint on flexion and extension of the neck can be infrequently demonstrated with a good quality imaging. In Group B the alignment of the odontoid process with the anterior arch of the atlas and with the inferior aspect of the clivus remains normal and there is no instability.
(d)
Vertical mobile and reducible atlantoaxial dislocation: There was basilar invagination when the neck was flexed, and the alignment was normal when the head was in extended position [27]. Although such mobility is only rarely identified, it does indicate the need for dynamic flexion–extension studies to preoperatively assess the craniovertebral instability. Vertical dislocation is due to incompetence of the atlantoaxial joint and lateral masses.
(e)
Wackenheim’s clival line: Wackenheim’s clival line is a line drawn along the clivus. The tip of the odontoid process was significantly superior to the Wackenheim’s clival line in Group A cases. In Group B cases, the relationship of the tip of the odontoid process and the lower end of the clivus and the atlantodental and clivo-dental interval remained relatively normal. In a majority of these cases, the tip of the odontoid process remained below the Wackenheim’s clival line [54] and McRae’s line of the foramen magnum [47]. The basilar invagination thus resulted from the rostral positioning of the plane of the foramen magnum in relation to the brainstem.
(f)
Platybasia: A line is drawn along the anterior skull base. The angle of this line to the clivus is referred to as the basal angle. Reduction of the basal angle is referred to as platybasia. Posterior cranial fossa volume: The Klaus’ height index [56] measured on the MRI was seen to be much more accurate than the conventional measurements based on plain X-rays. The tentorium could be clearly identified on MRI, and the distance of the tip of the odontoid from the line of the tentorium indicated the height of the posterior cranial fossa. On the basis of Klaus’ index, the posterior fossa height was found to be markedly reduced in Group B cases, whilst it was only moderately affected in Group A cases.
(g)
Omega angle: Although not frequently used, the omega angle or the angulation of the odontoid process from the vertical as described by Klaus was found to be a useful guide [56]. We described a modified omega angle as the measurement of the angle from the vertical was affected by the flexion and extension of the neck [16]. A line was drawn traversing through the centre of the base of the axis parallel to the line of the hard palate. The line of the hard palate was unaffected by the relative movement of the head and the cervical spine during the movement of the neck in these ‘fixed’ craniovertebral anomalies. Facial hypoplasia or hard palate abnormality was not seen in any case in this series and did not affect the measurements. The omega angle depicted the direction of displacement of the odontoid process. The omega angle was severely reduced in Group A cases, whilst it was much larger in Group B cases. The reduction in the omega angle in Group A cases depicted that the odontoid process had tilted towards the horizontal and was posteriorly angulated in Group A cases, whilst it was near vertical and superiorly migrated in Group B cases.
(h)
Brainstem girth: The effective brainstem girth measured on MRI was a useful additional parameter. Whilst the brainstem girth was markedly reduced in Group A cases, the girth was only marginally affected or unaffected in Group B cases indicating thereby that there was no direct brainstem compression as a result of the odontoid process in the latter group.
(i)
Neck size: Measurement of craniovertebral height can be done using a modification of Klaus’ posterior fossa height index [26]. The cervical height was measured from the tip of the odontoid process to the midpoint of the base of the C7 vertebral body.
(j)
Direct physical measurement of the neck length: It can be a useful parameter. The parameter of direct physical measurement of the neck length from the inion to the tip of the C7 spinous process can be useful [26].
Clinical Features
Majority of patients with Group A basilar invagination (58 %) had a history of minor to major head injury prior to the onset of the symptoms [19]. The pyramidal symptoms formed a dominant component. Kinaesthetic sensations were affected in 55 % cases. Spinothalamic dysfunction was less frequent (36 %). Neck pain as a major presenting symptom was in 77 % cases. Torticollis was present in 41 % cases. The analysis of radiological and clinical features suggests that the symptoms and signs were a result of brainstem compression by the odontoid process.
The presentation was relatively acute in Group A cases, whilst it was long-standing and slowly progressive in Group B cases. In Group B cases, the onset of symptoms and their evolution were insidious. Thus, a careful inquiry was needed to pinpoint the timing of appearance of the initial symptoms. In the majority of cases, the time of onset was already forgotten. This made it difficult to establish with certainty the age at which the complaints began. The symptoms and signs in Group B basilar invagination appeared to be directly related to the ‘crowding’ of neural structures at the foramen magnum. Although the dimensions of the foramen magnum were large and sometimes larger than even in a normal state, the volume of its contents and probably the ‘pulsatile’ compression of the structures at the foramen magnum resulted in neurological symptoms. The markedly reduced girth of the brainstem in Group A cases clearly showed that direct compression of the brainstem by the odontoid process caused the neurological symptoms. Central cord symptoms and related signs were noted in cases associated with syringomyelia.
Occipitalisation of the atlas: Occipitalisation of the atlas associated with basilar invagination was noted first by Rakitansky [cited by Grawitz [36]] and has since been referred to frequently [36, 47, 54, 55]. Many authors have regarded assimilation as a characteristic feature of basilar invagination. The assimilation of atlas can be partial or incomplete.
Klippel–Feil bone anomaly refers to the triad of observations of extensive cervical vertebral fusions, low hairline, restrictions of neck movements and a short neck.
Trauma of varying severity was a noteworthy precipitating factor in Group A cases [19]. Trauma seldom plays any major role in precipitating the symptoms in Group B cases. The fact that trauma influenced the acute development of symptoms pointed towards an element of instability of the craniovertebral region in Group A patients.
Age factor: Basilar invagination Group A is more often seen in younger patient group, whilst Group B basilar invagination is more frequently encountered in older patient group.
Surgical Management
Craniovertebral Realignment for Group A Basilar Invagination
The conventional form of treatment of Group A basilar invagination is a transoral decompression that is followed by posterior occipitocervical fixation. However, the long-term clinical outcome following the twin operation of transoral decompression followed by posterior stabilisation was seen to be inferior to the clinical outcome following surgery that involves craniovertebral realignment without any bone, dural or neural decompression [15, 16, 19, 27].
The technique of craniovertebral realignment by wide removal of atlantoaxial joint capsule and articular cartilage by drilling and subsequent distraction of the joint by manual manipulation provided a unique opportunity to obtain reduction of the basilar invagination and of atlantoaxial dislocation.
Technique of Facetal Distraction and Craniovertebral Realignment
This operation is suitable for patients with Group A basilar invagination. The exposure of the atlantoaxial joint in cases with basilar invagination is significantly more difficult and technically challenging when compared to a normally aligned atlantoaxial joint encountered during the treatment of posttraumatic instability. The joint is significantly rostral in location and the microscope needs to be appropriately angled. The atlantoaxial facet joints are widely exposed on both sides after sectioning of the large C2 ganglion. The joint capsule is excised and the articular cartilage is widely removed using microdrill. The joints on both sides are distracted using an osteotome. The flat edge of the osteotome is introduced into the joint and it is then turned vertical to effect distraction. The status of the dislocation and of basilar invagination is evaluated by intraoperative radiographic control. Corticocancellous bone graft harvested from the iliac crest is stuffed into the joint in small pieces. Specially designed titanium spacers are used in selected cases as strut graft and impacted into the joints to provide additional distraction and stability. Over the period of our experience, we have realised that bone graft introduction inside the joint cavity and subsequent fixation can suffice, and there is a need for metal spacer only in selected cases. Fixation of the joint with the help of interfacetal screws and a metal plate provided a biomechanically firm fixation and sustained distraction. Holes in the titanium metal spacer provided space for bone fusion. The fixation was seen to be strong enough to sustain the vertical, transverse and rotatory strains of the most mobile region of the spine. Postoperatively the traction is discontinued and the patient is placed in a four-post hard cervical collar for 3 months, and all his physical activities involving the neck are restrained during the period.
Reversibility of Musculoskeletal Changes Following Surgery
A number of bone and soft tissue anomalies are associated with basilar invagination. These include short neck, torticollis, platybasia, cervical vertebral body fusion (Klippel–Feil abnormality) including assimilation of atlas, spondylotic spinal changes and restriction of neck movements. A number of these abnormalities were seen to be reversible following decompression and stabilisation of the region [26]. Considering that several physical features associated with this group of basilar invagination are reversible, it appears that the pathogenesis in such cases may be more due to mechanical factors rather than congenital causes or embryological dysgenesis. The common teaching on the subject is that the short neck and torticollis are a result of embryological dysgenesis and effectively result in indentation of the odontoid process into the cervicomedullary cord. However, it appears that it is the cord compression due to indentation by the odontoid process that is the primary event and all the physical alterations and bony abnormalities, including the short neck and torticollis, are secondary natural protective responses that aim to reduce the stretch of the cord over the indenting odontoid process. Pain, restriction of neck movements and hyperlordosis of the neck indicate the presence of instability of the craniovertebral junction. All of these natural responses probably allow the cord a relatively stretch-free traversal over the indenting odontoid process. Reduction of the disc spaces, osteophyte formation, incomplete and complete cervical fusions and alterations in the craniospinal and cervical angulations appear to be directly related to the reduction in neck length. The reduction in the disc-space height and fusions are more prominently seen in the upper cervical vertebrae. It appears that cervical fusions and assimilation of the atlas may be related to long-standing and progressive reduction in the disc-space height.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


