Fig. 1
(a, b) Flexion/extension MRI study in a MPS IVA case, showing increased cord compression during flexion
Main features to consider in MPS are: the presence of odontoid hypoplasia, periodontoid soft tissue masses due to GAG accumulation behind the odontoid process and cartilage/fibrocartilage reactive hypertrophy compounded by hypertrophy of dura and ligamentum flavum [3], spinal canal narrowing, and spinal cord compression with/without MRI signs of cervical myelopathy (Fig. 2).
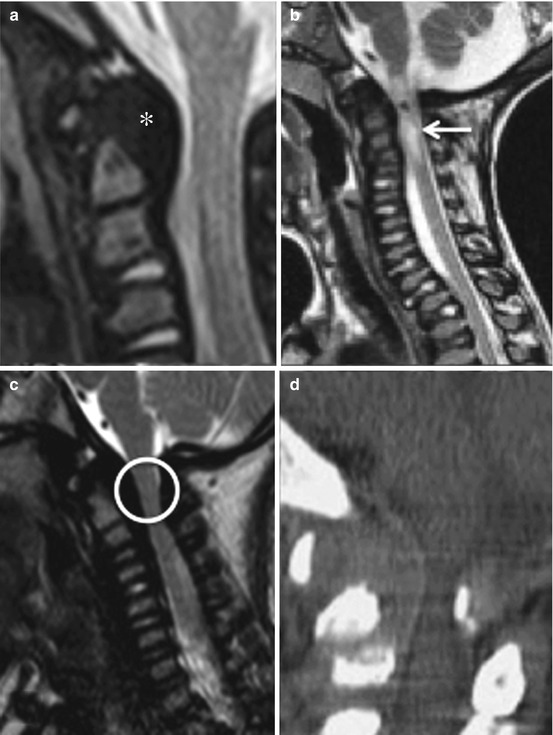
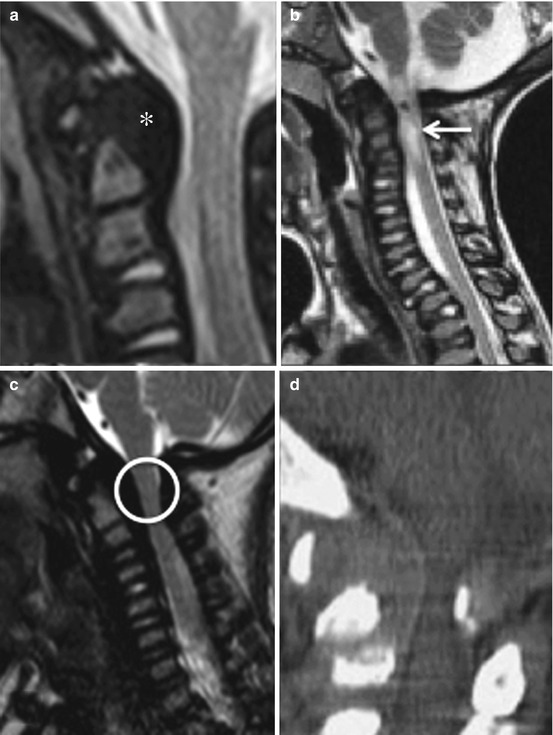
Fig. 2
MRI showing severe dens dysplasia and periodontoid tissue thickening (asterisk) in MPS II (a), acute posttraumatic myelopathy (arrow) in MPS IV (b), and severe spinal stenosis (circle) in MPS VI (c). Preoperative CT scan showing severe cord compression, dens dysplasia, and periodontoid tissue thickening in MPS IV (d)
In addition to high cervical stenosis, multilevel subaxial stenosis has been reported in MPS VI (Maroteaux-Lamy) [22]. Posteriorly protruding intervertebral discs, thickened dura, and hypertrophy of the ligamentum flavum are the most relevant features of subaxial canal narrowing [36].
We have recently reviewed radiological features of the CVJ in a consecutive series of 42 MPS patients followed at our Center for Metabolic Diseases: 12 MPS I, 15 MPS II, 2 MPS III, 9 MPS IV, and 4 MPS VI.
MRI studies have been scored according to following MRI features: dens dysplasia, periodontoid tissue thickening, spinal stenosis, myelopathy, and instability on dynamic MRIs [30].
Spinal stenosis in neutral position was classified according to the SAC scale, and the difference between the mean diameter of the subaxial cervical canal and the diameter of the cervical canal at the CVJ expressed in %. Presence or absence of signs of instability was determined by the presence or not of modifications of the SAC score and/or canal diameter during flexion/extension MRI studies at the occipitocervical junction.
CVJ abnormalities were frequent in the whole series of MPS patients, with a reduced diameter of the spinal canal at the CVJ in 17/42 children. The most severe spinal canal stenosis and cord compression were observed in MPS IV (3/9) and MPS VI (2/4). Reduction >50 % of the cervical canal diameter was observed in 5/42 patients. MRI signs of myelopathy were present in 3/42 cases, all affected by MPS IV. Dens hypoplasia was overall present in 33/42 cases and was a constant feature in MPS IV and VI. Due to the very young age of some of the children, hypoplastic dens nevertheless could still be in some case an expression of incomplete development of the C2 dens. Slight modifications of canal diameter during dynamic MRI studies were observed in 9/32 cases, confirming how clear-cut radiological signs of instability are seldom documented in MPS patients. Increased canal stenosis during dynamic MRI studies in flexion and extension was evidenced in 6/9 MPS IV patients.
These observations confirm how in Morquio’s disease severe CVJ abnormalities are more frequent and should be screened and controlled at scheduled intervals in all patients [33].
To avoid potentially harmful radiations, computed tomography (CT) scan studies of the CVJ should be reserved for children in whom MRI has evidenced significant pathological features and some surgical procedure is considered.
Fine-cut CT with coronal and sagittal 3-D reconstructions is a powerful tool for imaging the bone and clearly delineates anatomical features of C0–C1–C2 and possible associated bony abnormalities at the CVJ (Fig. 3).
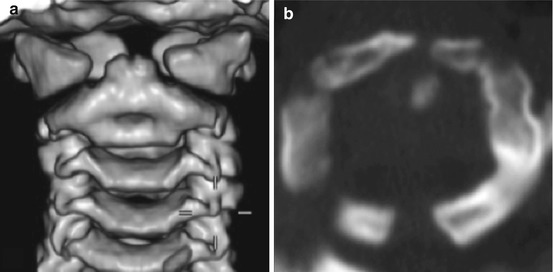
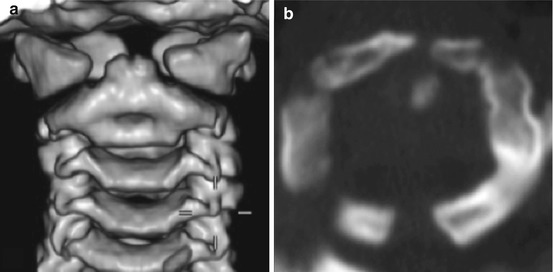
Fig. 3
3-D CT reconstruction (a) of the CVJ of a child affected by MPS VI, displaying anterior and posterior midline failure of ossification of the C1 ring; axial CT (b) showing similar features in another MPS VI case
Moreover, the dimensions of a single vertebra (height, width, length) can be easily calculated.
The recognition of heterogeneous anatomical features of the CVJ in MPS patients and the exact determination of bone geometry and diameters is of paramount importance for the selection of the most appropriate hardware placement in tailored surgical procedures with screwing techniques. In selected cases angio-CT delineating the course of vertebral arteries may be indicated, especially if suitability of C1/C2 transarticular screws is evaluated.
Indications to Surgery
The clinical evidence of acute or progressive myelopathy associated with radiological evidence of spinal cord compression at the CVJ is a strong indication to surgery as the natural history of untreated patients is invariably characterized by increasing neurological deficits and functional impairment [1, 12, 14, 22, 25, 38, 42, 46].
Preventive surgical treatment with decompression and fusion in asymptomatic children is still a matter of debate but has been especially recommended in all individuals affected by MPS IV (Morquio) with MRI evidence of stenosis and instability at the CVJ, with canal narrowing >50 % [38, 42, 44].
In our department we recommend prophylactic surgery in asymptomatic children with severe spinal canal narrowing and complete obliteration of perimedullary subarachnoid spaces (SAC < 1 mm), 50 % or more reduction of the cervical canal at CVJ, and MRI signs of instability (spinal canal stenosis and cord compression). Whenever possible, in very small children, we suggest to await for sufficient bone maturation, operating at the age of at least 3 years, although surgery can be feasible, if clinically necessary, even at a younger age as demonstrated in a 17-month-old symptomatic boy by Dickerman and coworkers [12].
Surgical Techniques
Even if the past surgery of the CVJ in small children was considered challenging and characterized by a high incidence of postoperative neurological complications, the improvement of preoperative radiological work-ups, the accurate preoperative CT identification of individual anatomical bone features, the availability of various techniques for instrumented bone fusion, and the improvement of multidisciplinary evaluations and anesthesiological techniques in these difficult patients, often affected by multiorgan disorders, have made this surgery safe and rewarding if the associated medical problems and anesthesiological challenges are recognized and managed appropriately.
Although some authors considered simple posterior decompression of the CVJ in MPS other than Morquio when dynamic radiological studies did not clearly evidence atlantoaxial or occipito-atlantoaxial instability [26, 39], we recommend decompression and fusion in all cases. Indeed, posterior decompression alone, without fusion, can actually expose these patients to acute posttraumatic myelopathy, even following a minor trauma in flexion, as evidenced in one of our children (case 1).
Ransford et al. [42] already evidenced how odontoid dysplasia with a partially cartilaginous and softer dens, the frequent finding of incomplete anterior or posterior or both ossification of the C1 ring (Fig. 3), and ligamentous laxity can result in complex CVJ instability allowing harmful translatory movements, which may be increased by posterior decompressive surgeries without stabilization.
In fact, decompression is a partly destabilizing technique in patients with pathological ligamentous laxity, as it needs removal of the posterior ring of C1, of the thickened ligamentum flavum, and of the occipito-atlantal membrane.
Recent advances in rigid fixation technologies have enhanced the ability to achieve stable posterior cervical fusions with a variety of screwing techniques, adaptable to the individual anatomical features of these usually very small children, and they should be preferred for their superior biomechanical stability [2, 7, 8, 16, 18, 55].
C1/C2 transarticular screws, C1 lateral mass screws, C1 Olerud clamps, C2 pars screws, C2 translaminar screws, or a combination of them as anchor for occipitocervical U-loop constructs can be taken in consideration on the basis of fine-cut preoperative CT studies [2]. Iliac crest graft, or rib graft, or calvarial bone graft [5] will be used to augment posterior fixation and achieve biological bone fusions. Rigid screwing techniques have also reduced or eliminated the need for external halo orthoses and their complications [2, 10].
Although we consider segmental screw fixation in the pediatric spine superior to posterior wiring techniques and external halo orthosis, the latter techniques do not need to be completely abandoned in selected cases as they still can afford good clinical results with long-term stabilization and fusion of the CVJ, as evidenced by Visocchi [51].
Clinical Results
Recent reports of surgery of the occipitocervical junction in children, comprising small series of MPS, evidence the feasibility, safety, and stability of screwing techniques with good clinical long-term outcomes after instrumented rigid implants [14, 31, 42, 44, 46].
Also in our cases, no asymptomatic patient had new postoperative neurological deficits, and all symptomatic patients improved their Ranawat score during follow-up and maintained stable constructs and solid bone fusion on neuroimaging studies at last follow-up examination.
Case Studies
Case 1: Acute Posttraumatic Myelopathy
H.M., a 6-year-old girl with MPS IVA. She had previously undergone CVJ decompression at another institution for severe canal stenosis and mild myelopathy, with removal of the posterior arch of C1 and of the thickened atlantooccipital membrane and ligamentum flavum. After a backward fall from a child’s chair, she developed an acute quadriplegia with respiratory failure (Ranawat IIIB) and was admitted to our neurological intensive care unit. MRI showed an impressive alteration of the spinal cord signal at C0–C1 (Fig. 4a). This patient was initially stabilized with an external halo orthosis and submitted to inpatient rehabilitation for some weeks afterward. After an initial neurological improvement and cardiorespiratory stability, she underwent internal stabilization with C2 pars screws (Fig. 4b) anchored to an occipitocervical U-loop and occipito-C2 calvarial bone graft. At 4-year follow-up examination, she was able to walk with crutches (Ranawat IIIA). Radiological follow-up examinations revealed wide canal decompression and a stable construct (Fig. 4c, d).
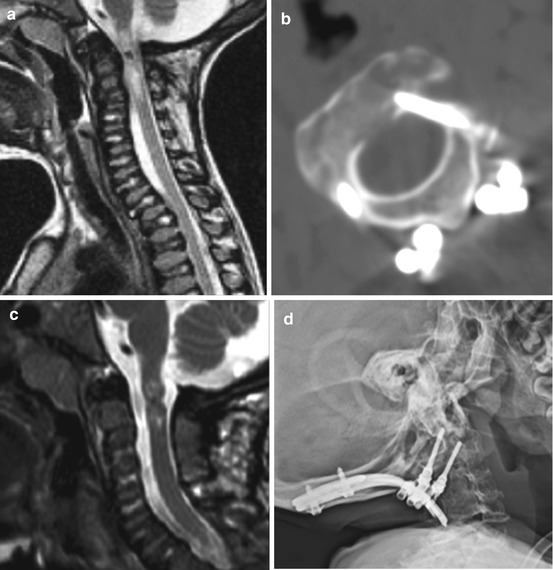
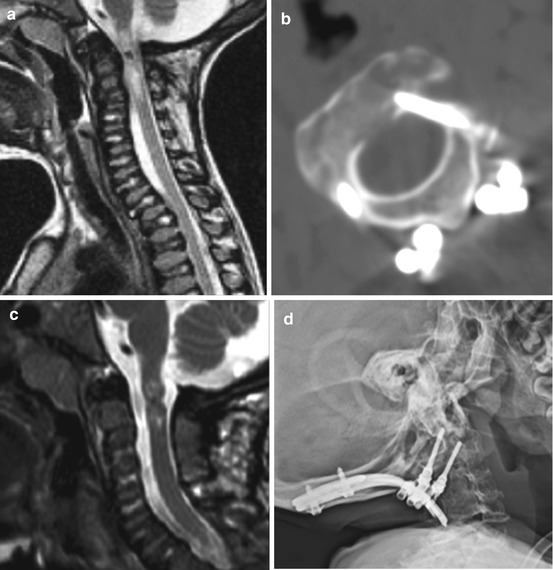
Fig. 4
(a) MRI showing severe posttraumatic myelopathy after a minor backward fall in a previously simply decompressed MPS IV child. (b) C2 pars screws, (c) postoperative MRI, and (d) plain X-rays at 4-year follow-up
Case 2: Progressive Myelopathy
R-B.G., a 6-year-old male with MPS VI. After a minor fall he experienced a transient tetraparesis with quick recovery of deambulation. In the following months he experienced repeated urinary tract infections. Cervical MRI was characterized by severe stenosis and cord compression at the CVJ with spinal cord signal alterations (Fig. 5a). Physical exam evidenced brisk tendon reflexes at all four limbs, and a urodynamic study was diagnostic for a neurological bladder. He was therefore submitted to posterior cervical decompression and internal stabilization with C2 pars screws anchored to an occipitocervical U-loop and calvarial bone graft. Postoperative course was uneventful with slow recovery of bladder function and normal daily activities. Radiological follow-up examination revealed good canal decompression, stable construct (Fig. 5b, c), and steady neurological conditions.
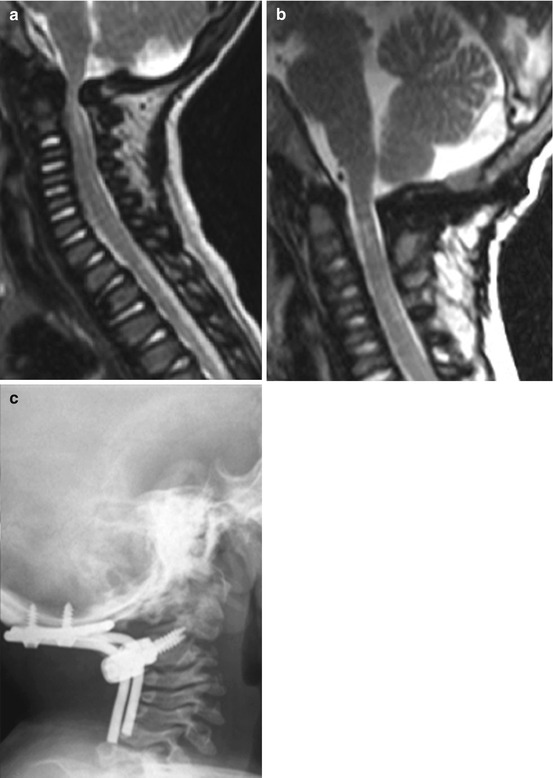
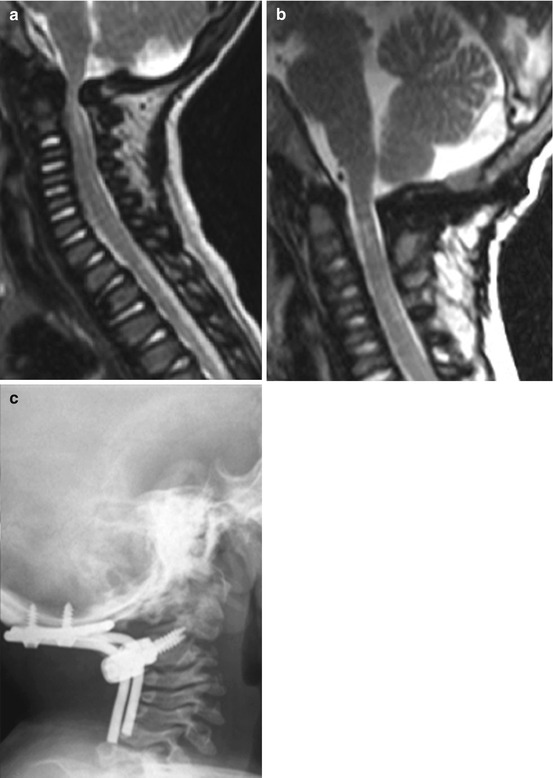
Fig. 5
(a) Preoperative MRI in a MPS VI child showing severe canal stenosis and cord compression. (b) Postoperative MRI and (c) plain X-rays showing good canal decompression and a stable construct at 2-year follow-up
Case 3: Preventive Surgery
P.M., a 2-year-old boy with MPS IVA. During routine neuroradiological work-up, severe canal stenosis at the CVJ was observed. As there were no signs of major instability and the child was completely asymptomatic with no radiological signs of myelopathy, the case was discussed with the parents and the pediatrician in charge with particular regard to the possible risk of sudden onset of neurological symptoms after trauma. Due to the small dimensions and incomplete development of bony structures at the CVJ and the increased risks of general anesthesia at that age, it was decided to schedule surgery at 3 years of age. After a follow-up MRI now evidencing increasing cord compression during flexion (Fig. 6a) and a thorough preoperative CT study, we performed preventive CVJ decompression and internal fixation with C2 laminar screws (Fig. 6b) anchored to an occipitocervical loop augmented with calvarial bone. Also in this case postoperative course was uneventful and radiological follow-up controls showed a stable construct (Fig. 6c).


Fig. 6
MRI showing severe cord compression during head flexion in MPS IVA (a), laminar screws (b), and postoperative plain X-rays at 2-year follow-up (c)
Case 4: Stabilization with Sublaminar Wires
C.V., an 8-year-old child with MPS IV. Mild canal stenosis and dens dysplasia at the CVJ (Fig. 7a, b), partial C0–C1 assimilation, and C2–C3 fusion with signs of C1/C2 instability on plain X-rays in flexion (Fig. 7c) were documented during standard neuroradiological work-up. Although the child was asymptomatic with no radiological and clinical signs of myelopathy, the radiological evidence of CVJ stenosis and instability urged us to operate the patient in order to prevent a possible neurological deterioration. CVJ decompression was associated to occipitocervical fusion with U-shaped titanium rods and sublaminar wires at C0–C3 and autologous bone harvested from the iliac crest (Fig. 7d). The patient harbored a SOMI brace system for 6 months. After a 17-year follow-up, the patient does not complain any neurological signs or symptoms or major functional impairments.
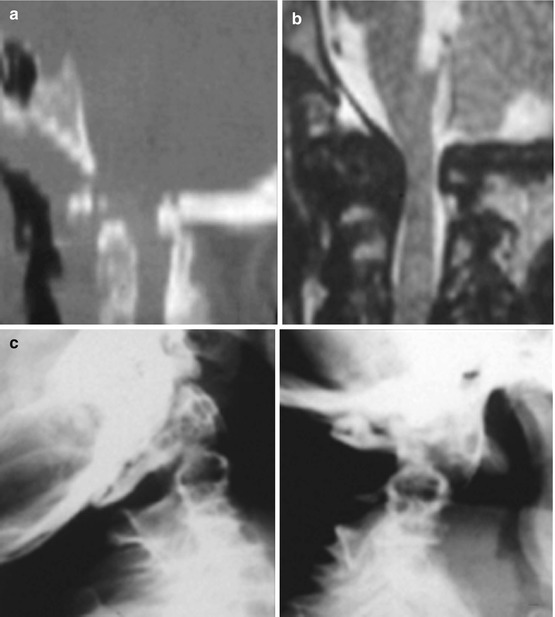

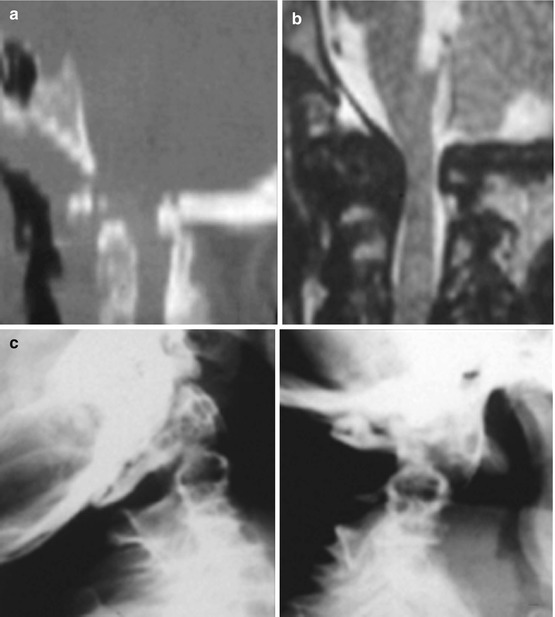

Fig. 7
(a) CT and (b) MRI showing mild canal stenosis, dens dysplasia, C0–C1 assimilation, and C2–C3 fusion. (c) Plain dynamic X-rays showing C1–C2 instability. (d) Postoperative plain X-rays
Discussion
In a database analysis of 5,300 patients with symptomatic craniovertebral abnormalities among which 2,000 were children, MPS formed only a smaller group [31].
Nonetheless, it is of paramount clinical importance to recognize early in the course of the MPS the presence or not of upper cervical stenosis, cord compression, and instability as, if unrecognized, it can severely affect the natural course of these patients already invalidated by multiorgan disorders.
ERT and HSCT may improve many of the systemic effects of some of the metabolic disorders but have unclear effects on the prevention of cervical myelopathy [22, 25]. According to Horovitz et al. [22] ERT may even increase joint mobility and cervical instability in MPS VI.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


